Abstract
Background
Umbilical hernias present commonly during pregnancy secondary to increased intra-abdominal pressure. As a result, umbilical hernia incarceration or strangulation may affect pregnant females. The purpose of this study is to detail the operative management and 30-day outcomes of umbilical hernias in pregnant patients using the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP).
Methods
All female patients undergoing umbilical hernia repair during pregnancy were identified within the ACS-NSQIP. Preoperative patient variables, intraoperative variables, and 30-day patient morbidity and mortality outcomes were investigated using a variety of statistical tests.
Results
A total of 126 pregnant patients underwent umbilical hernia repair from 2005 to 2014; 73 (58%) had incarceration or strangulation at the time of surgical intervention. The majority of patients (95%) underwent open umbilical hernia repair. Superficial surgical site infection was the most common morbidity in patients undergoing open umbilical hernia repair.
Conclusions
Based on review of the ACS-NSQIP database, the incidence of umbilical hernia repair during pregnancy is very low; however, the majority of patients required repair for incarceration of strangulation. When symptoms develop, these hernias can be repaired with minimal 30-day morbidity to the mother. Additional studies are needed to determine the long-term recurrence rate of umbilical hernia repairs performed in pregnant patients and the effects of surgical intervention and approach on the fetus.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary umbilical hernias account for 175,000 general surgery cases annually in the United States [1]. Increased intra-abdominal pressure is a known risk factor for the development of primary umbilical hernias [2]. Unlike groin hernias, primary umbilical hernias are far more common in women and this observation may be at least partially related to periods of increased intra-abdominal pressure in the pregnant female [2].
Approximately, four million live births occur annually in the United States with the risk of acute abdomen requiring prompt surgical intervention in pregnant women approaching nearly 1 in 500 pregnancies [3, 4]. Pregnant women present unique challenges regardless of operative or nonoperative treatment. Nonoperative management of primary umbilical hernias during pregnancy increases the risk for progression to bowel incarceration and strangulation while operative intervention exposes the mother and fetus to increased physiologic stress and potentially teratogenic medications [1].
The two most common causes of non-obstetric acute abdomen, appendicitis and biliary pathology, have been described previously [3, 5]. Nevertheless, there remains a paucity of literature detailing the incidence and treatment of other general surgery emergencies in the pregnant patient. The purpose of our study is to detail the operative management and 30-day morbidity of umbilical hernias repaired during pregnancy as reported in the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP).
Materials and methods
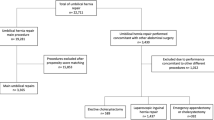
Pregnant women undergoing umbilical hernia repair from the years 2005–2014 were identified within the ACS-NSQIP database. Specifically, within the ACS-NSQIP database is a ‘pregnancy’ variable that is entered ‘yes’ if a patient undergoing surgery has a positive urine or blood test for pregnancy, if the fetus is visualized by ultrasound prior to surgery, or if there is evidence of a fetal heart rate by either ultrasound or fetal heart monitoring [6]. Only those patients with the pregnancy variable encoded ‘yes’ within the ACS-NSQIP database with one of the following Current Procedural Terminology (CPT) codes were included. Open umbilical hernias were identified by CPT Codes 49585 (reducible) and 49587 (incarcerated/strangulated) while laparoscopic umbilical hernias were identified by CPT Codes 49652 (reducible) and 49653 (incarcerated/strangulated). The use of mesh in open or umbilical hernia repair was identified by the CPT Code 49568. There is no separate CPT code for the use of mesh in laparoscopic umbilical hernia repair.
Preoperative patient variables, intraoperative variables, and 30-day postoperative morbidity and mortality variables available within the NSQIP database were investigated in this patient population. Thirty-day outcomes, including acute myocardial infarction, cardiac arrest, pneumonia, prolonged intubation, reintubation, venous thromboembolism, superficial surgical site infection, deep wound infection, organ space infection, wound dehiscence, bleeding requiring transfusion, urinary tract infection, sepsis, unplanned return to the operating room, and 30-day mortality, were detailed for patients who underwent either open or laparoscopic umbilical hernia repair. Fisher’s exact test is used for categorical variables and student’s t test and Kruskal–Wallis test for continuous variables. All data analysis was done using SAS version 9.3 and p < 0.05 was considered statistically significant.
