Abstract
Purpose
Knowledge about suture tension dynamics after laparotomy closure is limited due to the lack of adequate measurement tools. As a consequence, a miniaturized implantable sensor and data logger were developed and applied experimentally in a porcine model to measure suture tension dynamics after laparotomy closure.
Material and methods
We developed an implantable device (6 × 3 × 1 mm) fitted with silicon strain gauges and an implantable data logger allowing long-term registration. In nine domestic pigs, sensors and loggers were implanted along the suture closing a median laparotomy registering suture tension over a period of 23 h.
Results
Fascial closure was achieved by a mean suture tension of 1.07 N. After 30 minutes, suture tension was reduced to 0.81N (−24.3 %, p = 0.0003). After 12 h, tension showed a further decrease to 0.69 N (−35.5 %, n.s.), after 23 h mean suture tension reached 0.56 N, (−47.7 %, p = 0.014).
Conclusions
The aim to develop an implantable miniaturized sensor device registering long-term suture tension dynamics was achieved. The use in the animal experiment was feasible and safe. We observed a loss of almost 50 % of suture tension 23 h after fascial closure. This could mean that up to 50 % of initial suture tension may be an unnecessary surplus not contributing to tissue stability but to the risk of suture failure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laparotomy closure is a routine procedure in abdominal surgery. Although surgical techniques are highly standardized and in spite of modern suture materials and advanced supportive medical care, the failure rate of laparotomy closure remains constantly high. Incisional hernia occurs with a rate of about 15 % [1] and is the most frequent complication in abdominal surgery requiring re-operation. Endogenous risk factors for incisional hernia development have been investigated but they can hardly be influenced by the surgeon [2]. Exogenous risk factors have also been identified and numerous efforts have been undertaken to eliminate them. Running continuous sutures with a suture-length to wound-length ratio of ≥4 have been proven to be advantageous [3, 4] and excessive suture tension leading to tissue strangulation and necrosis should be avoided [5]. The negative effects of excessive suture tension on tissue regeneration have previously been investigated using laser-fluorescence-angiography and collagen content analysis in an animal model. Increased suture tension resulted in reduced blood supply of the incisional region and an abnormal collagen I/III ratio in the scar tissue [6, 7]. The registration and standardization of tension during the application of sutures (the mainstay of surgical action) have, however, only occasionally been investigated. In one experiment, in which we asked surgeons to tie knots while measuring the applied suture tension, we demonstrated the incapability of surgeons to control suture tension manually [8].
Currently, no implantable sensor device exists which allows long-term registration of suture tension. We neither have reliable information about the dynamics of suture tension after a suture has been accomplished nor a data base allowing us to define ‘adequate’ suture tension for fascial closure. As a consequence, a miniaturized implantable sensor device and data logger were developed and applied experimentally to learn more about the dynamics of the incised abdominal wall with the future aim to adjust suture tension to a tissue specific optimum and to reduce the incidence of incisional hernias.
Theoretical background
The main task of sutures is to approximate incised edges of tissue and the surgeon adjusts the suture tension to a level which secures close tissue approximation without tissue overlap. Sutures to close the abdominal wall pass through tissues of different mechanical stability. Abdominal fascias consist mainly of mechanically stable collagen while fatty tissue and muscles have no relevant mechanical stability to withstand the cutting force of a suture. While the sutures approximate the incisional edges, the muscles of the abdominal wall, postoperative abdominal distension, Valsalva manoeuvres, coughing, etc. exert a largely variable tearing force.
Materials and methods
Sensor device requirement specifications
The approximate stitch length of 10 mm to each side of the incision and stitch intervals between 10 and 15 mm for fascial closure defined the dimensions of a sensor that should not exceed 10 × 5 × 5 mm to avoid interference and blockade by surrounding tissues as well as triangulation effects. The construction of the device should allow positioning ‘on the thread’ to reduce external interfering factors. An in vitro feasibility study using a load cell defined the required measuring range between 0 and 3 N with an overload capability (maximum applicable force without damage to the sensor or influence on calibration) of 20 N to avoid damage to the sensor by high short time signals [9]. To allow long-term registration, an implantable data logger registering suture tensions every second and an external connect board to read out the data were deemed necessary. The development process was realized in collaboration between the Fraunhofer Institute for Production Technology in Aachen, Germany and the Department of Surgery, Technical University (RWTH) Aachen, Germany.
