Abstract
Purpose
With a newly described diagnostic pathway, we aim to avoid unnecessary surgical exploration for suspected symptomatic groin hernias in pregnancy.
Methods
A consecutive series of eighteen pregnant women was referred to our department due to a gradual onset of inguinal swelling and groin ache. In a prospective clinical study, we evaluated these patients clinically and employed grey-scale and colour Doppler sonography (CDS) in all cases—following a newly described pathway. All patients were examined pre- and post-partum by two qualified surgeons. Median follow-up time was 11 months.
Results
4/18 of the suspected hernias first occurred towards the end of the first, the majority (12/18) in the second, 2/18 in the last trimester and all were suspected after clinical examination only. Most women were referred by their gynaecologists. We found no hernias in any of the women but always noted large varicose veins along the round ligament during CDS. All women gave uncomplicated birth to single children, one by caesarean section. Complaints subsided spontaneously within roughly 2 weeks after delivery. No patient developed a groin hernia until the end of the follow-up period.
Conclusion
The diagnosis of an inguinal hernia with a first symptomatic onset during pregnancy may be wrong in most cases. Anamnesis and clinical examination must be backed by CDS and round ligament varicosity as an important differential diagnosis must always be considered. Our structured diagnostic pathway helps to easily make the correct diagnosis. Surgical exploration of the groin during pregnancy must be avoided.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A gradual onset of inguinal tenderness and reducible swelling of the groin—typically even the labia majora in women with a first-ever manifestation—during pregnancy can occasionally be observed [1, 2].
Patients thereafter usually present to surgical specialists with a focus on hernia treatment after referrals by their attending gynaecologists, obstetricians, midwives and family doctors who are often much concerned about potential incarceration, additional discomfort or other adverse events caused by the suspected groin hernia during labour.
Published literature, however, offers hardly any well-defined recommendations for these patients or for the treatment of their frequently suspected inguinal hernias with a first onset during pregnancy.
The authors of the only published [3] prospective analysis have, in fact, come to the conclusion that women with an onset of inguinal hernia symptoms and their attending doctors should follow a watchful-waiting strategy during pregnancy and that patients ought to undergo post-partum surgical exploration for hernia repair of the groin.
Opposed to the apparent lack of diagnostic and therapeutic recommendations, there are numerous case reports of surgical explorations of the inguinal region for suspected hernia of the groin during pregnancy [4, 5].
They commonly describe a somewhat frustrating procedure during which usually no hernia sac can be found, no actual hernia can be diagnosed and which eventually puts both the patient and the unborn child at unnecessary and avoidable risk of adverse events before, during and after surgery.
The diagnosis of varicosities in the inguinal canal during pregnancy, causing soft and painful swelling in the groin, was described in several case reports as early as 1962 [6, 7].
The use of ultrasound and CDS examinations has been known to be useful for distinguishing true hernias from important differential diagnoses, namely RLV [8–10].
It is, in addition, worth noting that there is not a single reported case of incarceration during pregnancy or delivery caused by a groin hernia with a first symptomatic manifestation during pregnancy to the best of our knowledge.
We found the complete lack of published guidelines for the direction of these patients unhelpful and have therefore developed a standardised diagnostic pathway including grey-scale ultrasound and CDS examinations for the management of their condition in our department.
Whether or not the manifestation of RLV during pregnancy is a precursor to—or even an independent risk factor for—the occurrence of a groin- or femoral hernia following childbirth was initially completely unclear.
Methods
From 12/2008 to 10/2012, a consecutive series of eighteen pregnant women with a median age of 28.5 (20–40) years was referred to our department by their attending gynaecologists, family doctors and surgeons or presented to our outpatient clinic after self-referral and was seen for follow-up.
Their median body mass index (BMI) was evaluated at 24.9 (20.3–27.5).
Risk factors for the development of hernias like chronic obstructive pulmonary disease (COPD), smoking, glucocorticoid-intake, diabetes or malignant conditions were absent in all patients’ medical histories.
The presenting complaints were inguinal swelling, groin ache and pain with a gradual onset during pregnancy.
