Abstract
Introduction
The proportion of epigastric hernias in the total collective of all operated abdominal wall hernias is 3.6–6.9%. The recently published guidelines for treatment of epigastric hernias of the European Hernia Society and the Americas Hernia Society recommend the use of a mesh for defect size of ≥ 1 cm, i.e., a preperitoneal flat mesh technique for sizes 1–4 cm, and laparoscopic IPOM technique for defects > 4 cm and/or obesity. Against that background, this analysis of data from the Herniamed Registry now aims to explore trends in epigastric hernia repair.
Methods
To detect trends, the perioperative outcome was calculated separately for the years 2010 to 2019 and the 1-year follow-up for the years 2010 to 2018 and significant differences were identified. Analysis was based on 25,518 primary elective epigastric hernia repairs. The rates of postoperative surgical complications, pain at rest, pain on exertion, chronic pain requiring treatment and recurrence associated with the various surgical techniques were calculated separately for each year. Fisher’s exact test for unadjusted analysis between years was applied with Bonferroni adjustment for multiple testing.
Results
The proportion of laparoscopic IPOM repairs declined from 26.0% in 2013 to 18.2% in 2019 (p < 0.001). Instead, the proportion of open sublay repairs rose from 16.5% to 21.8% (p < 0.001). That was also true for innovative techniques such as the EMILOS, MILOS, eTEP and preperitoneal flat mesh technique (8.3% vs 15.3%; p < 0.001). This change in indication for the various surgical techniques led to a significant improvement in the postoperative surgical complication rate (3.8% vs 1.9%; p < 0.001).
Conclusion
The trend is for epigastric hernia repair to be performed less often in laparoscopic IPOM technique and instead more often in open sublay technique or the new innovative techniques.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An epigastric hernia is defined as a defect in the linea alba between the xiphoid process and the umbilicus [1]. The prevalence of epigastric hernia is reported to be 3–5% [2]. The proportion of epigastric hernias in the total collective of all operated abdominal wall hernias is 3.6–6.9% [3, 4]. The percentage of emergency procedures due to incarceration and/or strangulation for epigastric hernias is 6.5% [5]. With a male to female ratio of 3:1, epigastric hernia is observed more commonly in men [1]. The main risk factors for epigastric hernia are extensive physical training, extensive coughing in lung disease and overweight and obesity [6]. Other potential influencing factors are smoking, chronic corticosteroid use, diabetes, old age and male gender [6].
A systematic review of epigastric hernia repair published in 2019 included only one randomized controlled trial (RCT) and seven retrospective studies [7]. That systematic review identified a lower recurrence rate for mesh use and less postoperative pain following laparoscopic repair [7]. The authors concluded that further studies of epigastric hernia repair were urgently needed.
In the meantime, two other RCTs have been published on umbilical and epigastric hernia repair [8,9,10]. In the MORPHEUS trial the preperitoneal flat mesh technique was compared with the open IPOM technique [8, 9]. Here, a significantly higher rate of early complication-related reoperations was observed for the open IPOM technique [8, 9]. No difference was seen in the recurrence rate [8, 9].
The other RCT identified improvements in the quality of life following closure of the epigastric hernia defect in laparoscopic IPOM technique [10]. No differences were found in the surgical site occurrences or the recurrence rates [10].
The recently published guidelines for treatment of epigastric hernias of the European Hernia Society and the Americas Hernia Society recommend the use of a mesh for defect size of ≥ 1 cm [11]. For defects of 1–4 cm the guidelines recommend a preperitoneal mesh technique with a 3-cm mesh overlap [11]. The laparoscopic intraperitoneal onlay mesh (IPOM) technique should only be used for defects > 4 cm and if there is a higher risk of wound complications, e.g., in obesity [11].
Against that background, this analysis of data from the Herniamed Registry now aims to present the reality in epigastric hernia repair and show trends in repair [12,13,14].
