Abstract
Background
Spigelian hernias are said to be a rare condition of the elderly population, usually arising below the arcuate line. Local experience has led us to challenge these commonly held beliefs.
Methods
Operations for Spigelian hernia from 2006–2016 were identified from the Edinburgh Lothian Surgical Audit computerised database and case notes were reviewed.
Results
One hundred and one patients underwent surgery for 107 Spigelian hernias in the 10-year period. The female-to-male ratio was 2:1. Ages ranged from 32 to 88 with a median of 64 years. Sixty-five operations were done open and 42 were laparoscopic. Twelve of the 27 for which the precise anatomic location was recorded were situated above the arcuate line. Twenty-nine hernias had small defects and comprised interstitial fat only with no peritoneal sac. Ages in this group ranged from 32 to 80 (median = 48 years). All presented with intermittent local pain and/or swelling, although in three patients the hernias were impalpable. Those three also underwent ultrasound, CT and/or laparoscopy, but the hernias were only identified after open surgical exploration. The remaining 78 cases had peritoneal sacs of varying size with defects up to 9 cm across, and all were identified on imaging and/or laparoscopy. Ages ranged from 38 to 88 (median = 67 years; p < 0.01). Eighteen patients presented as emergencies and all were in this group.
Conclusion
Spigelian hernias may be more common than we think and are probably under-diagnosed. They commonly arise above the arcuate line. We describe three clinical stages: Stage 1 hernias are those without peritoneal sacs and tend to arise in younger patients, can be difficult to diagnose and may not seen at laparoscopy. Stages 2 and 3 hernias arise in older patients, do have peritoneal sacs, are visible at laparoscopy and are more likely to present as emergencies. Stage three hernias are too large for laparoscopic repair. The differences between stages likely reflect the natural history of the condition, which begins as extraperitoneal fat protrusion and progresses over many years to develop a peritoneal sac.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spigelian hernia (SH) is said to be a rare condition of the elderly population, arising through an area of fascial deficiency in the lower abdomen just below the arcuate line. While they are most commonly seen in the elderly population [1–3], SH has been described in people of all ages, even neonates [4]. The name derives from Adriaan van de Speighel, sometimes written as Spigelius, a Flemish anatomist and surgeon who worked in Padua and died in 1626. He did not describe the hernia, but his name is associated with the fascial layer through which this hernia protrudes.
Most surgeons encounter no more than a handful of SH throughout their careers and few large series have been published. Much of what has been written about this condition is based on case reports and limited experience, and may be inaccurate owing to the perpetuation of old ideas and information. This review of 107 cases represents the largest series of SH reported to date and provides an update on the anatomical aspects, clinical presentation, imaging and current treatment options for SH in the era of CT scanning and laparoscopy.
Methods
Patients undergoing SH repair from February 2006 to February 2016 were identified from the Lothian Surgical Audit system, a prospectively maintained computer database of all surgical procedures in the Edinburgh region of south-east Scotland. Data including patient demographics, clinical presentation, location and size of fascial defect and surgical treatment were obtained from the hospital case notes. The choice of surgical treatment was at the discretion of the treating surgeon. The Mann–Whitney U and Chi-squared tests were used as appropriate to compare groups. Statistical significance was defined as p < 0.05.
Results
One hundred and seven SH were identified in 101 patients comprising 98 primary unilateral, three recurrent unilateral and three bilateral hernias. Adequate records were available for all of these. Sixty-six patients were female and 35 were male (ratio 2:1). Patients’ ages ranged from 32 to 88 with a median of 64 years. Defect sizes ranged from 1 × 1 to 6 × 9 cm in size. Fifty-one hernias were on the left, 48 on the right, three were bilateral, and there was no side recorded for two cases. Two hernias were superior to the umbilicus, one was level with it and the remaining 104 were in the lower abdomen. Altogether, 12 hernias were documented to be arising above (cephalad to) the arcuate line. In 15 cases, the defect was recorded as being below the arcuate line, and, in the remaining 77 cases, the precise location of the hernia in relation to the arcuate line was not recorded.
