Abstract
Background
While performing unilateral TEP herniorrhaphy, controversy still exists about whether to do contralateral exploration or not. Routine contralateral exploration has been proposed to prevent metachronous contralateral hernias by the repair of incidental contralateral occult hernias. Some surgeons have even proposed to do prophylactic bilateral TEP herniorrhaphy for unilateral hernia patients. To evaluate the appropriateness of not doing contralateral exploration in unilateral TEP herniorrhaphy, we reviewed our experiences under our practice of no contralateral exploration and we also reviewed other published literature.
Methods
A total of 305 patients who underwent 313 TEP herniorrhaphies for inguinal hernias by a single surgeon during August 2012–July 2016 at Chia-Yi Christian Hospital were enrolled in this retrospective study. Demographic, perioperative and follow-up data were obtained for analysis and review.
Results
Of the 305 patients, 261 patients had unilateral TEP herniorrhaphy and 44 patients had bilateral TEP herniorrhaphy. The mean operation time for the unilateral TEP herniorrhaphy group was 59.8 min, and for the bilateral TEP herniorrhaphy group it was 85.2 min (p < 0.001). Seven of 261 (2.7%) patients had metachronous contralateral hernia after unilateral TEP herniorrhaphy. There were no statistically significant differences in any of the outcome variables when comparing the sequential and simultaneous primary bilateral TEP herniorrhaphies.
Conclusions
Without routine contralateral exploration, the incidence of metachronous contralateral hernia was 2.7% (7/261) in unilateral hernia patients. This is acceptable as metachronous hernia also occurred in 3.2% of patients with negative contralateral exploration according to our literature review. Sequential and simultaneous bilateral primary TEP herniorrhaphy outcomes were similar. We conclude that no exploration for the other groin is a justified decision for unilateral inguinal hernia patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
For bilateral inguinal hernia patients, all international surgical societies recommend simultaneous laparoscopic inguinal hernia repair (LIHR) surgery as the standard treatment [1,2,3]. Although these patients can be managed with one operation, some unilateral inguinal hernia patients need sequential operations as metachronous contralateral hernia sometimes subsequently develop. These metachronous contralateral hernias might be independent events or consequences of uninspected contralateral occult hernias. Reported incidences of contralateral occult hernias in unilateral inguinal hernia patients ranges from 4.2% (15/361) to 57.5% (42/73) [4, 5]. Up to 28% of untreated incidental contralateral occult hernias will progress to symptomatic hernias [6]. Thus, the guidelines suggest that unilateral inguinal hernia patients should be informed of the possibility of contralateral occult hernias. The decision to proceed with simultaneous repair should be included in the consent form [2]. How to prevent a second operation for metachronous contralateral hernia in unilateral inguinal hernia patients is an issue. Some authors have even proposed prophylactic bilateral repair for unilateral inguinal hernia patients [5, 7]. But the risk of chronic post-herniorrhaphy pain and the possibility of hernia recurrence still make it difficult to recommend whether or not to perform prophylactic bilateral repair.
Totally extraperitoneal (TEP) and trans-abdominal pre-peritoneal (TAPP) repair are two standardized techniques for LIHR [2, 3]. There are advantages and disadvantages for both TEP and TAPP procedures. For inguinal hernia patients, TEP herniorrhaphy is our routine practice at Chia-Yi Christian Hospital (CYCH). When diagnosing contralateral occult hernias, the TEP approach needs extra explorations. With positive findings, simultaneous TEP herniorrhaphy of incidental contralateral occult hernias can avoid reoperation, second anesthetic exposure, another period of work loss and containment of costs to the healthcare system. With negative findings, this approach causes a violation of a virgin space, difficulty in the event of a need for surgery at a later date, the additional time, and trauma associated with the procedure. While performing unilateral TEP herniorrhaphy, controversy still exists about whether to inspect the contralateral groin [8].
