Abstract
Purpose
Abdominal wound dehiscence (AWD) is associated with significant morbidity and mortality. We aimed to provide a contemporary overview of management strategies for AWD.
Methods
PubMed, EMBASE, the Cochrane library and a clinical trials registry were searched from 2009 onwards using the key words “abdominal wound dehiscence”, “fascial dehiscence” and “burst abdomen”. Study outcomes included surgical site infection (SSI), recurrence, incisional hernia and 30-day mortality. Studies reported by the EHS clinical guidelines on AWD were included and compared with. OpenMetaAnalyst was used for meta-analysis to calculate statistical significance and odds ratios (OR).
Results
Nineteen studies were included reporting on a total of 632 patients: 16 retrospective studies, one early terminated randomized controlled trial, one review and the European Hernia Society guidelines. Nine studies reported use of synthetic mesh (n = 241), two of which used vacuum-assisted mesh-mediated fascial traction (VAWCM) (n = 19), six without VAWCM (n = 198) and one used synthetic mesh with both VAWCM (n = 6) and without VAWCM (n = 18); two used biological mesh (n = 19). Seven studies reported primary suture closure (n = 299). Three studies reported on an alternative method (n = 91). Follow-up ranged between 1 and 96 months. Meta-analysis was performed to compare the primary suture group with the synthetic mesh group. Heterogeneity was low to moderate depending on outcome. The overall SSI rate in the primary suture group was 27.6% versus 27.9% in the synthetic mesh group, resulting in mesh explantation in five patients; OR 0.65 (95% CI 0.23–1.81). Incisional hernia rates were 11.1% in the synthetic mesh group (19/171) and 30.7% in the primary suture group (67/218); OR 4.01 (95% CI 1.70–9.46). Recurrence rate did not show a statistically significant difference at 2.7% in the synthetic mesh group (3/112), compared to 10.2% in the primary suture group (21/206); OR 1.81 (95% CI 0.18–17.80). Mortality rates varied between 11.2% and 16.7% for primary suture group versus synthetic mesh; OR 1.85 (95% CI 0.91–3.76).
Conclusion
Included studies were of low to very low quality. The use of synthetic mesh results in a significantly lower rate of incisional hernia, whereas SSI rate was comparable to primary suture repair.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Abdominal wound dehiscence (AWD) is a serious postoperative complication associated with significant morbidity and mortality. The incidence of AWD ranges between 2% and 5.5% [1,2,3,4,5,6]. Mortality has been reported as high as 20.9% [7,8,9,10,11,12,13,14,15,16,17,18].
AWD usually occurs between the 6th and 12th postoperative day [12, 18,19,20]. It is associated with high costs prolonged hospital stay, repeat surgery and a frequent need for ambulatory wound care and follow-up visits [21].
Frequently reported surgery-related risk factors include the type of incision and type of closure technique. Data on the management of AWD are scarce, with low grades of evidence for the most effective management [22].
The European Hernia Society (EHS) formulated clinical guidelines for the treatment of burst abdomen [22]. It is suggested to treat patients with mesh reinforcement whenever fascial closure is possible, while the type and location of mesh should be evaluated by the treating surgeon [22]. Primary suture is a possible classical alternative, using continuous monofilament sutures, 5–8 mm from the wound edge, using a suture length to wound length ratio (SL:WL) of at least 4:1 [22,23,24,25]. The use of mesh was associated with an increased incidence of surgical site occurrence (SSO), as SSO for patients treated with mesh was 48.8% compared to 23.5% for primary suture closure [22].
This study represents an overview of recently published articles on the management of AWD, with an aim to investigate the impact of mesh and other techniques on the core clinical outcomes of surgical site infection (SSI), recurrence and hernia formation [22].
Methods
As a follow-up on a previously published review paper in 2010 [19], PubMed, EMBASE, the Cochrane Library and a trial registry (www.clinicaltrials.gov) were searched in duplicate from January 2009 onwards up to December 2019 using the keywords “abdominal wound dehiscence”, “fascial dehiscence” and “burst abdomen”. Studies reporting on a non-abdominal wound dehiscence, animals, children and studies with no original data were excluded. Non-English language articles were excluded. Only studies reporting on adults with AWD after midline incision and one or more of the outcomes surgical site infection (SSI), recurrence, incisional hernia or 30-day mortality were included.
