Abstract
Background
There are many different meshes available for laparoscopic repair of ventral hernias. A relatively new product is the Proceed mesh with a bioresorbable layer against the bowels and a polypropylene layer against the abdominal wall. There are, however, no human data available. The aim of this study was to evaluate the feasibility and outcome after laparoscopic ventral hernia repair using the Proceed mesh in humans.
Methods
Patients presenting for laparoscopic ventral hernia repair in our department from September 2004 to October 2006 were included in the study. All patients had a standard laparoscopic ventral hernia repair using the Proceed mesh secured with tackers with a double crown technique. Patients were discharged according to standard discharge criteria, and follow-up was performed with a search in the national patient database and with manual search in the patients’ files.
Results
Our study included 49 patients with a median age of 64 years (range 30–89) and body mass index of 27.8 (19.4–50.5). The dimensions of the mesh varied from 4 × 4 cm to 30 × 40 cm (median 15 × 15 cm). One patient developed an uncomplicated wound infection and none of the 49 patients developed mesh infections or postoperative seroma requiring surgical intervention. Thus, there were no mesh-related complications. During the follow-up period of 17 months (3–27), we have not seen any postoperative recurrences. The median length of stay was 1 day (range 0–63), and there was no mortality.
Conclusion
Laparoscopic ventral hernia repair in humans using the Proceed mesh is feasible and has a low complication rate even in obese patients or those with pulmonary disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Incisional hernia remains a risk after abdominal surgery. There are reported hernia incidences of 3–11% in patients having laparotomies and a 23% incidence in patients who experience infection of their laparotomy wound [1–5]. A recent systematic review revealed an overall hernia risk of 7.4% after laparotomy [6]. Primary suture repair of ventral hernias has reported recurrence rates of 25–52% [7, 8]. The introduction of prosthetic meshes to repair abdominal wall defects without tension, thereby leading to secondary respiratory complications, has reduced this recurrence rate to 13–19% after open surgery [9, 10] and to as low as 4.5% after laparoscopic repair [11].
There are many meshes on the market and we have used the Proceed mesh (Ethicon, Somerville, NJ, USA) since its introduction in 2004. There are, however, no human data available in the literature on the use of the Proceed mesh. We therefore want to report our experience with this mesh regarding feasibility and outcome after laparoscopic ventral hernia repair.
Patients and methods
Consecutive patients presenting for ventral hernia repair in our department from September 2004 to October 2006, except for the smallest umbilical hernias with a diameter of the defect of about 1 cm, were all scheduled for laparoscopic repair using the Proceed mesh (see Table 1). The Proceed mesh was made available for use in August 2004 and we performed the first operations during September 2004. We have used the Proceed mesh continuously since then, except for the period of product recall when we were not able to get the mesh for 6–8 months during 2006. Patients operated with other meshes during this period are not included in the present paper.
The Proceed mesh is a thin, flexible laminated mesh designed for repair of fascial deficiencies [12]. It consists of a cellulose fabric (ORC) and a polypropylene layer. The polypropylene side of the product allows tissue ingrowth while the ORC component provides a bioresorbable layer that separates the mesh from underlying organs, and thereby minimizes the risk of permanent tissue attachment to net mesh.
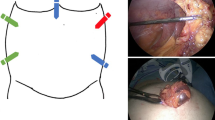
The laparoscopic ventral hernia repair was performed with a standard technique, removing all adhesions to the front abdominal wall and then securing a Proceed mesh, typically with a minimum of 5-cm overlap in all directions from the defect. The mesh was secured with tackers (Protack, Tyco Healthcare, Norwalk, CT, USA) using a standard double crown technique and we did not use sutures for mesh fixation. For the operations, three to five trocars were used depending on the size of the hernia. No antibiotics were given and we did not use drains in any of the patients. Postoperatively, patients were discharged from the hospital according to standard discharge criteria including being able to walk freely, eat and drink normal food, perform normal bowel movements and only requiring oral analgesics.
The data acquisition was performed in the electronic national hospital data register for reoperations supplemented with a manual check of hospital files. The follow-up period ended 31 December 2006.
Results
All operations were completed laparoscopically, and 49 patients were operated on during the inclusion period. The median follow-up time was 17 months. Many of the patients were moderately obese, with 16 patients having a BMI > 30, 15 (31%) were smokers, and 7 (14%) had been formally diagnosed with chronic obstructive pulmonary disease (COPD).