As there is no routine contralateral exploration for unilateral hernia patients in our hospital, few patients received sequential bilateral TEP herniorrhaphy as metachronous contralateral hernias occurred. The first question is how much it cost if we perform prophylactic bilateral TEP herniorrhaphies for unilateral hernia patients. To evaluate the suitability of prophylactic bilateral TEP herniorrhaphy for unilateral inguinal hernia patients, analysis of unilateral versus bilateral TEP herniorrhaphy was conducted. The second question is how many metachronous contralateral hernia would trouble the patients after unilateral TEP herniorrhaphies. To investigate the incidence and treatment courses of metachronous contralateral hernia in unilateral inguinal hernia patients, we present analyses of sequential versus simultaneous primary bilateral TEP herniorrhaphies. Based on the data and current literature review, we can optimize the decision-making process for unilateral hernia patients.
Materials and methods
A total of 305 patients who underwent 313 TEP herniorrhaphies for inguinal hernias by a single surgeon during August 2012–July 2016 at CYCH were enrolled into this retrospective cohort study. All patients received herniorrhaphies with mesh reinforcement, also known as hernioplasty. Patient demographics, relevant clinical history, perioperative findings and post-operative clinical courses were reviewed. A patient with comorbidity was defined by the presence of diabetes mellitus, hypertension, lung disease, etc. To eliminate the concern due to surgical experience effects on outcome variables, the cut point date between early and late phase operations in the study was 1st January, 2014 when approximately one hundred patients were enrolled. The type of hernia, incarcerated and strangulated hernia was all diagnosed intra-operatively. Re-do cases were defined as patients who received non-fresh herniorrhaphies. Presence of chronic pain was defined as Visual Analogue Scale (VAS) score > 5 over more than 6 months after herniorrhaphies. The outcome variables, including operation time, presence of complications, whether recurrent or not, length of hospital stay, number of post-operative outpatient follow-up visits and follow-up time were collected by medical record reviews and telephone interviews. The cutoff date for analysis was November 8th, 2017. The last follow-up date was obtained from the latest medical records in CYCH or from the telephone survey data, whichever was later. Those considered as ‘lost to follow-up’ refers to those patients with inactive medical files in CYCH 1 month or more post-surgery and/or there was no response to the telephone survey. This study was approved by the CYCH Institutional Review Board.
The study designs and data details of this study are illustrated in Fig. 1. Comparison of unilateral and bilateral TEP herniorrhaphies is presented in Table 1. Multivariate analysis is conducted in Table 2, identifying the significance of operation time. After excluding re-do patients, fresh inguinal hernia patients who had received simultaneous (n = 33) and sequential (n = 7) bilateral TEP herniorrhaphies were enrolled to conduct analysis as shown in Table 3. Detailed information from our literature review is presented in Table 4 [4,5,6,7,8,9,10,11,12,13,14,15,16,17]. Searches were undertaken in the PubMed computerized database using the following search terms: (occult OR unexpected) AND (groin OR inguinal) AND hernia AND (laparoscopic surgery OR laparoscopy). All resulting titles and abstracts were read. Studies which met our criteria were used to extract the data on topics about the incidences of contralateral occult hernia and metachronous contralateral hernia in adults were obtained and reviewed. All references in these studies were reviewed. Data were arranged in order of the total patient numbers and were summed to show the overall result.
Statistical analysis
Continuous variables are expressed as mean ± standard deviation (SD). Categorical and ordinal variables are expressed as numbers and percentages. Differences in the variables were compared using Student’s t test, ANOVA and Pearson’s Chi-square test. Variables significant in correlation analyses at probability (p) value < 0.050 were entered in multivariate linear regression analysis, performed to determine independent predictors of the operation time. The missing data were treated with the listwise deletion method. The missing rates are less than 5%. A p value < 0.050 is considered statistically significant. Statistical analysis was conducted using SPSS® version 21.0 (IBM Corp., Armonk, NY, USA).
Results
Of the 305 patients, 261 patients had unilateral TEP herniorrhaphy and 44 patients had bilateral TEP herniorrhaphy. Repeat unilateral TEP herniorrhaphy was performed on 8 patients. Seven of them had sequential primary bilateral TEP herniorrhaphy as metachronous contralateral hernia occurred. One of them had unilateral TEP twice due to recurrence. The mean follow-up time of the 305 patients was 2.6 ± 1.5 years. Until the end of this study, 12/305 (3.9%) patients were lost to follow-up and 10/305 (3.3%) patients died. Three patients had chronic pain with VAS score > 5.