Eighteen hernias (17%) presented as an emergency, and, in 15 of these, the hernia was diagnosed preoperatively, as a palpable lump in 11 and seen on CT scan in four. In three cases, the hernias were found at operation as an unexpected finding. Nine presented with incarcerated small bowel, five with incarcerated omentum and one with incarcerated sigmoid colon. Three patients presented with acute painful hernias without incarceration.
Of the 89 elective hernias, 76 (85%) presented with symptoms of intermittent pain and swelling at the lateral edge of the rectus sheath. One patient presented initially with a femoral hernia, one with an umbilical hernia and two with inguinal hernias, and it was only during laparoscopy for these that concurrent, ipsilateral SH were found. Six further cases were operated on for suspected inguinal hernias and found to have SH instead. In each of these cases, the defect lay inferior to the arcuate line. One patient presented with a long history of intermittent right-sided lower abdominal pain but no mass; the hernia was diagnosed on CT scan. Finally, three patients described intermittent pain and swelling at the edge of the rectus sheath, although nothing was apparent on clinical examination. One brought a photograph she had taken herself (Fig. 1). Each of these three patients underwent normal ultrasound, CT and laparoscopy before their small interstitial SH was found at open operation.
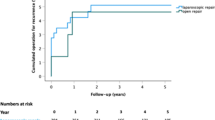
Sixty-five cases were operated on with open surgery and 42 laparoscopically. Three of the latter were converted to open surgery because no defect was visible at laparoscopy (see above). Four different laparoscopic techniques were employed, comprising 19 totally extraperitoneal (TEP) repairs, 11 intraperitoneal onlay mesh (IPOM), two transabdominal preperitoneal (TAPP) repairs and seven transabdominal partially extraperitoneal repairs [5, 6]. All of these operations involved the use of mesh. Four different open repair techniques were used: 24 with onlay mesh, 25 with mesh placed deep to the external oblique aponeurosis and extending medially into the retrorectus space, 11 suture-only repairs and five extraperitoneal mesh repairs.
At operation, 78 hernias had a peritoneal sac while in the remaining 29 cases the hernia comprised extraperitoneal fat only, with no peritoneal component. In those without a peritoneal sac, the median defect size was 1 × 1 cm (maximum size 2 × 2 cm) and the median age was 48 years (range 32–80). In contrast, the hernias with peritoneal sacs had a median defect size of 2.5 × 2.5 cm (maximum size 6 × 9 cm) and a median age of 67 years (range 38–88 years). These differences in defect size and age are statistically significant (see Table 1).
Discussion
The Lothian hospitals perform approximately 1500 hernia repairs per annum, of which 950 are inguinofemoral and 550 are ventral hernia repairs. At an average of nearly 11 per year in this series, SH therefore represents approximately 0.7% of all hernia repairs and 2.0% of all ventral hernia repairs in our region, which is consistent with other published reports [7, 8].
Anatomical aspects
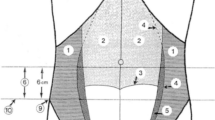
The musculoaponeurotic junction of the transversus abdominis (TA) muscle forms the linea semilunaris and runs in a gentle curve from the costal margin to the groin where it merges with the conjoined tendon (see Fig. 2). The lateral edge of the rectus sheath runs from the costal margin to the pubis and also follows a gentle curve. The Spigelian fascia extends between these two lines and comprises the fused aponeuroses of transversus abdominis and internal oblique (IO) muscles, although one or both of these layers are often muscular in the upper abdomen as they contribute to the posterior rectus sheath. The Spigelian fascia is crescentic in shape, widest just below the level of the umbilicus. The arcuate line, or semicircular fold of Douglas, runs across the lower abdomen and marks the inferior limit of the posterior rectus sheath. Below (caudal to) this line, all three lateral muscle aponeuroses run superficial to the rectus muscle.
