Abstract
Purpose
The aim of this study was to evaluate the outcome of ilioinguinal and iliohypogastric nerve blocks in patients with chronic pain after herniorrhaphy, by comparing nerve stimulator and ultrasound guidance to administer the block.
Methods
A total of 43 patients who received nerve blocks for chronic inguinal post-herniorrhaphy pain received standardized questionnaires. Nerve stimulator–guided blocks were performed prior to January 2009, and thereafter, ultrasound-guided blocks were performed using a local anaesthetic solution and a corticosteroid.
Results
The questionnaire was completed by 38 patients (88 %). The inguinal hernia repair was performed for a median 16 months (range 3–219) ahead of the nerve blocks. A median of 2 pain treatments (range 1–7) was calculated. Median follow-up was 21 months (range 3–68). According to the DN4, 21 patients (55.3 %) no longer reported neuropathic pain. Subjectively, 32 % no longer reported moderate-to-severe pain. After ultrasound-guided blocks, a higher VAS score (at rest and during activities), a higher proportion of daily pain and more anxiety and depression are reported compared to blocks performed after nerve stimulator guidance.
Conclusions
Ilioinguinal/iliohypogastric nerve blocks can be effective to treat chronic inguinal pain following surgery of the groin. The use of ultrasound was not superior to nerve stimulator–guided blocks. These blocks could be considered prior to more invasive procedures such as neurectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inguinal hernia repair is one of the most commonly performed surgical procedures worldwide. Chronic post-surgical pain (CPSP) after inguinal hernia repair occurs frequently with a mean incidence of 11 % (range 0–43 %), resulting in the main problem after inguinal hernia repair [1]. This pain can be invalidating with a neuropathic character. Treatment modalities of this neuropathic pain include pharmacotherapy, peripheral nerve blocks, pulsed radiofrequency treatment, transcutaneous electrical nerve stimulation (TENS), peripheral nerve field stimulation, mesh/staple removal, neurectomy and cryoanalgesic ablation [2].
An ilioinguinal or iliohypogastric nerve block is a rather simple and useful regional anaesthetic technique for postoperative analgesia after inguinal surgery [3–6]. Despite its seemingly easy implementation, a relatively high failure rate of 10–25 % has been reported [7]. To decrease this failure rate, a technique using ultrasound to visualize the nerve, before injecting local anaesthetics, is described [6–8]. This technique might also cause fewer side effects, but this has not been definitively proven [9, 10]. A significant increase in the overall success rate for adequate blocks performed using an ultrasound-guided technique versus all non-ultrasound techniques has been shown [10]. It can be concluded that nerve blocks are more directly and more precisely administered using ultrasound guidance.
Although mostly investigated as anaesthesia during surgery, the application of the nerve block has also been used to reduce CPSP. In this application, the use of ultrasound could also be successful [6]. The aim of this study is to evaluate the long-term success of nerve blocks focussing on nerve stimulator– versus ultrasound-guided placement of the block.
Methods
Patients and data acquisition
All patients who underwent ilioinguinal and/or iliohypogastric nerve blocks for CPSP after herniorrhaphy in the Catharina Hospital Eindhoven, in the period of January 2003 until October 2010, were identified using the electronic hospital information system. The patient files were retrieved and reviewed for demographic data, operative details and complications of the nerve blocks. Performed surgical techniques were Lichtenstein repair or the Totally Extra Preperitoneal technique. All patients received a postal questionnaire including the DN4 questionnaire to estimate the probability of persistent neuropathic pain, Visual Analogue Scale (VAS) to score the intensity and frequency of pain, the Hospital Anxiety and Depression Scale (HADS) and Pain Disability Index (PDI). The DN4 was considered positive for neuropathic pain when scoring 4 or more points. The HADS was scored positive for anxiety or depression when 8 or more points were scored per category. Subsequently, the questionnaire also included the use of pain medication and antidepressants. Successful outcome was regarded as a neuropathic pain score below 4 on the DN4 scale.