Animal housing and experiments
For the underlying investigation, six domestic male pigs with a mean body weight of 51.3 ± 4.9 kg (mean ± SD) were examined during 24 h. These animals also served as control animals in an experiment on the effects of intra-abdominal hypertension. Three more domestic male pigs from the intervention group of the same experiment with a mean body weight of 51.1 ± 4.8 kg (mean ± SD) were examined over 30 min and thereafter underwent a research protocol with elevated intra-abdominal pressure, the results of which have been reported elsewhere [10]. The research protocol was approved by the regional animal welfare committee and the district government (File Number 50.203.2-AC18, 53/02).
Experiments were carried out under supervision of a veterinarian at the Institute of Laboratory Animal Science, Technical University (RWTH) Aachen, Germany.
The animals were fasted for 24 h before the intervention period with free access to water. General anaesthesia was induced and maintained with ketamine and pentobarbital. Muscle relaxants were not administered throughout the experiment. The animals were placed in supine position. Volume-controlled ventilation with an inspiratory oxygen concentration of 25 % and a positive end-expiratory pressure of 2 cm H2O was used (Servo 900 C ventilator, Siemens, Solna, Sweden). At a constant respiratory rate of 15 breaths/min, the ventilatory setting was adjusted to maintain a PCO2 between 35 and 40 mm Hg. These settings remained unchanged throughout the experiment. Heart rate was recorded continuously with a three-channel ECG. Normal saline was infused at a constant rate of 1.5 ml/kg using an automatic infusion device (B.Braun Melsungen, Germany). A core temperature of 36–38 °C was maintained by application of heating lamps. Urine output was recorded via a suprapubic catheterization. A3-French thermistor tipped fiberoptic catheter (PV 2023 Pulsion Medical Systems, Munich, Germany) capable of thermal dye dilution measurements was placed in the descending aorta via the femoral artery. In addition, an 18-gauge catheter and a large-bore dialysis catheter (Arrow, Reading, PA) were placed in the carotid artery and the superior vena cava.
Urine output was recorded via a suprapubic catheterization. For safe placement of urine catheter and a 10 mm laparoscopy trocar, a 14 cm median skin incision was made at the level of the umbilicus. A strictly median 12 cm fascial and peritoneal incision was then performed. Both, laparoscopy trocar and suprapubic insertion cannula were placed under vision and via separate abdominal wall perforations. The urinary catheter was placed intravesically via puncture and secured with a purse string suture.
The fascia was then closed with size 1 running Vicryl (Ethicon, Norderstedt, Germany) omitting the peritoneum and as far as possible the rectus muscle. The distance of stitches to the incisional edges was kept at 1 cm to each side, the stitch intervals at 10 mm. After the fourth stitch and after the eighth stitch of the fascial suture, a sensor device designed to measure suture tension was threaded on the suture which was then accomplished and finished with a self-locking knot. Two sensors were used in each animal to serve as internal controls, to permit tension measurement along the suture and to visualize equalization of tension peaks that might occur during the experiments. Suture tension was adjusted to a level which secured close approximation of the incisional edges without tissue overlap. A subcutaneous pocket was then prepared adjacent to the laparotomy to house the data logger. The skin was closed by single sutures with 3-0 Vicryl and covered with a sterile dressing.
This was followed by laparoscopy performed via the previously inserted trocar in the left upper abdominal quadrant to rule out intra-abdominal haemorrhage. The pneumoperitoneum was then released with the trocar left in situ.
After an equilibration period of 1 h the registration of suture tension was started with measurement intervals of 1 s. After 24 h, the animals were killed by an overdose of pentobarbital and a necropsy performed in order to search for device-related adverse events. The sensors and data loggers were explanted and the data read out to undergo further analysis.
Statistical analysis
Suture tension dynamics were statistically analysed at different timepoints (initial tension versus tension after 30 min, 30 min vs. 12 h and 12 vs. 23 h) applying the paired two sided t test of repeated measurements one-way ANOVA. Differences were considered significant at a level of 5 %. Statistics were calculated using GraphPad Prism® version 6.04.
Results
Sensor realization
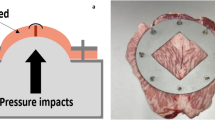
Applying CAD and FEM-model simulation, a bending beam construction milled out of solid aluminium in a U-shaped configuration was developed measuring 6 × 3 × 1 mm. The transverse beam of the bending beam was fitted with four matched silicon strain gauges [two on the upper and two on the lower surface under the microscope (Fig. 1)].