Results
A total of 126 pregnant women underwent umbilical hernia repair from 2005 to 2014. One hundred and twenty (95%) patients underwent open umbilical hernia repair; 71 (59%) of these patients had umbilical hernia incarceration or strangulation at the time of operation. Six (5%) patients underwent laparoscopic umbilical hernia repair; 2 (33%) of these patients had umbilical hernia incarceration or strangulation at the time of operation. A total of 20 (16%) patients underwent simultaneous umbilical hernia repair at the time of another procedure; 16 (80%) underwent open umbilical hernia repair while 4 (20%) underwent laparoscopic umbilical hernia repair. Sixteen (80%) patients who underwent concomitant umbilical hernia repair had an asymptomatic umbilical hernia, while four (20%) had an incarcerated or strangulated hernia. Laparoscopic appendectomy (n = 5, 25%) and laparoscopic cholecystectomy (n = 9, 45%) were the most common concurrent procedures. No patient underwent umbilical hernia repair at the time of cesarean section.
The average age of all patients was 30.3 years and the average body mass index at the time of surgical intervention was 30.7 kg/m2. A majority of patients were Caucasian and very few patients had associated comorbidities. The average operating time for those patients who underwent open umbilical hernia repair was 41.2 ± 24.3 min and 41.3 ± 25.2 min for the laparoscopic group. Three (3%) patients underwent open umbilical hernia repair with mesh. The CPT code for laparoscopic umbilical hernia repair includes repair both with and without mesh so we are unable to delineate how many patients underwent laparoscopic hernia repair with mesh.
In terms of 30-day outcomes, the average length of stay for all patients was 1.3 days. A total of four (3%) patients experienced a superficial surgical site infection, three (2%) patients experienced a postoperative urinary tract infection, one (1%) patient experienced postoperative sepsis, and three (2%) patients had an unplanned return to the operating room. For the patients who returned to the operating room, it is unknown if their reoperation was related to their index procedure or related to their pregnancy (i.e., preterm labor, cesarean section). No patients experienced an acute myocardial infarction, cardiac arrest, pneumonia, prolonged intubation, venous thromboembolism, deep wound infection, organ space infection, or wound dehiscence.
Discussion
This study represents the largest series in the literature of umbilical hernia repair in pregnant patients detailing the operative approach and 30-day outcomes. While appendicitis and biliary disease are the two most common non-obstetric causes of acute abdomen in the pregnant patient symptomatic umbilical hernias are also common in this population and present a unique challenge to general surgeons [3]. Unfortunately, there is a paucity of data available to aid surgeons in discussing expected outcomes with these patients. This study demonstrates that pregnant patients with an umbilical hernia and signs of incarceration or strangulation can safely undergo umbilical hernia repair without significant morbidity or mortality to the mother.