Technique
The nerve blocks were performed by an anaesthesiologist of the department of pain management. In patients treated prior to January 2009, the nerve block was administered using nerve stimulator guidance. This technique was primarily based on anatomical landmarks. The patient was positioned in the supine position and the injection site was located 1 inch medial and 1 inch inferior to the anterior superior iliac spine [11]. The nerve stimulator was used to locate the nerves and was adjusted in a way that sensory nerve stimulation was within chronaxy.
Using the landmarks, the needle was positioned close to the nerves by applying an electrical current as guidance. If the patient experienced paraesthesias in the area supplied by the nerve at a threshold of 0.3 mA or less, the position of the needle is near the nerve. When the correct position was determined, a solution consisting 4 ml of 0.5 % bupivacaine and 80 mg of triamcinolonacetonide was injected.
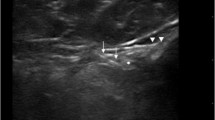
Since 2009, the nerve block injection was performed using ultrasound guidance for which a 38-mm broadband linear array transducer was used to explore the regional anatomy. According the technique described by Gofeld et al. [6], the anterior superior iliac spine (ASIS), ilioinguinal ligament and the line connecting the ASIS with the umbilicus were marked. The ilioinguinal nerve was visualized, mostly between the internal oblique and transverse or external oblique muscles and within 1–3 cm from the ASIS. A needle was inserted laterally through the entry point of the transducer, and 4 ml of 0.5 % bupivacaine and 80 mg of triamcinolonacetonide were deposited. The solution encircled the nerve and appeared as a distinct hypoechoic structure, highlighted by the hyperechoic surrounding fat [6]. Blocks were repeated after several months depending on the effect of the previous one. Upon patients’ request, other treatment modalities were performed.
Statistical analysis
Ordinal data were tested using Chi-square analysis and continuous data by Mann–Whitney U test. Differences were considered statistically significant when the p value was less than 0.05. All statistical evaluations were performed using SPSS, version 17.0 (SPSS, Chicago, IL, USA).
Results
All patients responded positive to the DN4 to rate their pain as neuropathic and had experienced a temporary effect of a diagnostic block, before treatment with nerve blocks. From the charts, no complications of the nerve blocks were encountered.
Forty-three (43) questionnaires were sent to patients who had undergone ilioinguinal or iliohypogastric nerve blocks in our hospital. In total, 38 patients (88.4 %) completed and returned the questionnaire. Of the 5 non-responders, 4 were untraceable and 1 refused to answer the questions. In total, 35 men (92.1 %) and 3 women (7.9 %) returned the questionnaire. The median age was 56 years (range 24-83). There were 39.5 % of the patients who experienced the CPSP on the left side, 52.6 % on the right side and 7.9 % of the patients experienced the pain on both sides. From this cohort, subjectively 30.6 % performed heavy work, 22.2 % performed light work and 47.2 % were retired or unemployed. The median number of injections was 2 with a minimum of one injection and a maximum of 7 injections. To cure the CPSP, 28.9 % of the patients received more than three injections. In total, 55.3 % of the blocks were performed using ultrasound guidance. The median follow-up was 21 months with a range of 3 to 68 months.
Table 1 shows the outcome of the ilioinguinal/iliohypogastric nerve blocks. Forty-five per cent of the patients still reported neuropathic pain (DN4 ≥ 4). More than two-thirds of the patients (68 %) graded their pain as moderate to severe. The pain was continuously present in 30 % of the cases. The median VAS score was 5 at rest and 7 during activities. Limitations during activities were rated with the Pain Disability Index with a median score of 29 and a widespread range of 0–70. Twenty-six percentage of the patients still used painkillers after treatment with these nerve blocks. Additional treatment such as TENS, neurectomy or acupuncture was performed in 21.1 % of the patients.
When comparing the groups who received the infiltration blocks, either nerve stimulator–guided or ultrasound-guided, the results were conflicting (Table 2). Only the VAS score during activities (p = .01) and VAS score during activities (p = .03) were significantly different between both groups. Also, the reported incidence of depression (p = .02) and anxiety (p = .01) was lower in the nerve stimulator group.
