Abstract
Objective
Incisional hernia at the site where a patient had previously had a stoma has not been clearly studied. The aim of this study is to determine the incidence and associated factors that may lead to an incisional hernia related to the reversal of an intestinal stoma.
Patients and methods
An analysis was made of 70 cases of intestinal reconnection. All patients received Cefotaxime or Ceftazidime during anaesthesia induction and two more doses at 1–8 h in the post-operative period. In all of the cases, closure of the stoma site was effected as a primary closure using no. 1 polyglycolic acid continuous suture. There followed wound lavage with iodopovidone, and the skin was closed with simple sutures using polypropylene 3/0. No drain was left in situ in any of the cases. The study considered the following aspects: demographic characteristics of the study group; illnesses giving rise to the need for stoma formation; the stoma site itself; clinical aspects, including body mass index (BMI); the incidence of incisional hernia; and any complications involving the surgical wound.
Results
At this hospital, the cause of requiring treatment with stoma formation was diverticular disease of the colon principally, and the age of the patients varied from 36 to 87 years (median 61). The incidence of incisional hernia at the stoma site was 22 cases (31.4%), presenting equally in both sexes and with greater frequency under the following circumstances: during the first year of follow-up and in patients with concomitant illnesses, principally diabetes. Local complications involving the surgical wound occurred in six cases (8.5%).
Conclusion
The incidence of incisional hernia at the stoma site was found to be 31.4% in this study, which is a high incidence of hernias with simple repair.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stoma formation following trauma or due to the presence of inflammatory or neoplastic diseases of the colon or small intestine is a common practice. The stoma so formed may be temporary or permanent.
On reconnecting the digestive tract, a wound inevitably remains on the abdominal wall at the site where the stoma was previously located, and the usual practice is to apply a primary repair technique in the closure of this wound.
The objective of the study being reported here was to establish the incidence of incisional hernia at the stoma site.
Patients and methods
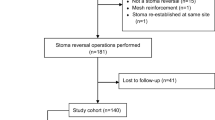
This retrospective study covered the period from May 1999 to January 2007, and reviewed the clinical files of 70 patients who had undergone stoma closure and intestinal reconnection, whether it was following an ileostomy or a colostomy. Pre-operative preparation for all patients involved a cathartic on the day prior to reconnection surgery, plus 1 g of third-generation cephalosporins (Cefotaxime or Ceftazidime) during the peri-operative period, which included one dose during anaesthesia induction and two more doses more 1–8 h in the post-operative period.
Closure of the stoma site was effected in all cases with a suture on a single plane using no. 1 polyglycolic acid (Vicryl®) continuous suture; surgical wound lavage was carried out using iodopovidone (Isodine®), and the skin was closed with polypropylene 3/0 simple or Sarnoff sutures. No wound drain was left in situ.
An analysis was carried out of the demographic aspects of the study group; the illness leading to stoma formation; the stoma site itself; the clinical aspects of the patient, including body mass index (BMI); the incidence of incisional hernia; and any complications involving the surgical wound.
The follow-up time experienced by the patients ranged from 2 months to 7 years and 3 months, with a median length of 28 months.
Statistical analysis was conducted using average and median central tendency measurements.
Results
A study was made of 70 patients who had had a temporary stoma, and included 53 male (59%) and 37 female patients (41%), with age mean of 61 years (range 36–87).
The illnesses giving rise to the need for stoma formation in the 70 patients who then underwent intestinal reconnection are listed in Table 1. In this regard, it should be noted that our hospital actually receives few trauma patients, because there is an emergency trauma hospital of our institution nearby. The presentation age of stoma patients varied from 36 to 87 (median age 61). Concomitant illnesses were present in 19 patients (27%), and the most frequent were found to be diabetes mellitus and arterial hypertension. Table 2 summarises the concomitant illness in patients with and without hernia. It is noteworthy that the incidence is equal in both sexes. The BMI mean was 36 kg/m2 (range 25–52) in both groups.
The stoma site was by colostomy in 65 patients (93%) and ileostomy in five (7%); the incidence of incisional hernia at the stoma site occurred in 22 cases (31.4%), all in the colostomy group. Local complications occurred in six patients (8.5%), particularly notable was the incidence of surgical wound infection in three cases (4.2%). These were treated with debridement and surgical wound lavage plus antibiotics (Cefotaxime and Metronidazole). In all three cases, Escherichia coli and Klebsiella sp. were isolated in the wound culture. The other complications included one seroma and two hematomas.