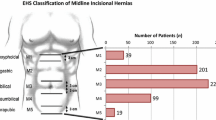
Recurrence was defined as the result of a technical failure after surgical repair, presenting as fascial reburst of the abdominal wall. SSI was defined using Centers for Disease Control and Prevention criteria [26]. Incisional hernia was defined by the EHS as “any abdominal wall gap with or without a bulge in the area of a postoperative scar perceptible or palpable by clinical examination or imaging” [27, 28]. References of included studies were evaluated for potentially relevant articles. Included studies were grouped by management method and data extraction was performed by AD and checked by GvR. The characteristics of included studies are described in Table 1.
Relevant data of studies included in the earlier meta-analysis for the EHS guidelines were also considered in our study [29], following the same methodology and analysis strategy with OpenMetaAnalyst [22, 29]. Collected data were presented as the risk ratio with 95% confidence interval (CI). Heterogeneity was assessed using I2 statistics, considering I2 below 50 as low heterogeneity, 50–70 as moderate heterogeneity and over 70 as high heterogeneity. Results were calculated with Binary Random-Effects Model.
Results
The search resulted in 4395 hits. After removal of duplicates, 4312 articles remained. After screening based on title and abstract, 4275 articles were excluded. Thirty-seven full-text articles were assessed for eligibility. Twenty-four articles were excluded based on no midline incision (n = 1), no clear difference in patient population (n = 1), not abdominal (n = 2), no abdominal wound dehiscence (n = 2), reporting on animals (n = 1), reporting on children (n = 1), no original data (n = 3) and no full text available for two articles. After cross-referencing, five articles were added, see Fig. 1; one study was identified in the trial registry. A total number of 19 studies were included: 16 retrospective studies, one early terminated randomized controlled trial, one review and the EHS guidelines. No prospective non-randomised studies were found. Follow-up ranged between 1–96 months.
Patient characteristics of the 19 included studies are described in Table 2; many did not report on possible confounding variables. Scholtes et al. reported 23 patients with wound class 3 (contaminated) (51.1%) and 22 patients with wound class 4 (dirty) (48.9%) treated with primary suture. In the synthetic mesh group 22 patients were reported with wound class 3 (66.7%) and 11 with wound class 4 (dirty; 33.3%) [8]. Dumanian et al. reported 20 patients with wound class 2 (clean-contaminated) (41.7%), 16 with wound class 3 (33.3%) and 12 with wound class 4 (25%) [13]. Other included studies did not report on wound class.
Patients were treated with synthetic mesh, with or without vacuum-assisted wound closure with mesh-mediated fascial traction (VAWCM), biological mesh, primary suture closure or an alternative management method. Alternative management methods include ‘retention-type’ use of nasogastric tubes (NGT), intrawound continuous negative pressure and irrigation therapy (IW-CONPIT) and synthetic mesh strips.
Mesh
Nine studies reported the use of synthetic mesh, with a total of 241 patients [8, 10,11,12, 14, 17, 30]. The synthetic mesh was made of polypropylene in five studies, with a total of 142 patients [8,9,10,11,12]. Lord et al. reported one patient treated with a Prolene® mesh [31]. Jakob et al. treated 54 patients with a polypropylene mesh and 16 patients with a polyester mesh [14]. McNeeley compared the use of Marlex® mesh, Prolene® mesh and Vicryl® mesh on, respectively, seven, four and seven patients [17]. Three studies with a total of 25 patients reported the use of synthetic mesh in combination with VAWCM [9, 10, 31]. In seven studies 216 patients were treated with synthetic mesh only, without VAWCM [8, 10,11,12, 14]. Bjørnsum–Meyer et al. used a temporary polypropylene mesh for VAWCM and performed the final closure using a delayed primary suture closure [9]. Petersson et al. also used a temporary polypropylene mesh, but performed a delayed closure by delayed primary suture or using a retromuscular polypropylene or polyvinylidene mesh [10]. Lord et al. used a Prolene® mesh sutured to the sheath, and the sheath was eventually closed with interrupted nylon sutures after mesh removal [31]. Abbott et al. used a polyglactin mesh to treat ten patients [30].