A Spigelian hernia involves a defect in the Spigelian fascia, that is, both the transversus abdominis and the internal oblique fascial layers, with the external oblique layer remaining intact (see Fig. 3). This fact distinguishes SH from incisional hernias and also explains why these hernias are often hard to feel, and why they can be missed at open operation until the external oblique layer is opened. Why these hernias involve a defect in two of the three abdominal wall layers is subject to speculation. It has been suggested that they arise at the site of small perforating vessels, but these are not a consistent finding at operation [8]. It maybe because the fibres of IO and TA run almost parallel, especially in the lower abdomen, that they are more prone to split together. Perhaps people developing Spigelian hernias just happen to have congenital fusion of the IO and TA layers—although this was not the case in the CT scan shown in Fig. 3.
CT scan showing right-sided Spigelian hernia protruding through the TA and IO aponeuroses with EO intact. The TA and IO aponeuroses are clearly seen as separate layers. This hernia is above the arcuate line as the TA aponeurosis extends posterior to the rectus muscle (heavy arrow). EO external oblique, IO internal oblique, TA transversus abdominis
It has also been said that SH generally arises below the arcuate line because the lack of posterior rectus sheath there represents an area of relative weakness [9]. This concept had been disputed in the past [8], and indeed there is no reason why the arcuate line should represent an area of weakness: after all, the three layers of fascia are still present. In the present series, 12 of the 27 cases in which the precise location of the hernia was recorded were seen to protrude above (cephalad to) the arcuate line. It is true that SH is most common in the so-called “spigelian belt” just below the level of the umbilicus [7, 10], but the defect may still lie above the arcuate line, as seen in Fig. 4. The Spigelian fascia is widest below the level of the umbilicus and therefore potentially at its weakest. Also, the abdominal girth is at its maximum at that level, so the wall tension will be greatest according to the law of La Place. Furthermore, in the upper abdomen, the TA and IO muscle bellies often extend medially into the posterior rectus sheath which makes the Spigelian fascia stronger and may help to explain why SH is less common above the umbilicus.
Development and progression of SH
Cases arising in babies and children may represent a congenital failure of fusion of mesenchymal layers, and, in this age group, they are often associated with cryptorchidism [4]. Adult hernias, however, are probably acquired. Our series shows that they are generally smaller in younger adults than in the elderly, and less likely to have a peritoneal sac, which suggests that there is a natural progression. As suggested by others [9, 11, 12], SH may begin with a small split in the fascial layers through which only extraperitoneal fat protrudes initially. Such early hernias are likely to be small and may present with pain for some time—perhaps years—before a lump is found. Such small hernias would not be visible at conventional laparoscopy, and indeed this was the case in three of the patients in this series. With time, these small interstitial hernias enlarge, become more easily palpable and develop a peritoneal sac. At this stage, they may entrap bowel or omentum and present as an emergency. With a peritoneal sac, they also become amenable to transperitoneal laparoscopic diagnosis and treatment.
Such a natural progression might also explain why SH appears to be more common in older patients. It may be simply that the hernias have been there for longer, and are consequently larger and easier to detect, in that age group.
Clinical features
Patients usually present with pain, localised swelling or both. Emergency presentation with obstruction or strangulation has been described in 10–29% of cases [10, 13], and in the present series it was 17%. Younger adults with smaller hernias are more likely to present with pain only, although a deep swelling may be palpable in some of these. If the hernia is entirely interstitial, however, there may be no lump to feel. If a lump is palpable, it may or may not be reducible. Typically, the fascial defect is smaller than the sac so irreducibility is common, and hence the propensity for emergency presentation.
Diagnosis
Palpable swelling
In a patient with a reducible swelling and cough impulse just lateral to the rectus sheath, the diagnosis is Spigelian hernia—or perhaps an incisional hernia related to a nearby scar (including laparoscopic port or drain-tube sites). In the presence of a stoma, it may be a parastomal hernia. Imaging is not required to confirm the diagnosis, although it may be useful to plan the surgical approach (see below).
As with other hernias, the appearance of the swelling is often associated with physical activity and often disappears with rest, sometimes suddenly and with a “popping” sensation. A cough impulse may be absent, especially if the defect is small. If the swelling is irreducible, the differential lies between a hernia and some other soft tissue swelling such as lipoma. Imaging may be useful before treatment is planned. Ultrasound is operator-dependent: it may clearly show a fascial defect and protruding tissue but absence of these features does not exclude hernia. CT or MRI scan may be preferred and some form of biopsy may be appropriate if a solid tumour is suspected.