The results of a comparison between unilateral and bilateral TEP herniorrhaphy groups are shown in Table 1. The percentage of males with unilateral inguinal hernia at 81.8% was lower than those with bilateral inguinal hernia at 95.5% (p = 0.040). A higher proportion of bilateral TEP herniorrhaphy operations were performed in the late phase of the study (p = 0.002). The dominant hernia type was indirect within the unilateral TEP herniorrhaphy group and direct within the bilateral TEP herniorrhaphy group (p < 0.001). A higher percentage of re-do cases were identified in the bilateral TEP herniorrhaphy group (p < 0.001). The mean operation time for the unilateral TEP herniorrhaphy group was 59.8 min, and for the bilateral TEP herniorrhaphy group it was 85.2 min (p < 0.001). There were no statistically significant differences between the two groups in all other operative outcome variables.
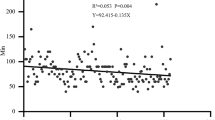
To examine the effect of bilateral TEP herniorrhaphy upon the operation time differences, all significantly different factors between unilateral and bilateral TEP herniorrhaphy groups were evaluated by multivariate linear regression analysis as shown in Table 2. Only the bilateral TEP herniorrhaphy was statistically significant in the model (β = 0.256, p < 0.001). Gender, operation phase, type of hernia and re-do cases were not statistically significant variables.
Without contralateral exploration, the incidence of metachronous contralateral hernia in unilateral hernia patients was 2.7% (7/261) in this study. The mean time interval between first and second TEP herniorrhaphy was 14.4 ± 10.8 months (range 0.6–28.4 months). A comparison of sequential and simultaneous bilateral primary TEP herniorrhaphy is shown in Table 3. A higher proportion of simultaneous bilateral primary TEP herniorrhaphy operations were performed in the late phase of the study (p = 0.001). The dominant hernia type was indirect within the sequential bilateral primary TEP herniorrhaphy group and direct within the simultaneous bilateral primary TEP herniorrhaphy group (p = 0.004). Longer follow-up time was noted in the sequential bilateral primary TEP herniorrhaphy group (p = 0.026). There were no statistically significant differences between the groups in all other operative outcome variables, including operation time. The operation time for second TEP herniorrhaphy was not influenced by the first TEP herniorrhaphy.
Searches in PubMed produced 58 titles. Eight studies [5, 7,8,9, 12, 13, 15, 16] were met our criteria to extract the data on topics about the incidences of contralateral occult hernia and metachronous contralateral hernia in adults. After reviewing these references, six other studies were obtained [4, 6, 10, 11, 14, 17]. In Table 4a, the overall report rate of contralateral occult hernia was 17.4% (675/3871). If incidental occult hernias were left untreated, metachronous contralateral hernia incidences were reported to be 6/21 (28.6%) in 12-month follow-up and 13/61 (21.3%) in 88-month follow-up [6, 9]. The overall report rate of metachronous contralateral hernia developing from untreated contralateral occult hernia was 23.2% (19/82). In Table 4b, the overall report incidences of metachronous contralateral hernia without contralateral exploration was 3.5% (20/564). The overall report incidences of metachronous contralateral hernia after negative contralateral exploration was 3.2% (41/1299). The thinking process of this study and literature review results are illustrated in Fig. 2.
Decision process for clinical unilateral hernia patients. Data reported in the boxes derived from a literature review and a study of the results. Further details are explained in Table 4 and in the “Discussion”
Discussion
Laparoscopic inguinal hernia repair (LIHR) surgery, including TEP and TAPP repair, simplifies the process of bilateral herniorrhaphy. The decision to conduct prophylactic bilateral surgery for unilateral hernia patients leads to lively discussions. Differences between unilateral and bilateral LIHR have been undergoing intense study. In our study, the majority of patients (261/305, 85.6%) underwent unilateral TEP herniorrhaphy. The highly significant impact of uni- and bilateral TEP herniorrhaphy on operation time, as already seen in Table 1, was confirmed in the multivariate model (59.8 ± 29.0 min for unilateral and 85.2 ± 33.0 min for bilateral operation, p < 0.001). No significant differences were found in complication rate, recurrence rate, length of hospital stay and number of post-operative outpatient follow-up services between uni- and bilateral TEP herniorrhaphy groups. Unilateral LIHR was needed in about 70% of the patient population [18, 19]. While controversy still exists about whether bilateral TEP herniorrhaphy is more risky and costly than unilateral TEP herniorrhaphy, a bilateral TEP herniorrhaphy needs more operation time [19]. To spend more operation time and risk causing complications is justified for bilateral inguinal hernia patients. But for unilateral hernia patients, the decision to conduct the prophylactic examination and the subsequence decision to operate on the other groin needs to be carefully assessed, with attention focused on expenses and benefits.