Kelley et al. performed a retrospective case study on one patient with a 200-cm2 onlay Strattice® biological mesh layer (LifeCell, Branchburg, NJ) [7] after closure of the abdominal wall. After a 6-week follow-up no recurrence, SSI or incisional hernia occurred and the patient survived. The early terminated randomized controlled study (NCT01083472), found in the trial registry only, included 37 out of 200 participants [32]. Eighteen patients were randomized for intraperitoneal or retrorectus placement of Strattice®; one developed a superficial wound infection and three patients experienced recurrences (16.7%); no incisional hernia was found after an unclear period of follow-up. The remaining 19 patients received ‘standard of care’, consisting of primary suture closure or absorbable bridging mesh with no data provided per subpopulation. This group was subsequently excluded from analysis.
Mesh position
The mesh was reported to be sutured in the onlay position in 57 patients, 56 with a non-absorbable mesh (polypropylene) and 1 with an absorbable mesh (Strattice®) [7, 11]. A total of 103 patients were treated with intraperitoneally placed mesh: in 87 patients polypropylene mesh was used and polyester mesh was used in 16 patients [8, 14]. For 18 patients Strattice® mesh was used in either intraperitoneal or retrorectus position [32]. The inlay position was used for 53 patients, using polypropylene for 24, polyglactin for 17, Marlex® for seven and Prolene® for five patients [9, 10, 17, 30, 31]. The type of mesh, mesh position and definitive closure technique of all studies reporting on the use of mesh can be found in Table 3.
Primary suture closure
Primary suture closure remained a widely reported technique to treat AWD. Seven studies reported the use of primary suture closure with a total of 299 patients, treated from 1986 till 2015 [8, 10, 11, 14, 15, 18, 30]. Gislason et al. reported the use of 5 different suture materials, using polyglactin (Vicryl®) for 18 patients, polyglycolic acid (Dexon) for 17 patients, polyglyconate (Maxon™ loop) for 10 patients, polydioxanone (PDS®) for 2 patients and polyamide (Ethilon™) for 2 patients; 4 patients were treated with unknown material [18]. Polydioxanone was used in 5 studies to treat 143 patients in total [8, 10, 11, 14, 18]. Tilt et al. used Prolene® as a suture material to treat 43 patients [15]. Scholtes et al. and Petersson et al. used Vicryl® strings and polypropylene, respectively, but did not report patient numbers [8, 10].
Jakob et al. was the only group that reported on the applied suture to wound length ratio (SL: WL ratio) of 4:1 [14]. Time period, suture materials and technique of the included studies reporting on primary suture closure are presented in Table 4.
Alternative management methods
Vahedian et al. reported the use of nasogastric tubes (NGT) with an interrupted suture technique on 25 patients [33]. They used one ultraviolet sterilized black NGT (10 FG) and one Hemovac perforator. The NGTs were sutured with a simple interrupted suture technique, and the NGTs were tied. Each patient received 4–5 NGT sutures with the distance of 4–5 cm. Delayed skin closure by far-and-near suturing technique was used in patients if needed; otherwise, the skin was left to close by secondary intention. During the 1-month follow-up, no recurrence, mortality, SSI or incisional hernia occurred [33].
Dumanian et al. used strips of light-weight macroporous polypropylene mesh [13]. The mesh was cut into 2 cm-wide pieces in order to fabricate mesh strips. The mesh strips were placed in interrupted fashion and spaced 1 cm from each other. A total number of 48 patients were treated with this new technique, with a mean follow-up of 358 days (11.8 months). A SSI rate of 19.0% (9/47) was reported, of which seven had superficial infections. None of them required mesh strip removal [13]. One patient died during follow-up—unrelated to use of mesh strips—resulting in 47 surviving patients. Three patients (6.0%) developed recurrence and three (6.0%) an incisional hernia at their midline closure. Incisional hernia was defined as “any defect in the abdominal wall fascia as diagnosed by physical examination or CT scan”, after a mean 11.8-month follow-up [13].