The results are summarized in Tables 1 and 2. Five (10%) of our patients required the insertion of two separate meshes in order to cover the hernia area, and one of these patients required two meshes each measuring 20 × 30 cm stitched together, forming a mesh of 40 × 30 cm, in order to cover his hernia defect. The vast majority of patients stayed for 0–2 days after their operation (median stay was 1 day), five patients went home on the day of their surgery, and only three patients stayed for longer than 10 days.
There was no mortality among the 49 patients who underwent surgery. Five patients developed postoperative complications: one patient developed a pulmonary embolus on the second postoperative day and was hospitalized for 37 days, one patient developed respiratory complications and was hospitalized for 54 days, one patient developed uncomplicated pneumonia and had a quick recovery, one patient had intraabdominal bleeding with a hemoglobin drop, which was conservatively treated, and was hospitalized for 2 days, and one patient had a small bowel perforation during a stomal hernia repair and underwent re-laparotomy with removal of the mesh. This patient had a complicated course with hospitalization for 63 days, which also required intensive care during that period, but she had full recovery. Among the other 44 patients there was no morbidity. Only one patient developed an uncomplicated wound infection (trocar site), and none of the 49 patients developed postoperative seroma requiring emptying by a needle or surgical intervention. Thus, there were no mesh infections in our total group of 49 patients. Furthermore, we did not see any signs of recurrence during the follow-up period.
Discussion
Our results have shown that laparoscopic repair of ventral hernia using the Proceed mesh is feasible with a very low complication rate. In particular, we had no mesh infections, and seroma formation was not a clinical problem.
The patients were included consecutively, and all operations could be completed laparoscopically. We have previously used other meshes for laparoscopic ventral hernia repair, but the Proceed mesh is excellent for intraabdominal repair of abdominal wall deficiencies. Some years ago we used the Goretex mesh (ePTFE), but although the mesh has a different structure on its two sides, it is quite thick and difficult to manipulate and to introduce into the abdominal cavity. Furthermore, we have done quite a few re-operations in these patients where the mesh has shrunk to very small sizes causing hernia recurrences. Finally, the price of this mesh is higher than the other materials available on the market, and we therefore abandoned this mesh some years ago. Thereafter, we used the Parietex composite mesh (polyester with bovine inactivated collagen). Our results with this mesh have been fine with still no infections and no recurrences yet. However, it is not possible to cut the mesh to the preferred size, and it may be a little difficult to manipulate in the abdominal cavity, and we therefore also abandoned this mesh a couple of years ago.
There are no randomized clinical trials available comparing different meshes for laparoscopic ventral hernia repair in humans. There are some animal data available [13–16], but this cannot be translated directly to the human situation because of, e.g., differences in daily life between animals and humans, working conditions, inter-individual differences in collagen properties, and age-related effects on wound healing. Thus, the literature cannot give general recommendations for choice of mesh based on randomized clinical trials, so surgeon’s preference and cost will most often determine the choice of mesh [11].
We based our follow-up on review of the patients’ medical records supplemented by a database search for admissions to other hospitals. During the follow-up period we did not experience any complications that needed admission. This probably means that the patients have not experienced any serious complications or recurrence, although we may have overlooked a recurrence if the patient did not contact a surgical hospital department. We had a median follow-up time of 17 months, and it is therefore possible that some patients may develop late recurrences after the operation. Further long-term follow-up studies should focus on this problem comparing the different composite meshes available on the market.
Incisional hernia is likely to develop after laparotomy [1–5] and with a higher incidence after vertical compared with horizontal incisions [17]. When inserting a mesh via open surgery the recurrence rates are in the range of 13–19% [9, 10]. However, this method has several drawbacks, some of them being soft-tissue dissection in already poor quality tissue and postoperative drain placement. This has led to a complication rate of up to 20% involving wound infection, mesh infection and fistula formation [18–20]. In laparoscopic repair, the surgeon can avoid extensive dissection of the vulnerable tissue with fewer complications, less pain and earlier recovery [21, 22]. New meshes for laparoscopic repair are frequently introduced, and often without any published human data. The present paper is the first report on use of the Proceed mesh in humans, and our experience so far has been very encouraging even though our patient sample was heterogeneous and had a median follow-up of 17 months.
Conclusion
During a 2-year period we inserted 54 Proceed meshes in 49 patients with ventral hernia in our department. All operations were done laparoscopically. There was no mortality, and morbidity rate was low. In particular, we only found one wound infection at a trocar site and no seromas requiring surgical intervention. Thus, there were no mesh infections or other mesh-related complications requiring reinterventions. Laparoscopic ventral hernia repair using the Proceed mesh therefore seems to be a promising technique for treating ventral hernias even in higher risk patients who are obese or have pulmonary diseases.