Sprocket holes attached to both vertical beams of the device together with integrated guides on the horizontal beam secured the guiding of the thread over the sensor and an exact positioning during the entire measurement period.
An implantable two channel 16 bit data logger was also built in multi-layer technique with a 256 kByte RAM allowing variable measurement sampling intervals. The data logger had a diameter of 25 mm and a thickness of 3 mm. The data loggers were encapsulated into polycrystalline wax to reduce tissue reaction during long-term studies. The connect board to read out the data storage of the logger allowed data transfer with Hyperterminal 4.0 (multi-threades TTY sample for Win32) for data processing with a conventional PC.
Contour accuracy and sensitivity during testing revealed the sensors suitable for force signals expected in laparotomy closure. All sensors underwent an offline calibration in a spring-load-calibrator. 15 measurements were taken in each direction from 0 to 3 N and from 3 to 0 N to perform the basic calibration. All sensors underwent a further five-point calibration with a standard load of 1 N immediately before implantation and a check for accuracy of measurement immediately after explantation.
Experimental use
Sensor and data logger function
The implantation and function of the device caused no adverse effects like bleeding, inflammation or tissue necrosis as investigated during necropsy. Cutting of sutures through the incisional edges was not observed.
Of the 12 sensor devices used in the 23 h experiment, eight sensors in four animals registered suture tension throughout the entire period (approx. 83500 registered measurements each), two sensors in one animal did not register suture tension at all and one sensor in another animal malfunctioned after 30 min. The animals with only one sensor functioning were also excluded from further analysis. Of the six sensors used in the half-hour experiment none showed a sensor defect (approx. 1800 measurements each) (Fig. 2). Malfunction occurred due to solder breakage as cables connecting sensor and data logger had a diameter of only 0.1 mm.
All nine data loggers worked as expected and reading out the data via the external connect board proved uneventful in all cases.
Suture tension dynamics
Analysis of suture tension dynamics revealed decreasing suture tension beginning immediately after fascial closure continuing until the end of the experiment after 23 h. When a suture tension of below 1 N was applied for fascial closure, values of the two sensors implanted into each animal showed an almost parallel curve progression (sensors bb001-1 and bb001-2; sensors bc001-1 and bc001-2) while in fascial closure with a tension above 1 N and a more marked difference of suture tension along the suture line, curves showed a pronounced convergence beginning 30 min after fascial closure continuing until the end of the experiment (sensors be001-1 and be001-2; sensors bf001-1 and bf001-2) (Fig. 3).
To ensure close contact of the incisional edges of the laparotomy without tissue overlap, a mean initial suture tension of 1.07 N (range 0.41–3.18 N) had to be applied. After 30 min, mean tension had reduced to 0.81 N (range 0.11–2.90 N; p = 0.0003), a reduction of 24.3 % compared to the initial tension. After 12 h, mean suture tension was 0.69 N (range 0.26–1.85 N; n. s.; p = 0.15). After 23 h, mean suture tension was 0.56 N (range 0.16–1.36 N; p = 0.014), a loss of 47.7 % when compared to initial suture tension (Fig. 4).
Discussion
This experiment reached its primary aim to develop an implantable miniaturized sensor device and its secondary aim to register long-term suture tension dynamics.
The implanted device is not the result of serial production and currently no comparable product is available on the market. Malfunction due to solder breakage occurred in 3 out of 12 sensors. As cables connecting sensor and data logger had a diameter of only 0.1 mm, even minor mishandling during implantation might have caused the failure in function. It can be expected, however, that registered data were reliable and further research and development are likely to overcome the fragility.
Although interpretation of results is limited by the small number of registered curves, they showed a statistically significant decrease of suture tension in the first 30 min after fascial closure, followed by a slow but also statistically significant transgression into a plateau phase toward the end of the experiment which can be interpreted as a steady state balanced between the cutting force of the suture and the mechanical stability of the sutured tissue.
For two reasons animals examined remained under anaesthesia throughout the entire duration of the experiment: In the first place, changes and superimposition of suture tension caused by spontaneous muscle activity, change of posture and/or changes of intra-abdominal pressure due to abdominal distension and oedema formation as seen after abdominal surgery or trauma were ruled out. It can be assumed that the loss of suture tension in an experimental setting allowing physiological changes of abdominal wall tension and intra-abdominal pressure would have produced different results. Secondly, the number of artefacts caused by spontaneous motion which might have complicated the interpretation of results was reduced.