Metachronous contralateral hernia could be a consequence of uninspected contralateral occult hernia at the time of first TEP herniorrhaphy surgery. Therefore, some surgeons routinely practice bilateral exploration during TEP inguinal herniorrhaphy to examine the healthy groin and repair of incidental contralateral occult hernia. The data of our current literature review is presented in Table 4. Figure 2 shows the decision process for clinical unilateral hernia patients. By multiplying the overall report incidence of each scenario after contralateral exploration, the extrapolated incidences of metachronous contralateral hernia are shown in the bottom boxes. The incidences of metachronous contralateral inguinal hernia in patients with positive findings but no surgical intervention was 4.0%. The incidences of metachronous contralateral inguinal hernia in patients with negative finding under observation were 3.2%. That means only 4% of unilateral hernia patients would have benefited from receiving routine contralateral exploration. The possibility of developing severe chronic pain (VAS score > 5) in the groin that was previously completely asymptomatic is low but troublesome for these patients and their surgeons. The incidence of severe post-herniorrhaphy chronic pain was 1.0% (3/305) in this study and 0.9% (2/227) in Manangi’s study [20]. Meanwhile, International Endohernia Society reported the overall mean recurrence rates after TEP repairs during 1999–2008 (N = 13,562) was 0.54% (range 0.1–1.92%) [2]. There is still a possibility of hernia recurrence after prophylactic simultaneous bilateral TEP herniorrhaphy. On the contrary, negative contralateral exploration findings happened in the majority of patients, caused virgin space violation and time waste, and do not ensure metachronous contralateral hernia will not happen. To practice routine bilateral exploration during TEP inguinal herniorrhaphy in unilateral inguinal hernia patients is unnecessary for the majority of patients.
Without contralateral exploration, the incidence of metachronous contralateral hernia in unilateral hernia patients was 2.7% (7/261) in our study. According to Table 4 and Fig. 2, the overall incidence is 3.5% (20/564) which is close to the result found in those who had negative findings of 3.2% (41/1299). No difference was found in outcome variables between sequential and simultaneous bilateral TEP groups in our study, including operation time. The operation time for the second TEP herniorrhaphy was similar to the first TEP herniorrhaphy. Accessing a previously scarred umbilicus entry point is not problematic. Compared to the explored groin, the unexplored one is not only stronger, but also easier to treat if metachronous hernias occur later. While metachronous contralateral hernia is rare and cannot always be prevented by surgery, a justified strategy for inguinal hernia patients is not to explore the contralateral groin.
To maximize the benefit of TEP herniorrhaphy for unilateral hernia patients, it is suggested that improvement of the diagnosis of contralateral occult inguinal hernia should be under a less invasive approach. Rather than TEP contralateral exploration, groin ultrasound and diagnostic laparoscopy may be better methods to improve the diagnosis of contralateral occult inguinal hernia under a less invasive approach. The accuracy of image study is clearly higher than only physical examination. Based on a systematic review of image studies in the diagnosis of occult inguinal hernia [21], ultrasound has a sensitivity of 86% and a specificity of 77%. If there is still diagnostic uncertainty, diagnostic laparoscopy can offer rapid and definite assessment of both groins [15]. Although the presence of pneumoperitoneum may compromise the extraperitoneal space, it is still a better alternative method to prevent unnecessary extraperitoneal space trauma. The patients with unilateral hernia should be provided with an easier approach to check the other groin to allow simultaneous repair if a contralateral occult hernia exists. If metachronous contralateral hernias eventually occur, these unexplored spaces are easier to operate on.