In the controlled prospective clinical study, the number of previous pregnancies and deliveries, the pregnancy’s trimester of the complaint’s onset, number of children born at the end of the pregnancy, possible pre-existing pathologic conditions of the groin, side of the complaint, diagnostic pathway and recommended management, complaint-related complications during labour, potentially recommended caesarean section for fear of complicated delivery, ongoing complaints after childbirth, possible surgical exploration of the inguinal region and manifestation of hernias in the previously swollen or tender groin at a later point in time were investigated.
In the last follow-up examination, particular attention was paid to the potential presence of a by then detectable inguinal hernia to see whether or not RLV in pregnancy resembles an indicator or even an independent risk factor for the development of groin hernias in the further course.
All patients were seen by two qualified surgeons with a focus on hernia surgery of our department prior to thorough clinical and careful grey-scale and colour Doppler sonographic examinations upon initial presentation as well as within 3 months after childbirth and during follow-up.
Results
Eighteen patients came to our department during pregnancy.
5/18 of them did so during their first, 6/18 in the second and 4/18 in their third pregnancy. Three women had a history of more than 3 previous pregnancies (4 or 5).
Most (13/18) pregnant women were referred by their gynaecologists and 2/18 by their family doctors. In addition, one of the women had also been seen by a surgeon of another hospital prior to presentation at our department, in this case hernia surgery before delivery was recommended. Two patients presented to our clinic after self-referral.
4/18 of the suspected hernias first occurred towards the end of the first, 12/18 in the second, 2/18 in the third trimester and all were initially suspected after clinical examination only.
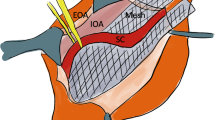
We could not verify an inguinal or femoral hernia in any of the women but always noticed the presence of reducible swelling of the respective inguinal region or at times even of the labium majus (Figs. 1 and 2) as well as varicose veins along the round ligament during Doppler sonography (DS) (Fig. 3).
During Valsalva’s manoeuvre, the swelling typically increased gradually. In accordance with the published literature [10], sonography revealed a reduced intravenous flowrate and an increase in the veins’ diameter under these conditions (Fig. 4).
Due to the type of ultrasound transducer (12 MHz, linear) available, we were not able to precisely determine the actual length of the dilated veins within the inguinal canal. Exemplarily, we have, however, in one patient measured the diameter of round ligament and varicose veins at rest and in supine position with 0.9 cm and during Valsalva’s manoeuvre in the same position with 2.1 cm.
A structure of these dimensions can without doubt be easily palpated in the groin upon clinical examination. Because of its size and noticeably increasing diameter during Valsalva’s manoeuvre, it can also easily be mistaken for a hernia, if not examined with sonography and CDS.
Thrombosis or rupture of these veins was not noted in any case in the course of the trial.
Signs and symptoms were located on the right side in 9/18 patients and on the left side in 6/18 patients; in 3/18 patients, a bilateral involvement was diagnosed.
All women gave birth to a single child without difficulty during labour.
One caesarean section was performed for the obstetrician’s fear of ‘hernia’-related complications during labour despite the fact that no hernia had been detected in our examinations in this case.
None of the pregnant women had previously undergone surgery for inguinal or femoral hernias. All complaints—like swelling in the groin and local inguinal tenderness—reportedly subsided spontaneously within approximately 2 weeks after childbirth. None of the women had to undergo surgery for inguinal or femoral hernias during the follow-up period of a median 11 (3–45) months.
3/18 patients were lost to follow-up due to a change in family name and/or contact details which made it impossible for us to re-invite them for a follow-up examination.
Post-partum as well as final examinations again consisted of a personal interview, clinical examination, grey-scale and colour-DS of the inguinal and femoral region.
Discussion
In 2007, Buch et al. [3] monitored the pregnancies of 12 women with—mixed groin and umbilical—hernias in a prospective study for the first time and operated on all of their patients after childbirth. As published, RLV was not considered as a differential diagnosis nor was sonography/CDS used in any of the cases.
The experience gained from this heterogenous study population led to the authors’ conclusion that even in the presence of an inguinal hernia a watchful-waiting strategy is a feasible approach towards the management of groin hernias in pregnancy.
This conclusion is supported by the fact that we know of no published medical reports about incarceration of groin hernias during pregnancy or delivery.