The results of this study can not be uncritically transferred into conditions in humans. The small amount of fatty tissue in the abdominal wall of the pigs used in the experiment allowed a true fascial closure of the laparotomies. In humans, the amount of subcutaneous and pre-peritoneal fatty tissue often reaches a thickness of several centimetres. The inclusion of fatty tissue during fascial closure is thus often inevitable. This tissue contains only negligible amounts of collagen and the thread cuts through which might cause another relevant loss of suture tension.
The authors are aware of the fact that monofilament, slowly absorbable sutures are currently considered to be the material of choice for fascial closure. In the setting of our experiment, monofilament sutures were also tested. The more rigid monofilaments were found to affect measurement accuracy of the sensors, most probably because they do not adapt to the sensors as closely as the softer multifilament sutures finally used. An effect of the suture material on the results can not be ruled out but seems unlikely in a 24 h experiment.
Regarding suture tension dynamics, we have for the first time registered its course after laparotomy closure in an animal experiment. Mean tension necessary for fascial closure was approximately 1 N. After 23 h, the mean residual suture tension measured was approximately 0.5 N, meaning a weight of only 50 grams on the thread. An extensive literature search involving the years between 1974 and 2014 was performed to find comparable investigations. No comparable animal investigation has been published nor is any clinical investigation using a comparable setting available. Usually, surgeons try to control suture tension visually and tactile with the aim to closely approximate wound edges while at the same time avoiding the cutting of sutures through the tissue.
It seems however, that there is a range of applicable force between loose wound edges and excessive suture tension. How much control doe surgeons have regarding tension application?
In another experiment, surgeons were asked to apply suture tension just ‘adequate’ for fascial closure using a ‘knot-trainer’. 17 surgeons with a mean surgical experience of 86.7 months applied a tension of 2.8 N ± 1.13 N (mean ± SD) to close a mock fascia [8], almost three times the tension found necessary in our experiment and with a rather high standard deviation of roughly 40 % of mean. During our literature search, one study comparing the applied suture tension was found. In this study, the variation of initial suture tension ranged between 0.7 and 5.9 N although the aim of the researches was to place all sutures with the same tension [11]. As a consequence, it may be speculated that applied suture tension during wound closure is variable and far beyond standardization and control.
Although the negative influence of inadequate suture tension in different tissues leading to severe complications with a relevant socio-economic impact is well known, surgeons still rely on their tactile skill and their experience when suturing, mostly directed by an often cited ‘feeling for the tissue’ for which no scientific evidence exists [12]. Interestingly, scientific research has been focused on the influence of suture technique and suture material and their effects on incisional hernia incidence for years and two randomized multi-centre studies are still investigating these factors [13, 14]. The surgeons’ influence and the control of suture tension are still neglected.
The general decrease of suture tension registered in each animal and the similarity of curve progression between the animals clearly demonstrate that suture tension is no static parameter. The demonstrated self-adjustment of suture tension expose as a misconception the ability of surgeons to simply feel what ‘adequate’ suture tension is. The values of sensor Bf001-2 (Fig. 3) are the best example: The suture with the highest initial suture tension shows the steepest decrease of tension of all sutures.
Suture tension decreases because a primarily inadequate suture tension strangulates the sutured tissues and necrotic tissues are no more able to retain the suture. 50 % of initial suture tension may be an unnecessary surplus not contribution to suture stability but to the risk of suture failure. Complete absence of haptic control in laparoscopic suturing is another problem which has already been addressed [15]. Further experiments to evaluate a tissue specific suture tension optimum and testing of elastic suture materials will have to follow.