Retrospective studies have disadvantages and limitations. Lack of long-term follow-up and retrospective data collection might underestimate the events of hernia recurrence or occurrence. Patient’s subjective need for hernia surgery could also skew results. From a small sample size of single surgeon experiences and observation of current heterogeneous data, the findings of this study might not be universally applicable, but would be justifiable for common practice. Further prospective randomized studies about whether to routinely do bilateral exploration for unilateral hernia patients are suggested. Additionally, a longer term follow-up is warranted.
Bilateral TEP herniorrhaphy surgery requires significantly longer operation time than unilateral TEP herniorrhaphy. For unilateral hernia patients, prophylactic bilateral TEP herniorrhaphies are not justified due to the low expectation rate of metachronous contralateral hernia. Without routine bilateral exploration, the incidence of metachronous contralateral inguinal hernia was 2.7% (7/261) in unilateral hernia patients in this study. This is acceptable as metachronous hernia also occurred in 3.2% of patients with negative contralateral exploration which occurred in 82.6% of the patients who underwent routine contralateral examination. Sequential and simultaneous bilateral TEP herniorrhaphy outcomes were compatible. No exploration for the other groin is a justified decision for unilateral inguinal hernia patients. Use of image study and diagnostic laparoscopy might maximize the benefit of TEP herniorrhaphy for unilateral hernia patients under a less invasive approach.
References
Simons MP, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J, de Lange D, Fortelny R, Heikkinen T, Kingsnorth A, Kukleta J, Morales-Conde S, Nordin P, Schumpelick V, Smedberg S, Smietanski M, Weber G, Miserez M (2009) European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 13(4):343–403. https://doi.org/10.1007/s10029-009-0529-7
Bittner R, Arregui ME, Bisgaard T, Dudai M, Ferzli GS, Fitzgibbons RJ, Fortelny RH, Klinge U, Kockerling F, Kuhry E, Kukleta J, Lomanto D, Misra MC, Montgomery A, Morales-Conde S, Reinpold W, Rosenberg J, Sauerland S, Schug-Pass C, Singh K, Timoney M, Weyhe D, Chowbey P (2011) Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia [International Endohernia Society (IEHS)]. Surg Endosc 25(9):2773–2843. https://doi.org/10.1007/s00464-011-1799-6
Poelman MM, van den Heuvel B, Deelder JD, Abis GS, Beudeker N, Bittner RR, Campanelli G, van Dam D, Dwars BJ, Eker HH, Fingerhut A, Khatkov I, Koeckerling F, Kukleta JF, Miserez M, Montgomery A, Munoz Brands RM, Morales Conde S, Muysoms FE, Soltes M, Tromp W, Yavuz Y, Bonjer HJ (2013) EAES Consensus Development Conference on endoscopic repair of groin hernias. Surg Endosc 27(10):3505–3519. https://doi.org/10.1007/s00464-013-3001-9
Saggar VR, Sarangi R (2007) Occult hernias and bilateral endoscopic total extraperitoneal inguinal hernia repair: is there a need for prophylactic repair? Results of endoscopic extraperitoneal repair over a period of 10 years. Hernia 11(1):47–49. https://doi.org/10.1007/s10029-006-0157-4
Crawford DL, Hiatt JR, Phillips EH (1998) Laparoscopy identifies unexpected groin hernias. Am Surg 64(10):976–978
Thumbe VK, Evans DS (2001) To repair or not to repair incidental defects found on laparoscopic repair of groin hernia: early results of a randomized control trial. Surg Endosc 15(1):47–49
Pawanindra L, Philips P, Chander J, Ramteke VK (2010) Is unilateral laparoscopic TEP inguinal hernia repair a job half done? The case for bilateral repair. Surg Endosc 24(7):1737–1745. https://doi.org/10.1007/s00464-009-0841-4