Despite these facts, the obstetrician’s concerns have to be taken seriously. Immediate feedback and clarification of the examinations’ results should be given to the referring doctors. To underline the importance of interdisciplinary communication, we report a caesarean section performed in one of our patients for the obstetrician’s fear of ‘hernia’-related complications during labour.
We agree with the published literature that a first-ever onset of inguinal swelling and tenderness during pregnancy resembles a diagnostic and therapeutic challenge.
From our study population, we do, however, see that the complaints reported are usually not caused by hernias and that differential diagnosis must be taken into consideration at an early stage in order to avoid unnecessary surgical risks for both the pregnant women and their unborn children.
We therefore propose an algorithm for the diagnostic work-up and further treatment (Fig. 5).
By strictly adhering to this standardised diagnostic pathway, in which grey-scale sonography and CDS are of pivotal importance, we diagnosed no inguinal or femoral hernias, lymphadenopathy or other pathologic conditions responsible for the symptoms.
Instead, RLV was disclosed to be the sole underlying cause of the presenting complaints in all our patients.
Accordingly, all symptoms subsided spontaneously within weeks after delivery and none of our patients developed hernias during the follow-up-period.
In addition, our findings rather strongly suggest that symptomatic RLV particularly in pregnancy is a much more frequent cause of inguinal-hernia-like symptoms than suggested by literature [11].
Furthermore, our observations reveal that RLV manifestations during gestation are neither an independent risk factor nor sentinel markers for the development of groin hernias in the post-partum period or thereafter. This, however, will have to be verified by longer periods of follow-up. The potentially increasing risk of development of inguinal or femoral hernias in patients in particular after multiple pregnancies with the symptoms described will therein be of special interest.
Subsuming published literature and supported by our own results, we are convinced that surgical exploration of the inguinal region for suspected inguinal hernias with a gradual onset of complaints during pregnancy is not indicated and that both grey-scale and CDS must always be used in the work-up of these cases.
Should patients history, thorough clinical and ultrasound examination, disclose the presence of a—then likely pre-existing—inguinal hernia during pregnancy in future patients, we agree with the published literature [3] that it must be monitored closely during the pregnancy and should be considered for surgery after childbirth.
It is for this reason that we specifically outline this option in our suggested algorithm’s hernia arm (Fig. 5).
References
Andriessen M, Hartemink K, de Jong D (2009) Round ligament varicosities mimicking inguinal hernia during pregnancy. Ned Tijdschr Geneeskd 153:A169
Ijpma F, Boddeus K, De Haan H, van Geldere D (2008) Management of hernias in pregnancy. J Am Coll Surg 208:320
Buch K, Tabrizian P, Divino C (2008) Management of hernias in pregnancy. J Am Coll Surg 207:539–542
Guillem P, Bounoua F, Duval G (2001) Round ligament varicosities mimicking inguinal hernia: a diagnostic challenge during pregnancy. Acta Chir Belg 101(6):301–311
Ijpma F, Boddeus K, de Haan H, van Geldere D (2009) Bilateral round ligament varicosities mimicking inguinal hernia during pregnancy. Hernia 13:85–88
Reisfield DR (1962) Varicosities in veins of the inguinal canal during pregnancy. J Med Soc NJ 59:24–26
McLaren CA, Brown PW (1983) Varicocoele in the female. J R Coll Surg Edinb 28:125
McKenna D, Carter J, Poder L, Gosnell J, Maa J, Pearl J, Goldstein R (2008) Round ligament varices: sonographic appearance in pregnancy. Ultrasound Obstet Gynecol 31:355–357
Murphy G, Heffernan E, Gibney R (2007) Groin mass in pregnancy. Br J Radiol 80:588–589
Uzun M, Akkan K, Coskun B (2010) Round ligament varicosities mimicking inguinal hernias in pregnancy: importance of color Doppler sonography. Diagn Interv Radiol 16:150–152
Buch K, Tabrizian P, Divino C (2008) Reply to: management of hernias in pregnancy. J Am Coll Surg 208:320–321
Conflict of interest
All authors declare no conflicts of interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lechner, M., Fortelny, R., Öfner, D. et al. Suspected inguinal hernias in pregnancy—handle with care!. Hernia 18, 375–379 (2014). https://doi.org/10.1007/s10029-013-1082-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-013-1082-y