Discussion
Chronic pain after inguinal hernia repair is a severe disabling complication of this frequently performed operation [1]. Ilioinguinal/iliohypogastric nerve blocks can be effective to treat this complication, although repeated treatments may be required [6]. In this study, 55 % of the patients no longer reported neuropathic pain after treatment with ilioinguinal/iliohypogastric nerve blocks. However, only 32 % reported not to suffer moderate-to-severe pain any longer. Overall, high pain scores at rest or during activities and limitations for daily activities were reported.
Gofeld et al. [6] describe a group of patients in whom a block with local anaesthetic was successful, but only 5 out of 8 patients (62.5 %) reached complete pain relief for several days. In a study by Suresh et al. [12], two patients who underwent ultrasound-guided ilioinguinal nerve blocks with 5 ml of 0.25 % bupivacaine were described. These patients were still pain free at 6 months of follow-up. Furthermore, the use of CT guidance is proposed as a technique to visualize the nerve for the management of chronic pelvic pain [13, 14]. Parris et al. [13] described a case in which CT-guided ilioinguinal nerve block with 3 ml of 0.5 % bupivacaine was successful for 3 days.
In the present study, conflicting results were encountered. The higher pain scores in the ultrasound-guided group can be explained by the different follow-up duration, with a mean of 38 months in the nerve stimulator group and a mean of 13 months in the ultrasound guidance group (p < .01). Over time and after repeated blocks, more effect can be expected in the latter group. The more reported incidence of depression and anxiety is presumably more the result rather than the cause of more chronic pain in the ultrasound group.
In contrast to the herniorrhaphy group, in the group of patients who underwent different interventions none of them remained to have neuropathic pain. In a study examining chronic pain after pfannenstiel incisions, 7 % of the patients reported moderate-to-severe pain [15]. In half of these patients, nerve entrapment was seen.
The present study was a retrospective case series only, which can be seen as a limitation. No comparison to blocks without guidance or other treatments such as neurectomy was performed. The impact of guidance, nerve stimulator or ultrasound, or presumably increasing experience from the anaesthesiologists (>100 procedures) cannot be addressed to. Lastly, the difficulties of pain measurement were highlighted again in this study. Persisting high other pain scores hamper to regard disappeared neuropathic pain as a success. Nevertheless, in the group without neuropathic pain, significantly less disability due to pain was reported. Furthermore, HADS anxiety and depression level were significantly higher in the group with neuropathic pain. An interaction between chronic pain and depression is suggested in the literature [16].
To the authors’ belief, the nerve blocks could diminish the incidence of patients requiring a neurectomy as this is an invasive procedure of which no definitive success has been reported [17–20]. It remains unknown whether or not the success of a neurectomy is lower if persisting pain due to failed blocks endured longer. Haematoma, leg weakness, bowel haematoma, bowel puncture, femoral nerve block and high serum local anaesthetic concentration are described as complications of inguinal nerve blocks [21, 22]. In the present series, no such complications were encountered. Although our success was probably lower than the 62.5 % pain relief in the study of Gofeld et al. [6], we did find prolonged pain relief after a median follow-up of 20 months. Future studies should randomize nerve blocks and other treatment modalities, as will be presented by Loos et al. [23].
In conclusion, ilioinguinal or iliohypogastric nerve blocks can be effective to treat chronic inguinal pain. Success rate ranged from 32 to 55 %, although repeated treatments may be required. Ultrasound guidance was not superior to nerve stimulator guidance. Both techniques can be considered as an adequate therapy prior to more invasive procedures such as neurectomy.