Wu CC, Chueh SC, Tsai YC (2016) Is contralateral exploration justified in endoscopic total extraperitoneal repair of clinical unilateral groin hernias: a prospective cohort study. Int J Surg 36(Pt A):206–211. https://doi.org/10.1016/j.ijsu.2016.10.012
van den Heuvel B, Beudeker N, van den Broek J, Bogte A, Dwars BJ (2013) The incidence and natural course of occult inguinal hernias during TAPP repair: repair is beneficial. Surg Endosc 27(11):4142–4146. https://doi.org/10.1007/s00464-013-3008-2
Zendejas B, Onkendi EO, Brahmbhatt RD, Greenlee SM, Lohse CM, Farley DR (2011) Contralateral metachronous inguinal hernias in adults: role for prophylaxis during the TEP repair. Hernia 15(4):403–408. https://doi.org/10.1007/s10029-011-0784-2
Sayad P, Abdo Z, Cacchione R, Ferzli G (2000) Incidence of incipient contralateral hernia during laparoscopic hernia repair. Surg Endosc 14(6):543–545
Griffin KJ, Harris S, Tang TY, Skelton N, Reed JB, Harris AM (2010) Incidence of contralateral occult inguinal hernia found at the time of laparoscopic trans-abdominal pre-peritoneal (TAPP) repair. Hernia 14(4):345–349. https://doi.org/10.1007/s10029-010-0651-6
Bochkarev V, Ringley C, Vitamvas M, Oleynikov D (2007) Bilateral laparoscopic inguinal hernia repair in patients with occult contralateral inguinal defects. Surg Endosc 21(5):734–736. https://doi.org/10.1007/s00464-007-9196-x
Panton ON, Panton RJ (1994) Laparoscopic hernia repair. Am J Surg 167(5):535–537
Koehler RH (2002) Diagnosing the occult contralateral inguinal hernia. Surg Endosc 16(3):512–520. https://doi.org/10.1007/s00464-001-8166-y
Uchida H, Matsumoto T, Ijichi H, Endo Y, Koga T, Takeuchi H, Kusumoto T, Muto Y, Kitano S (2010) Contralateral occurrence after laparoscopic total extraperitoneal hernia repair for unilateral inguinal hernia. Hernia 14(5):481–484. https://doi.org/10.1007/s10029-010-0690-z
Ferzli GS, Shapiro K, DeTurris SV, Sayad P, Patel S, Graham A, Chaudry G (2004) Totally extraperitoneal (TEP) hernia repair after an original TEPIs it safe, and is it even possible? Surg Endosc 18(3):526–528. https://doi.org/10.1007/s00464-003-8211-0
Wauschkuhn CA, Schwarz J, Boekeler U, Bittner R (2010) Laparoscopic inguinal hernia repair: gold standard in bilateral hernia repair? Results of more than 2800 patients in comparison to literature. Surg Endosc 24(12):3026–3030. https://doi.org/10.1007/s00464-010-1079-x
Kockerling F, Schug-Pass C, Adolf D, Keller T, Kuthe A (2015) Bilateral and unilateral total extraperitoneal inguinal hernia repair (TEP) have equivalent early outcomes: analysis of 9395 cases. World J Surg 39(8):1887–1894. https://doi.org/10.1007/s00268-015-3055-z
Manangi M, Shivashankar S, Vijayakumar A (2014) Chronic pain after inguinal hernia repair. Int Sch Res Notices 2014:839681. https://doi.org/10.1155/2014/839681
Robinson A, Light D, Kasim A, Nice C (2013) A systematic review and meta-analysis of the role of radiology in the diagnosis of occult inguinal hernia. Surg Endosc 27(1):11–18. https://doi.org/10.1007/s00464-012-2412-3
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Drs. Ching-Chung Chiang, Hsin-Yi Yang and Yu-Chen Hsu have no conflicts of interest or financial ties to disclose.
Ethical approval
This study was approved by the CYCH Institutional Review Board.
Human and animal rights
Human Experimental Ethical Inspection was approval by Institutional Review Board of Chia-Yi Christian Hospital.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Chiang, CC., Yang, HY. & Hsu, YC. What happens after no contralateral exploration in total extraperitoneal (TEP) herniorrhaphy of clinical unilateral inguinal hernias?. Hernia 22, 533–540 (2018). https://doi.org/10.1007/s10029-018-1752-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-018-1752-x