Methods
Herniamed is an internet-based hernia registry in which hospitals and independent surgeons in Germany, Austria and Switzerland can voluntarily document their routine hernia operations. A contract is made with every responsible surgeon where the latter commits to ensuring that data on the hernia operations carried out in the hospital/surgical clinics are completely and correctly entered into the Herniamed Registry. As a prerequisite for documentation in the Herniamed Registry, all patients must sign a separate consent form agreeing to their data being processed in the Herniamed Registry and indicating their acceptance of the follow-up procedure. As part of the information provided to patients regarding participation in the Herniamed Registry, they are told to inform the treating hospital or the treating clinic about any problem occurring after hernia repair. If problems occur after the hernia operation, the patient should attend the treating hospital or surgical clinic for examination [12,13,14].
All perioperative complications (bleeding, hematoma, wound-healing disorder, deep/mesh infection, and seroma) as well as complication-related reoperations are recorded for up to 30 days after surgery [12,13,14].
After 1, 5 and 10 years patients and their general practitioner are sent a questionnaire asking them about any pain at rest, pain on exertion, chronic pain requiring treatment or any protrusion in the surgical area or recurrence. If the patient or general practitioner reports a relevant finding, the patient may be requested by the treating hospital or clinic to attend for clinical examination [12,13,14].
In the current retrospective analysis, the prospectively documented data of patients who underwent routine primary elective epigastric hernia repair with the laparoscopic IPOM technique or open suture, IPOM, onlay, sublay, component separation, or “other techniques” were evaluated to determine the postoperative surgical complications, the complication related reoperations and 1-year follow-up outcomes [12,13,14].
All infrequently used alternative techniques and new procedures (EMILOS, MILOS, eTEP, preperitoneal flat mesh technique) can only be documented in the Herniamed Registry as “other techniques” [12,13,14].
To detect trends in treatment and outcome, evaluations were performed separately for the years 2010 to 2019. Since the annual number of cases in the Herniamed Registry for the years 2010 to 2012 was still relatively low, thus showing substantial variance in the results, for the postoperative outcomes the years 2013 and 2019 were compared. Similarly, for the 1-year follow-up only the years 2013 and 2018 were compared [12,13,14].
Fisher’s exact test was applied for unadjusted analysis between years using a significance level of alpha = 5%. For post hoc tests of single categories, a Bonferroni adjustment for multiple testing was implemented.
Results
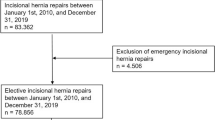
In total, 737 participating hospitals/surgical clinics entered data into the Herniamed Registry on 737,795 routine hernia repairs they had carried out between 1 January 2010 and 31 December 2019 (Fig. 1).
The proportion of epigastric hernias in the total collective of all hernias was 3.9% (n = 28,463/737,795) (Fig. 1). The gender distribution was 52% men and 48% women. 5.8% (n = 1652 / 28,463) of epigastric hernias required emergency operation (Fig. 1). 4.8% of all elective repairs (n = 1293/26,811) were reported as recurrence, although these should be considered incisional hernias.
Further analysis was undertaken with 25,518 primary elective epigastric hernia repairs (Fig. 1).
The number of epigastric hernia repairs recorded each year in the Herniamed Registry continued to rise because of the increase in the number of participating hospitals/surgical clinics (Table 1). In the total collective of all epigastric hernia repairs for the years 2010–2019, the proportion of open suture techniques was 33.4%, laparoscopic IPOM was 22.6%, open sublay 20.4%, open IPOM 9.7%, open onlay 2.8%, component separation technique 1.4%, and the proportion of “other techniques” was 9.7% (Table 2).
The distribution of the defect size based on the European Hernia Society classification [15] into small (< 2 cm), medium (≥ 2–4 cm) and large (> 4 cm) remained stable during the observation period (Fig. 2). The most recent proportion with defect size small was 45.4%, medium 38.3% and large 16.3% (Fig. 2).