References
Nienhuijs S, Staal E, Strobbe L, Rosman C, Groenewoud H, Bleichrodt R (2007) Chronic pain after mesh repair of inguinal hernia: a systematic review. Am J Surg 194:394–400
Thomassen I, van Suijlekom HA, van der Gaag A, Nienhuijs SW (2011) Intervention techniques for chronic postherniorrhaphy pain. Eur J Surg. doi:10.1007/s10353-011-0035-x
Shandling B, Steward DJ (1980) Regional analgesia for postoperative pain in pediatric outpatient surgery. J Pediatr Surg 15:477–480
Bunting P, McConachie I (1988) Ilioinguinal nerve blockade for analgesia after caesarean section. Br J Anaesth 61:773–775
McLoughlin J, Kelley CJ (1989) Study of the effectiveness of bupivacaine infiltration of the ilioinguinal nerve at the time of hernia repair for post-operative pain relief. Br J Clin Pract 43:281–283
Gofeld M, Christakis M (2006) Sonographically guided ilioinguinal nerve block. J Ultrasound Med 25:1571–1575
van Schoor AN, Boon JM, Bosenberg AT, Abrahams PH, Meiring JH (2005) Anatomical considerations of the pediatric ilioinguinal/iliohypogastric nerve block. Paediatr Anaesth 15:371–377
Willschke H, Marhofer P, Bosenberg A et al (2005) Ultrasonography for ilioinguinal/iliohypogastric nerve blocks in children. Br J Anaesth 95:226–230
Neal JM (2010) Ultrasound-guided regional anesthesia and patient safety: an evidence-based analysis. Reg Anesth Pain Med 35:S59–S67
Gelfand HJ, Ouanes JP, Lesley MR et al (2011) Analgesic efficacy of ultrasound-guided regional anaesthesia: a meta-analysis. J Clin Anesth 23:90–96
Cousins MJ, Bridenbaugh PO (2009) Neural blockade in clinical anaesthesia and pain medicine chap. 14, 4th edn. Lippincott Williams & Wilkins, Philadelphia, pp 343–371
Suresh S, Patel A, Porfyris S, Ryee MY (2008) Ultrasound-guided serial ilioinguinal nerve blocks for management of chronic groin pain secondary to ilioinguinal neuralgia in adolescents. Paediatr Anaesth 18:775–778
Parris D, Fischbein N, Mackey S, Carroll I (2010) A novel CT-guided transpsoas approach to diagnostic genitofemoral nerve block and ablation. Pain Med 11:785–789
Rigaud J, Riant T, Delavierre D, Sibert L, Labat JJ (2010) Somatic nerve block in the management of chronic pelvic and perineal pain. Prog Urol 20:1072–1083
Loos MJ, Scheltinga MR, Mulders LG, Roumen RM (2008) The pfannenstiel incision as a source of chronic pain. Obstet Gynecol 111:839–846
Soderfjell S, Molander B, Johansson H, Barnekow-Bergkvist M, Nilsson LG (2006) Musculoskeletal pain complaints and performance on cognitive tasks over the adult life span. Scand J Psychol 47:349–359
Loos MJ, Scheltinga MR, Roumen RM (2010) Tailored neurectomy for treatment of postherniorrhaphy inguinal neuralgia. Surgery 147:275–281
Amid PK (2004) Causes, prevention, and surgical treatment of postherniorrhaphy neuropathic inguinodynia: triple neurectomy with proximal end implantation. Hernia 8:343–349
Amid PK (2002) A 1-stage surgical treatment for postherniorrhaphy neuropathic pain: triple neurectomy and proximal end implantation without mobilization of the cord. Arch Surg 137:100–104
Amid PK, Hiatt JR (2007) New understanding of the causes and surgical treatment of postherniorrhaphy inguinodynia and orchalgia. J Am Coll Surg 205:381–385
Vaisman J (2001) Pelvic hematoma after an ilioinguinal nerve block for orchialgia. Anesth Analg 92:1048–1049
Lipp AK, Woodcock J, Hensman B, Wilkinson K (2004) Leg weakness is a complication of ilio-inguinal nerve block in children. Br J Anaesth 92:273–274
Loos MJA, Verhagen T, Scheltinga MRM, Roumen RMH (2010) A randomised controlled trial of injection therapy versus neurectomy for post-herniorrhaphy inguinal neuralgia: rationale and study design. Hernia 14:593–597
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thomassen, I., van Suijlekom, J.A., van de Gaag, A. et al. Ultrasound-guided ilioinguinal/iliohypogastric nerve blocks for chronic pain after inguinal hernia repair. Hernia 17, 329–332 (2013). https://doi.org/10.1007/s10029-012-0998-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-012-0998-y