Morinaga et al. used intrawound continuous negative pressure and irrigation treatment (IW-CONPIT) with artificial dermis as a new technique to treat AWD [16]. Eighteen patients were treated between March 2007 and August 2016 using this technique, with an unknown period of follow-up. After complete debridement, artificial dermis PELNAC was attached to the exposed bowel. Two tubes were inserted into the sponge to provide continuous irrigation with saline (1–3 l/day). One tube was connected with a bottle containing saline solution, the other to a continuous suction unit. After complete epithelialization, intestinal resection was performed and the abdominal wall was reconstructed [16]. Morinaga et al. reported a 0.0% (0/18) mortality rate [16].
Meta-analysis
Comparisons were made for primary sutured group and synthetic mesh group only, as the numbers of relevant studies for other techniques were deemed too low.
The overall mortality rate for the primary sutured group was 15.9% (43/270 patients) compared to 11.7% (23/206 patients) for the synthetic mesh group [8, 10,11,12, 14, 15, 17, 18]. The mortality rate for patients treated with synthetic mesh in combination with VAWCM was 16.7% (4/24) [9, 10]. Mortality rates were not significantly higher for primary suture closure than for the synthetic mesh group (p = 0.136), odds ratio (OR) 1.85, [95% CI 0.91–3.76], I2 = 8.39, see Fig. 2.
Overall SSI rate in the mesh group was 27.9% (41/147 patients) [10,11,12, 14, 17], resulting in mesh explantation for five patients [14, 17]. Jakob et al. compared the use of polypropylene and polyester mesh. 16 of the 45 patients (36%) treated with polypropylene mesh occurred to have SSI compared to eight of the 14 patients (57%) treated with polyester mesh. SSI resulted in partial mesh removal in 2/45 (4%) treated with polypropylene mesh and 2/14 patients treated with polyester mesh [14]. For primary suture closure, 27.6% (59/214 patients) had a SSI [9,10,11,12, 14, 15, 18], but this was not significantly different compared to the mesh group (p = 0.103), OR 0.65 (95% CI 0.23–1.81), I2 = 45.35, see Fig. 3.
Overall recurrence rates were 2.7% (3/112 patients) in the synthetic mesh group versus 10.2% (21/206 patients) in the primary suture group [9,10,11, 15]; OR 1.81 (0.18; 17.80) I2 = 55.63, see Fig. 4. Three of the 15 patients (20.0%) treated with synthetic mesh with VAWCM developed a recurrence [9]. In the group treated with synthetic mesh without VAWCM, no recurrence was reported (0/97 patients)[10,11,12, 30].
Incisional hernia occurred in 11.1% (19/171 patients) of all patients treated with synthetic mesh. Patients treated without VAWCM developed an incisional hernia in 10.2% (16/157 patients). The use of synthetic mesh in combination with VAWCM resulted in three incisional hernias out of 14 patients (21%) [8,9,10,11,12, 14].
Bjørsum-Meyer et al. reported three incisional hernias (3/14, 21%), after 1, 12 and 19 months [9]. Petersson et al. had a median follow-up of 405 days (40–953 days) and reported one incisional hernia (1/20, 5.0%) [34]. López-Cano et al. followed 34 mesh group patients (34/56, 60.7%), six patients developed incisional hernia after a minimum follow-up of 12 months (6/34, 17.6%) [11].
Primary suture closure resulted in an incisional hernia rate of 30.7% (67/218 patients) [8, 10, 11, 14, 15, 18]. Gislason et al. reported a 43% incisional hernia rate (23/53 patients) with a median follow-up of 23 months (1–8 years), with different hernia rates for various suture materials [18]. Reported rates are included in Table 5. Petersson et al. had a median follow-up of 619 days (205–1042 days) and 53.3% developed an incisional hernia (8/15 patients) [10].