The incidence of umbilical hernia incarceration or strangulation during pregnancy is not well known. In a small study by Buch et al. [1], 12 female patients with a known umbilical or groin hernia were followed through the course of their pregnancies. No patient developed hernia incarceration or strangulation and no patient required emergency hernia repair during pregnancy [1]. All patients underwent hernia repair postpartum. Based on their observations, the authors concluded that umbilical and groin hernias in pregnant patients should be managed with watchful waiting during pregnancy with planned surgical intervention postpartum [1]. Using a large, nationwide database, our study suggests that a certain percentage of these pregnant patients will require surgical intervention. Of the 126 patients included in our study, 73 (58%) had a diagnosis of incarceration or strangulation at the time of umbilical hernia repair. The potential for hernia incarceration and strangulation must be considered by the general surgeon when determining the timing of umbilical hernia repair in women of child-bearing age. Unfortunately, this dataset has a limited ability to predict which patients go on to develop incarceration or strangulation. Considering that over a ten-year period only 126 pregnant patients required umbilical hernia repair, the assumption is that few patients actually require repair. Without knowing how many patients had umbilical hernias that did not require operative intervention during their pregnancy, it is difficult to make a solid recommendation on who should get an operation. However, this data does contrast the conclusion by Buch et al. [1], and allows general surgeons to better inform pregnant patients about the potential for emergent surgery for incarceration or strangulation during pregnancy. Additionally, this study demonstrates minimal 30-day morbidity for the mother and thus patients who are symptomatic should be considered for repair prior to completion of their pregnancy. This recommendation is further supported by a recent systematic review by Jensen et al. who found that repair of symptomatic abdominal wall hernias at the time of pregnancy or during cesarean section is safe [7].
This systematic review not only supports this recommendation, but it highlights the paucity of data currently available in the literature. Jensen et al. [7] systematically reviewed Pubmed and Embase using the terms ‘abdominal wall hernias’ and’ pregnancy’. Within the literature, they did not find a single randomized controlled trial, prospective analysis, or retrospective case series on the topic of abdominal wall hernia repair during pregnancy. However, they did identify 12 case reports of emergent abdominal wall hernia repair during pregnancy. Of these 12 cases, seven were umbilical hernias, of which six underwent primary repair and one patient had a mesh repair. While our study does have limitations on the amount of operative details due to the inherent nature of the ACS-NSQIP database, it is nonetheless the largest case series of umbilical hernia repair during pregnancy currently available to inform surgeons on this clinical scenario.
A recent study by Oma et al. [8] followed 224 female patients who went on to become pregnant following primary umbilical hernia repair. Although previous studies have shown a lower recurrence rate with mesh versus primary repair in non-pregnant patients, this study found no difference in hernia recurrence rate at an average follow-up time of 3.8 years in female patients who went on to become pregnant regardless of surgical approach [8,9,10]. Only a small percentage of patients in our study underwent umbilical hernia repair with mesh. Although not well described in the literature, there are several reasons that may explain the hesitancy to use mesh during hernia repair in a pregnant patient, including the risk of lateral detachment of the mesh or inadequate overlap of the hernia defect as the uterus continues to grow as well as mesh-associated pain [6].
General surgeons must be equipped to manage the pregnant patient who presents with a symptomatic umbilical hernia requiring acute surgical intervention. When faced with this scenario, a multi-disciplinary approach including the general surgeon, anesthesiologist, and obstetrician should be utilized. The risk for preterm labor and delivery following emergency surgical intervention in the pregnant patient is estimated to be 4% [11, 12]. Therefore, pregnant women who require acute surgical intervention should undergo surgery at an institution with neonatal capabilities. To minimize the risk of fetal stress and teratogenicity, surgical intervention should be delayed until the second trimester, if possible, and the use of local or regional anesthesia should be considered [13].
Despite these findings, our study does have limitations, some of which are inherent in using the ACS-NSQIP database. Pregnancy characteristics, including gestational age and trimester of surgical intervention, are not available within the ACS-NSQIP database. Similarly, hernia characteristics, including the size of the hernia defect and the use of mesh during laparoscopic umbilical hernia repair, are not detailed within the ACS-NSQIP database. Furthermore, while it would be nice to know if the open or laparoscopic surgical approach to umbilical hernia repair in this patient population leads to differences in 30-day morbidity, the incidence of laparoscopic umbilical hernia repair in this patient population is too small to make definitive conclusions. Additionally, the outcomes detailed within this manuscript are limited to maternal outcomes only as fetal outcomes are not available within the ACS-NSQIP database. Twenty patients underwent umbilical hernia repair at the time of laparoscopy for an alternative source of acute abdominal pathology. We are unable to determine if these patients had symptoms related to their umbilical hernia at the time of operation or if these hernias were incidentally discovered and repaired at the time of laparoscopy. Three patients returned to the operating room within 30 days of their original umbilical hernia repair and we are unable to determine if these re-operations were related to the index operation or related to pregnancy complications such as preterm labor or miscarriage. Finally, the ACS-NSQIP database only includes outcomes within the first 30 days postoperatively which limits our ability to make long-term conclusions regarding maternal and fetal health or hernia recurrence.