No palpable swelling
In cases with the absence of palpable swelling, the need for investigation is based on clinical suspicion alone. Ultrasound, CT or MRI scanning may be performed, but in the absence of a palpable swelling these tests are likely to be normal. If a Spigelian hernia is present, it will be small and probably interstitial, protected from the examining hand by the tough and smooth external oblique layer, and in some obese individuals even a large hernia may be difficult to feel through the thick subcutaneous fat layer.
Transperitoneal laparoscopy is useful for both diagnosis and treatment but will only identify hernias with a peritoneal sac. Hernias comprising interstitial fat only, which in our experience are the most common type of SH seen in patients under the age of 55, are not visible this way. They may be identifiable with totally extraperitoneal laparoscopy but this would be an unusual investigation to perform in a patient presenting with lower abdominal pain, and furthermore hernias arising above the arcuate line would be difficult or impossible to see from within the retrorectus space. They may be diagnosed incidentally, however, if totally extraperitoneal laparoscopy is being performed for some other reason such as a suspected inguinal hernia. This occurred in eight cases in the present series and has also been described by Dulucq et al. [14]. If the diagnosis of a small interstitial SH is suspected strongly enough, an open approach should reliably find it.
Treatment
Surgery is the only effective treatment and is recommended in most patients because of high risk of acute presentation, although some patients with asymptomatic hernias and significant medical co-morbidities may be better treated conservatively.
Surgical repair may be laparoscopic or open. We suggest that the technique of choice depends on the experience of the surgeon, the patient’s fitness for surgery and the clinical “stage” of the hernia as follows:
Stage I: The hernia contents comprise interstitial fat only with no peritoneal component (Fig. 5). This is typically a patient at the younger end of the age spectrum who presents with intermittent, well-localised pain suggestive of hernia, but no palpable swelling. If present, any swelling will be small and irreducible. These should be treated by open surgery because they are not visible laparoscopically. The site must be carefully identified and marked on the skin preoperatively. At operation, the surgeon may be initially dismayed to find nothing, but exploration is only complete after the external oblique has been opened, as well as internal oblique and even the rectus sheath if necessary, to explore all the musculofascial layers. The defect is usually small, less than 2 cm in maximum dimension. If mesh is to be employed, it can be placed extraperitoneally or in the retromuscular plane which extends between the retrorectus space medially and the plane deep to external oblique laterally. The subcutaneous (onlay) plane may also be used, but this risks mesh exposure in the event of wound infection or breakdown.
Stage II: A peritoneal component is present and the defect is moderate in size, say up to 5 cm in diameter (Fig. 4). The patient may be any age. A swelling is likely to be palpable and may or may not have a cough impulse, or be reducible. These can be treated either laparoscopically or open depending on the preference of the surgeon. Laparoscopic totally extraperitoneal repair is only applicable to hernias arising below the arcuate line. Transperitoneal laparoscopic repair may be IPOM or TAPP, but because of the risk of neurovascular injury from tacks fired into the posterolateral abdominal wall, a partially extraperitoneal repair [5, 6] is a good option. Small hernia defects may be manageable by laparoscopic suture alone [2].
Stage III: A large hernia with significant distortion of the abdominal wall (Fig. 6). The patient is usually older and the defect is likely to be more than 5 cm in diameter, with a sac much larger than this. These hernias will be easily palpable and may or may not be reducible. They are often too large for laparoscopic repair either because the working space is lost once the hernia contents are reduced, or because the defect is too large for secure coverage [15]. These are best treated with an open repair which may involve a degree of abdominal wall reconstruction with or without excision of redundant skin. Because of their lateral location, components separation techniques are not applicable, but the peritoneal flap hernioplasty [16] is very useful in these cases.