Incisional hernia rates were significantly higher for patient after primary suture closure [p = 0.036, OR 4.01 (95% CI 1.70–9.46), I2 = 22.60] using Binary Random-Effects Model, see Fig. 5. No significant difference was observed between primary suture closure and mesh group for SSI, recurrence and mortality.
Two studies received external funding [22, 32]; one study received an internal funding [13].
Discussion
This study provides an overview of the impact of mesh and other closing techniques on the core clinical outcomes of surgical site infection (SSI), recurrence and hernia formation as to be able to guide surgeons towards current best evidence. To date, only published retrospective studies were found in the literature and only a few studies had considerable numbers of patients. Our meta-analysis showed that the use of synthetic mesh results in lower incisional hernia rates compared to primary suture closure, confirming previously published results [8, 10, 11, 14, 30]. This reinforces the statement that patients with a high risk for developing an incisional hernia should be treated with a synthetic mesh. There are various reports indicating that the use of a synthetic mesh results in higher SSI and SSO rates than primary suture closure [10, 11, 14]. In this meta-analysis, SSI were considerable in both groups, but there was no significant difference in favour of the primary suture group. Consequences of SSI may include mesh removal and prolonged treatment with antibiotics.
Lima et al. reported that AWD can be prevented in high-risk patients, using our previously developed risk score for AWD [4, 35]. They compared the use of a preventive polypropylene mesh in the onlay position to primary suture closure using slowly absorbable running sutures in high-risk patients undergoing emergency laparotomy [34]. In this randomized clinical trial, the use of a mesh prevented fascial dehiscence (0/63 patients) when compared to the 7 out of 52 patients (13.5%) in the suture group (p = 0.003). The use of mesh was not associated with significantly higher SSO rates, but some specific SSO (SSI, seroma and superficial wound dehiscence) were more frequently reported. SSO rates were 42.9% (27/63 patients) in the mesh group and 28.8% (15/52 patients) in the suture group. However, this study was based on prevention of AWD, not treatment [34].
Limitations of our study include the retrospective design of the studies that were included, with a considerable proportion of possible confounding variables not reported by the majority, such as wound class. Clean wounds could be closed with primary suture closure, although in the literature this is associated with higher recurrence rates [10, 19, 30]. The use of synthetic mesh is often associated with a decrease in incisional hernia rates, as confirmed in our meta-analysis [8, 10, 11, 14]. Mortality rates were lower for patients treated with synthetic mesh versus patients treated with primary suture closure, although statistically not significant and, possibly, a form of selection bias. This confirms previously published results [8, 11, 14]. Considering the sum of these outcomes, the use of synthetic mesh is slightly favourable over primary suture closure. The EHS clinical guidelines reported that the use of a mesh is related to an increased incidence of SSO, but a decreased incisional hernia rate and mortality rate. The EHS recommends the use of mesh reinforcement whenever fascial closure is possible [22]. Overall, the results by the EHS are comparable with results of our meta-analysis. As for clinical implications, surgeons will still need to assess the contamination degree of the wound and trade the risk of SSI for the benefit of decreased AWD with a synthetic mesh closure. In case of dirty wounds, the risk of mesh infection may be higher than the benefit from decreased hernia.
Our analysis included 11 studies published after 2010, providing a relevant update of recent literature regarding the management of AWD. VAWCM was published by Petersson, often proposed as a good alternative in cases with severe visceral swelling [35]. VAWCM is often associated with high material cost [36, 37]. With only three studies reporting on the use of VAWCM and outcomes limited to less than 25 patients, it is a technique that needs more exploration in terms of potential benefits in the setting of AWD [9, 10, 31]. We are aware that some surgeons use a strategy involving onlay slowly resorbable mesh in combination with negative pressure wound therapy, but we were unable to find any reports. Retention type sutures, like NGT presented by Vahedian et al. may provide an alternative for resource-limited countries [33]. Mesh strips, IW-CONPIT and biological meshes are newly presented alternatives with early promising results [7, 13, 16]. Dumanian et al. recommended mesh strips in contaminated wounds [13]. Mesh strips offer the durability of a planar mesh, while minimizing the total volume of material. Future studies on these new techniques are needed to compare the surgical outcomes of primary suture closure and synthetic mesh with the new techniques.