Conclusion
Based on review of the ACS-NSQIP database, the incidence of umbilical hernia repair during pregnancy is very low; however, the majority of patients required repair for incarceration of strangulation. When symptoms develop, these hernias can be repaired with minimal 30-day morbidity to the mother. Additional studies are needed to determine the long-term recurrence rate of umbilical hernia repairs performed in pregnant patients and the effects of surgical intervention and approach on the fetus.
References
Buch KE, Tabrizian P, Divino CM (2008) Management of hernias in pregnancy. J Am Coll Surg 207(4):539–542
Salameh JR (2008) Primary and unusual abdominal wall hernias. Surg Clin N Am 88(1):45–60
Augustin G, Majerovic M (2007) Non-obstetrical acute abdomen during pregnancy. Eur J Obstet Gynecol Reprod Biol 131(1):4–12
Pregnancy Statistics. http://www.statisticbrain.com/pregnancy-statistics/. Accessed April 5, 2017
Cox TC, Huntington CR, Blair LJ, Prasad T et al (2016) Laparoscopic appendectomy and cholecystectomy versus open: a study in 1999 pregnant patients. Surg Endosc 30:593–602
ACS NSQIP Participant Use Data File. https://www.facs.org/quality-programs/acs-nsqip/program-specifics/participant-use. Accessed July 14, 2016
Jensen KK, Henriksen NA, Jorgensen LN (2015) Abdominal wall hernia and pregnancy: a systematic review. Hernia 19(5):689–696
Oma E, Jensen KK, Jorgensen LN (2016) Recurrent umbilical or epigastric hernia during and after pregnancy: a nationwide cohort study. Surgery 159(6):1677–1683
Arroya A, Garcia P, Perez F, Andreu J et al (2001) Randomized clinical trial comparing suture and mesh repair of umbilical hernia in adults. Br J Surg 88(10):1321–1323
Sanjay P, Reid TD, Davies EL, Arumugam PJ et al (2005) Retrospective comparison of mesh and sutured repair for adult umbilical hernias. Hernia 9(3):248–251
Cohen-Kerem R, Railton C, Oren D, Lishner M et al (2005) Pregnancy outcome following non-obstetric surgical intervention. Am J Surg 190(3):467–473
Odibo I (2013) Non-obstetric surgery during pregnancy. powerpoint. Little Rock, AR: Division of Maternal-Fetal Medicine
VandeVelde M, DeBuck F (2007) Anesthesia for non-obstetric surgery in the pregnant patient. Minerva Anestesiol 73(4):235–240
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
INH declares no conflict of interest directly related to this work but is the recipient of the Americas Hernia Society Resident Research Grant. MJR declares no conflict of interest directly related to this work but is the Medical Director for the AHSQC, receives consulting fees for Bard and Artiste, and has received grant funding from Miromatrix and Intuitive Surgical, Inc. ASP declares no conflict of interest directly related to this work but is a consultant for Bard and MedTronic and has received grant funding from Intuitive Surgical, Inc. RLA declares no conflict of interest. SR declares no conflict of interest. FB declares no conflict of interest. DMK declares no conflict of interest.
Ethical approval
Ethical approval was not required for this study.
Human and animal rights
This study does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was not required for this study.
Rights and permissions
About this article
Cite this article
Haskins, I.N., Rosen, M.J., Prabhu, A.S. et al. Umbilical hernia repair in pregnant patients: review of the American College of Surgeons National Surgical Quality Improvement Program. Hernia 21, 767–770 (2017). https://doi.org/10.1007/s10029-017-1633-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-017-1633-8