References
Albertsmeier M, Seiler CM, Fischer L, Baumann P, Hüsing J, Seidlmayer C, Franck A, Jauch KW, Knaebel HP, Büchler MW (2012) Evaluation of the safety and efficacy of MonoMax® suture material for abdominal wall closure after primary midline laparotomy- a controlled prospective multicentre trial: ISSAAC [NCT 005725079]. Langenbecks Arch Surg 397(3):363–371
Höer J, Lawong G, Klinge U, Schumpelick V (2002) Einflußfaktoren der Narbenhernienentstehung: Retrospektive Untersuchung an 2983 laparotomierten Patienten über einen Zeitraum von 10 Jahren. Chirurg 73:478–480
Cengiz Y, Blomquist P, Israelsson LA (2001) Small tissue bites and wound strength: an experimental study. Arch Surg 136:272–275
Israelsson LA, Jonsson T (1993) Suture length to wound length ratio and healing of midline laparotomy incisions. Br J Surg 80:1284–1286
Högström H, Haglund U, Zederfeldt B (1990) Tension leads to increased neutrophil accumulation and decreased laparotomy strength. Surgery 107:215–219
Höer J, Töns Ch, Schachtrupp A, Anurov M, Titkova S, Oettinger A, Schumpelick S (2002) Quantitative evaluation of abdominal wall perfusion after different types of laparotomy closure using laser fluorescence videography. Hernia 6:11–16
Höer J, Junge K, Schachtrupp A, Klinge U, Schumpelick V (2002) Influence of laparotomy closure technique on collagen synthesis in the incisional region. Hernia 6(3):93–98
Höer J, Wetter O, Klinge U, Junge K, Schumpelick V (2002) Can surgeons control suture tension? Results of a study with a newly designed device. Hernia 6(Supplement 1):27–28
Höer J, Wetter O, Peschke C, Schumpelick V, Weck M (2001) Einsatz miniaturisierter Sensoren zur Kontrolle von Naht- und Fadenspannung in der Chirurgie. In: Neue Technologien für die Medizin. Forschung, Praxis, Innovation. Shaker Verlag Aachen 2001, 321-340
Schachtrupp A, Graf J, Töns Ch, Höer J, Fackeldey V, Schumpelick V (2003) Intravascular volume depletion in a 24-hour porcine model of intra-abdominal hypertension. J Trauma 55:734–740
Klink CD, Binnebösel M, Aizai H, Lambertz A, von Trotha K, Junger E, Disselhorst-Klug C, Neumann U, Klinge U (2011) Tension of knotted surgical sutures shows tissue specific rapid loss in a rodent model. BMC Surg. doi:10.1186/1471-2482-11-36
Dunn AL, Buffa EA, Marchevsky AM, Heller J, Moores AP, Farell M (2012) Inter- and intra-operator variability associated with extracapsular suture tensioning: an ex vivo study. Vet Comp Orthop Traumatol 25(6):474–477
Rahbari NN, Knebel P, Kieser M, Bruckner T, Bartsch DK, Friess H, Mihaljevic AL, Stern J, Diener MK, Voss S, Rossion I, Büchler MW, Seiler CM (2012) Design and current status of CONTINT: continuous versus interrupted abdominal wall closure after emergency midline laparotomy - a randomized controlled multicenter trial [NCT00544583]. Trials. doi:10.1186/1745-6215-13-72
Harlaar JJ, Deerenberg EB, van Ramshorst GH, Lont HE, van der Borst EC, Schouten WR, Heisterkamp J, van Doorn HC, Cense HA, Berends F, Stockmann HB, Vrijland WW, Consten EC, Ottow RT, Go PM, Hermans JJ, Steyerberg EW, Lange JF (2011) A multicenter randomized controlled trial evaluating the effect of small stitches on the incidence of incisional hernia in midline incisions. BMC Surg. doi:10.1186/1471-2482-11-20
Martell J, Elmer T, Gopalsami N, Park YS (2011) Visual measurement of suture strain for robotic surgery. Comput Math Methods Med. doi:10.1155/2011/879086
Acknowledgments
Sensor and data logger development have been granted by the German Ministry of Education and Research Grantee: J. H. Grant No: 01EZ0013 AKM.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J H. declares conflict of interest directly related to the submitted work. The scientific work was granted by the German Ministry of Research and Education during the conduct of the study. A. S. declares conflict of interest directly related to the submitted work. The scientific work was granted by the German Armed Forces Health and Trauma Service Research Department during the conduct of the study. He is Chief Medical Officer of a medical service company. The underlying work was designed, performed and analyzed prior to his employment for this company. O. W. declares no conflict of interest.
Rights and permissions
About this article
Cite this article
Schachtrupp, A., Wetter, O. & Höer, J. An implantable sensor device measuring suture tension dynamics: results of developmental and experimental work. Hernia 20, 601–606 (2016). https://doi.org/10.1007/s10029-015-1433-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-015-1433-y