Conclusion
There is an overall lack of evidence in studies published regarding the management of abdominal wound dehiscence. The use of synthetic mesh shows the best outcomes with regard to incisional hernia rate, and inclusion of the latest studies showed no increase in SSI rates. Results reported in the EHS clinical guidelines correspond with our findings, confirming the recommendation to use mesh when fascial closure is possible. Methods like VAWCM, the use of synthetic mesh strips and the use of biological mesh have only been reported anecdotally.
References
Gislason H, Grønbech J, Søreide O (1995) Burst abdomen and incisional hernia after major gastrointestinal operations–comparison of three closure techniques. Euro j surg Acta Chir 161(5):349–354
Webster C, Neumayer L, Smout R et al (2003) Prognostic models of abdominal wound dehiscence after laparotomy. J Surg Res 109(2):130–137
Seiler CM, Bruckner T, Diener MK et al (2009) Interrupted or continuous slowly absorbable sutures for closure of primary elective midline abdominal incisions: a multicenter randomized trial (INSECT: ISRCTN24023541). Ann Surg 249(4):576–582
van Ramshorst GH, Nieuwenhuizen J, Hop WC et al (2010) Abdominal wound dehiscence in adults: development and validation of a risk model. World J Surg 34(1):20
Bloemen A, Van Dooren P, Huizinga B, Hoofwijk A (2011) Randomized clinical trial comparing polypropylene or polydioxanone for midline abdominal wall closure. Br J Surg 98(5):633–639
Kenig J, Richter P, Lasek A, Zbierska K, Zurawska S (2014) The efficacy of risk scores for predicting abdominal wound dehiscence: a case-controlled validation study. BMC surgery 14(1):65
Kelley BP, Heller L (2012) A novel approach to repair of wound dehiscence in the complicated patient. Hernia 16(3):369–372
Scholtes M, Kurmann A, Seiler CA, Candinas D, Beldi G (2012) Intraperitoneal mesh implantation for fascial dehiscence and open abdomen. World J Surg 36(7):1557–1561
Bjørsum-Meyer T, Skarbye M, Jensen KH (2013) Vacuum with mesh is a feasible temporary closure device after fascial dehiscence. Dan Med J 60(11):A4719–A4719
Petersson P, Montgomery A, Petersson U (2014) Wound dehiscence: outcome comparison for sutured and mesh reconstructed patients. Hernia 18(5):681–689
López-Cano M, Pereira JA, Feliu X et al (2015) Outcome of the use of a synthetic mesh in the repair of burst abdomen as compared with simple suture. Internat J Clin Med 6(03):113
Abo-Ryia MH (2017) Simple and safe technique for closure of midline abdominal wound dehiscence. Hernia 21(5):795–798
Dumanian GA, Lanier ST, Souza JM et al (2018) Mesh sutured repairs of contaminated incisional hernias. Am J Surg 216(2):267–273
Jakob MO, Spari D, Zindel J, Pinworasarn T, Candinas D, Beldi G (2018) Prophylactic, synthetic intraperitoneal mesh versus no mesh implantation in patients with fascial dehiscence. J Gastrointest Surg 22(12):2158–2166
Tilt A, Falola RA, Kumar A et al (2018) Operative management of abdominal wound dehiscence: outcomes and factors influencing time to healing in patients undergoing surgical debridement with primary closure. Wounds 30(11):317–323
Morinaga K, Rikimaru Y, Kiyokawa K (2019) Treatment of abdominal surgical wound dehiscence with bowel exposure and infection: using intrawound continuous negative pressure, irrigation, and application of artificial dermis. Ann Plast Surg 82(2):213–217
McNeeley SG Jr, Hendrix SL, Bennett SM et al (1998) Synthetic graft placement in the treatment of fascial dehiscence with necrosis and infection. Am J Obstet Gynecol 179(6 Pt 1):1430–1435
Gislason H, Viste A (1999) Closure of burst abdomen after major gastrointestinal operations–comparison of different surgical techniques and later development of incisional hernia. Eur J Surg 165(10):958–961