Table 3 summarises the characteristics of the population developing incisional hernia at the stoma site. The results show that the frequency of occurrence is greater under the following circumstances: during the first year of follow-up and in patients with concomitant illnesses, mainly diabetes.
The median delay between wound repair and incisional hernia was 6 months (range 2–25).
Discussion
The incidence of incisional hernia at the stoma site is not clearly established in the literature, because many series do not count the phenomenon as a post-operative complication, either because it does not appear soon after surgery or because it is simply not diagnosed. An analysis of 216 stoma cases presented at the 2005 Congress of the Association of Surgeons of Great Britain and Ireland (ASGBI) found the frequency of hernia at the stoma site to be 8.3% [1]. By contrast, the study reported here revealed an incidence of 31.4%, which is similar to the general incidence of incisional hernia [2–4].
Abdominal wall hernia or incisional hernia is a complication that presents in 13–35% of patients undergoing abdominal surgery, conditioned, in part, by well-established predisposing factors [5, 6], such as cancer, obesity, diabetes, cirrhosis of the liver, malnutrition, Crohn’s disease, collagenopathies, chronic renal insufficiency and chronic pneumopathies, conditions that do not permit good repair processes of the wound. Abdominal hernia at the stoma site should behave similar to other parts of the abdomen.
The group that principally developed an incisional hernia at the stoma site is that who suffer a concomitant illness, principally diabetes mellitus, even when it is well-controlled. This author considers, therefore, that a mesh prosthesis should be used at the stoma site during closure of the abdominal wall in cases of these types. Indeed, these factors have already been identified by Arumugam et al. [7] as factors indicating the risk of other complications in stoma formation, even though that particular study does not include hernias at the stoma site occurring after reconnection.
The general thinking to date has been that a prosthetic mesh should not be used in contaminated sites or when the surgery involves opening the digestive tract. However, studies exist confirming the safety of using a prosthetic mesh in surgery on a prepared intestine [8, 9]. It follows, therefore, that the management of a stoma in an intestine prepared prior to surgery, and with a low concentration of bacteria, does not contraindicate the use of a mesh.
In the opinion of this author, given that incisional hernia at the stoma site presents in a third of patients following reconnection of the digestive tract, closure using a mesh prosthesis should be considered. However, comparative studies need to be conducted to provide more data.
Conclusion
The incidence of incisional hernia at the stoma site is high. In this study, it was found to be 31.4%.
References
Dalmia S, Marimuthu K, Nagpal K, Matthew G (2005) Intestinal stomas: an analysis of 216 cases. Association of Surgeons of Great Britain and Ireland (ASGBI) abstract
Kingsnorth A (2006) The management of incisional hernia. Ann R Coll Surg Engl 88:252–260
Guzmán-Valdivia G, Medina O, Martínez A (2003) Simplified technique for incisional hernia repair with mesh prosthesis. Hernia 7:206–209
Cassar K, Munro A (2002) Surgical treatment of incisional hernia. Br J Surg 89:534–545
Geçim I, Koçak S, Ersoz S, Bumin C, Aribal D (1996) Recurrence after incisional hernia repair: results and risk factors. Surg Today 26:607–609
Ríos A, Rodríguez J, Munitiz V, Alcaraz P, Pérez D, Parrilla P (2001) Factors that affect recurrence after incisional herniorrhaphy with prosthetic material. Eur J Surg 167:855–859
Arumugam PJ, Bevan L, Macdonald L, Watkins AJ, Morgan AR, Beynon J, Carr ND (2003) A prospective audit of stomas—analysis of risk factors and complications and their management. Colorectal Dis 5:49–52
Birolini C, Utiyama M, Rodrigues AJ Jr, Birolini D (2000) Elective colonic operation and prosthetic repair of incisional hernia: does contamination contraindicate abdominal wall prosthesis use? J Am Coll Surg 191:366–372
Geisler DJ, Reilly JC, Vaugham SG, Glennon EJ, Kondylis PD (2003) Safety and outcome of use of nonabsorbable mesh for repair of fascial defects in the presence of open bowel. Dis Col Rectum 46:1118–1123
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Guzmán-Valdivia, G. Incisional hernia at the site of a stoma. Hernia 12, 471–474 (2008). https://doi.org/10.1007/s10029-008-0378-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-008-0378-9