References
Gorge CD, Ellis H (1986) The results of incisional hernia repair: a twelve year review. Ann R Coll Surg Engl 68:185–187
Mudge M, Hughes LE (1985) Incisional hernia: a 10-year prospective study of incidence and attitudes. Br J Surg 72:70–71
Bucknall TE, Cox PJ, Ellis H (1982) Burst abdomen and incisional hernia: a prospective study of 1129 major laparotomies. BMJ 284:931–933
Carlson MA, Ludwig KA, Conlon RE (1995) Ventral hernia and other complication of 1.000 midline incisions. South Med J 88:450–453
Khaira HS, Lall P, Hunter B, Brown JH (2001) Repair of incisional hernias. J R Coll Surg Edingb 46:39–43
Cheng H, Rupprecht F, Jackson D, Berg T, Seelig MH (2007) Decision analysis model of incisional hernia after open abdominal surgery. Hernia 1265:129–137
Stoppa RE (1989) The treatment of complicated groin and incisional hernias. World J Surg 13:545–554
Hesselink VJ, Luijendijk RW, deWilt JHW, Heide R, Jeekel J (1993) An evaluation of risk factors in incisional hernia recurrence. Surg Gynecol Obstet 176:228–234
Koller R, Miholic J, Jalk RJ (1997) Repair of incisional hernias with expanded polytetrafluorothylene. Eur J Surg 163:261–266
Bauer JJ, Harris MT, Kreel I, Gelernt IM (1999) Twelve-year experience with expanded polytetrafluorothylene in the repair of abdominal wall defects. Mt Sinai J Med 66:20–25
Eriksen JR, Gögenur I, Rosenberg J (2007) Choice of mesh for laparoscopic ventral hernia repair. Hernia 11:481–492
Johnson and Johnson (2008) Proceed surgical mesh. http://www.proceedmesh.com. Accessed March 2008
Harrell AG, Novitsky YW, Christiano JA, Gersin KS, Norton HJ, Kercher KW, Heniford BT (2007) Prospective histologic evaluation of intra-abdominal prosthetics four months after implantation in a rabbit model. Surg Endosc 21:1170–1174
Jacob BP, Hogle NJ, Durak E, Kim T, Fowler DL (2007) Tissue ingrowth and bowel adhesion formation in an animal comparative study: polypropylene versus Proceed versus Perietex Composite. Surg Endosc 21:629–633
Novitsky YW, Harrell AG, Cristiano JA, Paton BL, Norton HJ, Peindl RD, Kercher KW, Heniford T (2007) Comparative evaluation of adhesion formation, strength of ingrowth, and textile properties of prosthetic meshes after long-term intra-abdominal implantation in a rabbit. J Surg Res 140:6–11
Novitsky YW, Cristiano JA, Harrell AG, Newcomb W, Norton JH, Kercher KW, Heniford BT (2008) Immunohistochemical analysis of host reaction to heavyweight-, reduced-weight-, and expanded polytetrafluoroethylene (ePTFE)-based meshes after short- and long-term intraabdominal implantations. Surg Endosc. doi:10.1007/s00464-007-9737-3
Grantcharov TP, Rosenberg J (2001) Vertical compared with transverse incisions in abdominal surgery. Eur J Surg 167:260–267
Leber GE, Garb JL, Albert AI, Reed WP (1998) Long-term complications associated with prosthetic repair of incisional hernias. Arch Surg 132:1141–1144
Park A, Gagner M, Pomp A (1996) Laparoscopic repair of large incisional hernias. Surg Laparosc Endosc 6:123–128
White TJ, Santos MC, Thompson JS (1998) Factors affecting wound complications in repair of ventral hernias. Am Surg 64:276–280
Costanza MJ, Heniford BT, Arca MJ, Mayes JT Gagner M (1998) Laparoscopic repair of recurrent ventral hernia. Am Surg 64:1121–1127
Ramshaw BJ, Esartia P, Schwab J, Mason EM, Wilson RA, Duncan TD, Miller J, Lucas GW, Promes J (1999) Comparison of laparoscopic and open ventral herniorrhaphy. Am Surg 65:827–831
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rosenberg, J., Burcharth, J. Feasibility and outcome after laparoscopic ventral hernia repair using Proceed mesh. Hernia 12, 453–456 (2008). https://doi.org/10.1007/s10029-008-0368-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-008-0368-y