van Ramshorst GH, Eker HH, Harlaar JJ, Nijens KJ, Jeekel J, Lange JF (2010) Therapeutic alternatives for burst abdomen. Surg Technol Int 19:111–119
López-Cano M, Pereira JA, Armengol-Carrasco M (2013) “Acute postoperative open abdominal wall”: Nosological concept and treatment implications. World J Gastrointest Surg 5(12):314–320
van Ramshorst GH, Eker HH, van der Voet JA, Jeekel J, Lange JF (2013) Long-term outcome study in patients with abdominal wound dehiscence: a comparative study on quality of life, body image, and incisional hernia. J Gastrointest Surg 17(8):1477–1484
López-Cano M, García-Alamino JM, Antoniou SA et al (2018) EHS clinical guidelines on the management of the abdominal wall in the context of the open or burst abdomen. Hernia 22(6):921–939
Harlaar JJ, van Ramshorst GH, Nieuwenhuizen J et al (2009) Small stitches with small suture distances increase laparotomy closure strength. Am J Surg 198(3):392–395
Israelsson LA, Millbourn D (2012) Closing midline abdominal incisions. Langenbecks Arch Surg 397(8):1201–1207
Millbourn D, Cengiz Y, Israelsson LA (2011) Risk factors for wound complications in midline abdominal incisions related to the size of stitches. Hernia 15(3):261–266
Horan TC, Andrus M, Dudeck MA (2008) CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 36(5):309–332
Korenkov M, Paul A, Sauerland S et al (2001) Classification and surgical treatment of incisional hernia. Results of an experts’ meeting. Langenbecks Arch Surg 386(1):65–73
Muysoms FE, Miserez M, Berrevoet F et al (2009) Classification of primary and incisional abdominal wall hernias. Hernia 13(4):407–414
CEBM. OpenMeta [Analayst]. https://www.cebm.brown.edu/openmeta/index.html.
Abbott DE, Dumanian GA, Halverson AL (2007) Management of laparotomy wound dehiscence. Am Surg 73(12):1224–1227
Lord AC, Hompes R, Venkatasubramaniam A, Arnold S (2015) Successful management of abdominal wound dehiscence using a vacuum assisted closure system combined with mesh-mediated medial traction. Ann R Coll Surg Engl 97(1):e3–e5
Repair of Challenging Abdominal Wall Defects: Strattice(TM) TM in Abdominal Wall Repair (StAR) (StAR), Clinicaltrials.gov identifier NCT010834722013.
Vahedian J, Jahanian S, Banivaheb B et al (2018) A new method for surgical Abdominal mass closure after abdominal fascial dehiscence using Nasogastric tube and Hemovac perforator: a case-series study. World J Surg 42(10):3106–3111
Lima HVG, Rasslan R, Novo FCF et al (2020) Prevention of fascial dehiscence with onlay prophylactic mesh in emergency laparotomy: a randomized clinical trial. J Am Coll Surg 230(1):76–87
Petersson U, Acosta S, Bjorck M (2007) Vacuum-assisted wound closure and mesh-mediated fascial traction–a novel technique for late closure of the open abdomen. World J Surg 31(11):2133–2137
Deleyto E, García-Ruano A, González-López JR (2018) Negative pressure wound therapy with instillation, a cost-effective treatment for abdominal mesh exposure. Hernia 22(2):311–318
Acosta S, Bjorck M, Petersson U (2017) Vacuum-assisted wound closure and mesh-mediated fascial traction for open abdomen therapy - a systematic review. Anaesthesiol Inten Thera 49(2):139–145
Funding
No funding was received for any part of the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors reported a conflict of interest.
Ethical approval
As this was a meta-analysis, no ethical approval was requested.
Human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
No informed consent is required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Denys, A., Monbailliu, T., Allaeys, M. et al. Management of abdominal wound dehiscence: update of the literature and meta-analysis. Hernia 25, 449–462 (2021). https://doi.org/10.1007/s10029-020-02294-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-020-02294-4