The surgical techniques used in epigastric hernia repair changed highly significantly when comparing 2013 with 2019 (p < 0.0001) (Fig. 3). This is due to a significant reduction in the proportion of laparoscopic IPOM repairs from 26.0% in 2013 to 18.2% in 2019 (p < 0.0001) (Fig. 3). By contrast, the open sublay technique (16.5% vs 21.8%; p < 0.001) and the “other techniques”, with EMILOS, MILOS, eTEP, preperitoneal flat mesh technique, etc. (8.3% vs 15.3%; p < 0.001), were used significantly more often.
The relatively large proportion of open suture techniques remained unchanged between 2013 and 2019 (Fig. 3). That was also true for the open IPOM technique (Fig. 3).
Encouragingly, changes in indication for the various surgical techniques also led to a reduction in the postoperative surgical complication rate (3.8% vs 1.9%; p < 0.0001) (Fig. 4). That was really due to a corresponding drop in the postoperative surgical complication rates associated with the laparoscopic IPOM and open sublay technique (Fig. 4). However, no change was seen in the complication-related reoperation rates (Fig. 5). Changes in the surgical techniques used for epigastric hernia repair did not significantly impact outcomes at 1-year follow-up (Figs. 6, 7, 8, 9).
Relevant pain rates were identified for the total collective (Figs. 6, 7, 8). Between 2013 and 2019, the rates for pain at rest were 4.2–4.3%, for pain on exertion 9.0–9.6% and for chronic pain requiring treatment 3.1–3.7% (Figs. 6, 7, 8). The pain rates for laparoscopic IPOM reached values higher than the mean value calculated for the total collective for the years 2013 and 2018 (Figs. 6, 7, 8).
With mean values of 2.8–3.4%, the recurrence rates at 1-year follow-up reached particularly high values for the open onlay technique at 7.5% in 2013 and 9.1% in 2018 (Fig. 9). Likewise, for the open suture technique, rates of 5.1% in 2013 and 3.5% in 2018 were above those seen for the mesh techniques with the exception of the open onlay technique (Fig. 9).
Discussion
In concordance with the literature, the proportion of epigastric hernias among all hernia repairs in the Herniamed Registry is 3.9% [3, 4]. The male to female ratio for operated epigastric hernias is 52–48%. This is in contradiction to the literature data showing a preponderance of men with a ratio of 3:1 [1]. A male to female ratio of 1:1 was identified in other clinical series, too [16].
As in the literature, a relatively high proportion of emergency epigastric hernia repairs was also detected in the Herniamed Registry at 5.8% [5].
This trend analysis of the surgical techniques demonstrates a highly significant change between 2013 and 2019. During the same period there was no `significant difference in the distribution of defect sizes as defined by the European Hernia Society classification.
The proportion of laparoscopic IPOM in epigastric hernia repair declined between 2013 and 2019 from 26.0% to 18.2% (p < 0.001). Instead, the open sublay operation and the “other techniques”, including the new innovative techniques such as EMILOS, MILOS, eTEP, preperitoneal flat mesh technique, were indicated more often. A similar trend away from laparoscopic IPOM to the open sublay technique and “other techniques” was observed for incisional hernia [17]. This can be explained by the increasing reservations expressed by experienced hernia surgeons about intraperitoneal mesh placement, which can potentially result in severe complications [18, 19].
Indeed, this change in the surgical techniques used for epigastric hernia repair led to a reduction in the postoperative surgical complications, but without changing the complication-related reoperation rates. Hence, this change in indication for the laparoscopic IPOM and open sublay techniques appears to have helped improve the perioperative outcome. This confirms a critical indication for use of the laparoscopic IPOM technique [18, 19].
Another critical aspect of using laparoscopic IPOM for epigastric hernia repair is the relatively high rates of pain at rest, pain on exertion and chronic pain requiring treatment. The pain rates identified in the years 2013 and 2018 for the laparoscopic IPOM reached values higher than the mean value recorded for all epigastric hernia repairs in this registry analysis. Unfortunately, no comparable data are reported in the literature [7]. One RCT that compared laparoscopic ventral hernia repair with and without defect closure also identified high rates of chronic pain [10].