Conclusion
This is the largest series of Spigelian hernia reported to date. It is an uncommon hernia but not rare, comprising approximately 2% of ventral hernias treated at our hospital over the study period. Considering that 10/107 (9%) of elective SH were found incidentally and another 18/107 (17%) presented for the first time as emergencies, it is likely that SH is under-diagnosed and therefore more common than we think. There should be a high risk of suspicion when a patient complains of pain with or without a swelling in the regions of the Spigelian belt. This series also shows that acquired SH is not a disease of the elderly, as the median age at presentation was 64 years and 25/107 hernias (23%) were diagnosed in patients below the age of 50. Thirdly, it confirms that the SH is not confined to the so-called weak area below (caudal to) the arcuate line, as 12/27 (44%) of the cases in which the precise location of the hernia was recorded in this series were seen to arise above this level.
Definitive surgical treatment for SH is recommended because of high risk of incarceration. A variety of laparoscopic and open repair techniques are available. In the modern era, the availability of CT scanning and laparoscopy allows the diagnosis and precise anatomy to be confirmed and a tailored surgical approach to be planned.
References
Spangen L (1989) Spigelian Hernia. World J Surg 13:573–580
Bittner JG IV, Edwards MA, Shah MB, MacFadyen Jr BV, Mellinger JD (2008) Mesh-free laparoscopic Spigelian hernia repair. Am Surg 74:713–720
Moreno-Egea A, Campillo-Soto A, Norales-Cuenca G (2015) Which should be the gold standard laparoscopic technique for handling Spigelian hernias? Surg Endosc 29:856–862
Jones BC, Hutson JM (2015) The syndrome of Spigelian hernia and cryptorchidism: a review of the paediatric literature. J Paediatr Surg 50:325–330
Sharma A, Dey A, Khullar R, Soni V, Baijal M, Chowbey PK (2011) Laparoscopic repair of suprapubic hernias: transabdominal partial extraperitoneal (TAPE) technique. Surg Endosc 25:2147–2152
Brady RR, Ventham NT, de Beaux AC, Tulloh B (2014) Laparoscopic partially extraperitoneal (PEP) mesh repair for laterally placed ventral and incisional hernias. Surg laparosc Endosc Percutan Tech 24:99–100
Skandalakis PN, Zoras O, Skandalakis JE, Mirilas P (2006) Spigelian Hernia: surgical anatomy, embryology, and technique of repair. Amm Surg 72:42–48
Read RC (1960) Observations on the etiology of Spigelian hernia. Ann Surg 152:1004–1009
Mittal T, Kumar V, Khullar R, Sharma A, Soni V, Baijal M, Chowbey PK (2008) Diagnosis and management of Spigelian hernia: A review of literature and our experience. J Min Access Surg 4:95–98
Polistina FA, Garbo G, Trevisan P, Frego M (2015) Twelve years of experience treating Spigelian hernia. Surgeryu 157:547–550
River LP (1942) Spigelian Hernia. Ann Surg 116:405
Zimmerman LM, Anson BJ, Morgan EH, McVay CB (1944) Ventral Hernia due to normal banding of the abdominal muscles. Surg Gynaec Obst 78:535
Larson DW, Farley DR (2002) Spigelian hernias: repair and outcome for 81 patients. World J Surg 26:1277–1281
Dulucq JL, Wintringer P, Mahajna A (2011) Occult hernias detected by laparoscopic totally extraperitoneal inguinal hernia repair: a prospective study. Hernia 15:399–402
Tulloh B, de Beaux AC (2016) Defects and donuts: the importance of the mesh:defect area ratio. Hernia 20:893–895
Malik A, Macdonald ADH, de Beaux AC, Tulloh BR (2014) The peritoneal flap hernioplasty for repair of large ventral and incisional hernias. Hernia 18:39–45
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
BT declares conflict of interest not directly related to the submitted work. All the remaining authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by the authors.
Rights and permissions
About this article
Cite this article
Webber, V., Low, C., Skipworth, R.J.E. et al. Contemporary thoughts on the management of Spigelian hernia. Hernia 21, 355–361 (2017). https://doi.org/10.1007/s10029-017-1579-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-017-1579-x