The highest recurrence rates at 1-year follow-up were identified for the open onlay technique. Accordingly, the guidelines do not recommend the open onlay technique for epigastric hernia repair [11].
Several analyses from the Danish Ventral Hernia Database demonstrated that the suture technique was associated with significantly higher recurrence rates compared with the mesh techniques [20, 21]. Similarly, in this present Herniamed Registry analysis, the recurrence rates for the years 2013 and 2018 for suture repair are above the mean values obtained for the total collective and concord with the findings of the Danish Ventral Hernia Database (20/21).
The limitations of this analysis of trends in epigastric hernia repair derive from the inability to take account of potential influencing factors, apart from the surgical techniques, on the outcome. Another limitation is the loss to follow-up for around one-fifth of all patients. Furthermore, it was possible to summarize rarely performed and innovative new techniques only as a single group denominated as “other techniques”. Despite this, the present analysis does provide important insights into the reality in epigastric hernia repair.
In summary, this trend analysis demonstrates that the proportion of laparoscopic IPOM techniques in epigastric hernia repair has declined highly significantly. Instead, open sublay repairs and other techniques as well as new, innovative techniques are being increasingly used in recent times. This changeover has led to a significant reduction in the postoperative surgical complications. Relatively high chronic pain rates have been identified for the laparoscopic IPOM. The open onlay technique has a very high recurrence rate. Mesh procedures have lower recurrence rates than suture repair.
References
Fitzgibbons, Jr. RJ (2002) Greenburg AG 35B Epigastric Hernia; Page 398–404 in: Nyhus & Condon’s-Hernia, Fifth Edition by Lippincott Williams & Wilkins
Ponten JEH, Thomassen I (2014) Nienhuijs SW A Collective Review on Mesh-Based Repair of Umbilical and Epigastric Hernias. Indian J Surg 76:371–377. https://doi.org/10.1007/s12262-013-0920-6
Statistisches Bundesamt (Destatis) (2019) Artikelnummer: 5231401197014
Rutkow IM (2003) Demographic and socioeconomic aspects of hernia repair in the United States in 2003. Surg Clin North Am. 83:1045–1051. https://doi.org/10.1016/S0039-6109(03)00132-4
Helgstrand F, Rosenberg J, Kehlet H, Bisgaard T (2013) Outcomes after emergency versus elective ventral hernia repair: a prospective nationwide study. World J Surg 37:2273–2279. https://doi.org/10.1007/s00268-013-2123-5
Ponten JE, Somers KY, Nienhuijs SW (2012) Pathogenesis of the epigastric hernia. Hernia 16:627–633. https://doi.org/10.1007/s10029-012-0964-8
Blonk L, Civil YA, Kaufmann R, Ket JC, van der Velde S (2019) A systematic review on surgical treatment of primary epigastric hernias. Hernia 23:847–857. https://doi.org/10.1007/s10029-019-02017-4
Ponten JE, Leenders BJ, Leclercq WK, Lettinga T, Heemskerk J, Konsten JL, Castelijns PS, Nienhuijs SW (2018) Mesh versus patch repair for epigastric and Umbilical Hernia (MORPHEUS Trial); one-year results of a randomized controlled trial. World J Surg. 42:1312–1320. https://doi.org/10.1007/s00268-017-4297-8
Ponten JEH, Leclercq WKG, Lettinga T, Heemskerk J, Konsten JLM, Bouvy ND, Nienhuijs SW (2019) Mesh OR patch for hernia on epigastric and Umbilical sites (MORPHEUS-Trial): the complete two-year follow-up. Ann Surg. 270:33–37. https://doi.org/10.1097/SLA.0000000000003086
Bernardi K, Olavarria OA, Holihan JL, Kao LS, Ko TC, Roth JS, Tsuda S, Vaziri K, Liang MK (2020) Primary fascial closure during laparoscopic ventral hernia repair improves patient quality of life: a multicentre, blinded randomized controlled trial. Ann Surg 271:434–439. https://doi.org/10.1097/SLA.0000000000003505
Henriksen NA, Montgomery A, Kaufmann R, Berrevoet E, East B, Fischer J et al (2020) Guidelines for treatment of umbilical and epigastric hernias from the European Hernia Society and Americas Hernia Society. BJs 107:171–190. https://doi.org/10.1002/bjs.11489
Stechemesser B, Jacob DA, Schug-Pass C (2012) Köckerling Herniamed: an internet-based registry for outcome research in hernia surgery. Hernia 16:269–276. https://doi.org/10.1007/s10029-012-0908.3
Kyle-Leinhase I, Köckerling F, Jorgensen LN, Montgomery A, Gillion JF, Rodriguez JAP, Hope W, Muysoms F (2018) Comparison of hernia registries: the CORE project. Hernia 22:561–575. https://doi.org/10.1007/s10029-017-1724-6
Köckerling F, Brunner W, Fortelny R, Mayer F, Adolf D, Niebuhr H, Lorenz R, Reinpold W, Zarras K, Weyhe D (2020) Treatment of small (< 2 cm) umbilical hernias: guidelines and current trends from the Herniamed Registry. Hernia. https://doi.org/10.1007/s10029-020-02345-w
Muysoms FE, Miserez M, Berrevoet F, Campanelli G, Champault DD, Chelala E et al (2009) Classification of primary and incisional abdominal wall hernias. Hernia 13:407–414. https://doi.org/10.1007/s10029-009-0518-x
Ponten JE, Leenders BJ, Charbon JA, Nienhuijs SW (2015) A consecutive series of 235 epigastric hernias. Hernia 19:821–825. https://doi.org/10.1007/s10029-014-1227-7
Köckerling F, Hoffmann H, Mayer F, Zarras K, Reinpold W, Fortelny R, Weyhe D, Lammers B, Adolf D, Schug-Pass C (2020) What are the trends in incisional hernia repair?–Real-world data over 10 years from the Herniamed Registry. Hernia. https://doi.org/10.1007/s10029-020-02319-y
Sharma A (2018) Berger D The current role of laparoscopic IPOM repair in abdominal wall reconstruction. Hernia 22:739–741. https://doi.org/10.1007/s10029-018-1820-2
Muysoms F (2018) IPOM: history of an acronym. Hernia 22:743–746. https://doi.org/10.1007/s10029-018-1804-2
Christoffersen MW, Helgstrand F, Rosenberg J, Kehlet H, Bisgaard T (2013) Lower reoperation rate for recurrence after mesh versus sutured elective repair in small Umbilical and Epigastric Hernias A Nationwide Registry Study. World J Surg 37:2548–2552. https://doi.org/10.1007/s00268-013-2160-0
Christoffersen MW, Helgstrand F, Rosenberg J, Kehlet H, Strandfelt P (2015) Bisgaard T Long-term recurrence and chronic pain after repair for small umbilical or epigastric hernias: a regional cohort study. Am J Surgery 209:725–732. https://doi.org/10.1016/j.amjsurg.2014.05.021
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Köckerling reports grants from Johnson & Johnson, Norderstedt, grants from Karl Storz, Tuttlingen, grants from pfm medical, Cologne, grants from Dahlhausen, Cologne, grants from B Braun, Tuttlingen, grants from MenkeMed, Munich, grants from Bard, Karlsruhe, during the conduct of the study; personal fees from Bard, Karlsruhe, outside the submitted work. All other authors have nothing to disclose.
Ethical approval
As only cases of routine hernia surgery are documented in the Herniamed Registry, an ethical approval was not neccessary.
Human and animal rights
This article does not contain any study with animals performed by any of the authors.
Informed consent
All patients with routine hernia surgery documented in the Herniamed Registry have signed an informed consent declaration agreeing to participate.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Köckerling, F., Adolf, D., Zarras, K. et al. What is the reality in epigastric hernia repair?–a trend analysis from the Herniamed Registry. Hernia 25, 1083–1094 (2021). https://doi.org/10.1007/s10029-021-02408-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-021-02408-6