Abstract
Background
Parastomal hernia with a reported incidence of up to 50% is a major problem after ostomy formation. Hernias at the closure site may be a problem after the closure of the enterostomy. In this study, in addition to physical examination, we used ultrasonography (USG) in order to find the true incidence of ostomy closure site and laparotomy incisional hernias.
Methods
We examined patients with closed enterostomy sites by both physical examination and USG for the detection of hernias. Risk factors for hernia formation, such as age, gender, body mass index (BMI), ostomy type, and surgical site infections, were determined.
Results
The evaluation of 31 patients with ostomies resulted in a 32% incidence of closed ostomy site hernias when patient medical history, physical examination, and ultrasonographic examination were used together. With physical examination and USG, incisional hernias at the laparotomy incision were found in 58% of cases. USG was able to detect hernias which were not clinically evident at the ostomy closure site and the laparotomy wound. BMI, age, gender, ostomy type, and surgical site infection did not have a significant effect on hernia formation.
Conclusion
Ostomy closure site and laparotomy incisional hernias are important clinical problems with a high incidence after ostomies are closed. Closure of the enterostomy site should be regarded as a hernia repair rather than a simple fascial closure. USG is a valuable clinical tool in combination with physical examination for the detection of minor defects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The surgical treatment of some gastrointestinal and other intraabdominal pathologies may cause the patient to end up with a colostomy or ileostomy. Parastomal hernia, with a reported incidence of 5–52%, is a commonly encountered problem [1–4]. While parastomal hernias constitute a major problem, hernias at repaired ostomy sites is another concern, with a high incidence of up to 26% using physical examination alone [4]. Although some studies investigated the early morbidity and mortality of ostomy closure, studies addressing the incidence of hernias at the ostomy closure site in the long-term are lacking [4–8].
Most commonly, hernias are diagnosed with physical examination, but it has been shown that clinically undetected hernias can be diagnosed with additional radiological studies [4]. Ultrasonography (USG) has been found to be useful in the detection of abdominal wall hernias which are not clinically overt [9].
In this study, patients with closed ostomies were evaluated in order to define the incidence of hernias at the repaired enterostomy site and the laparotomy wound. Hernias were diagnosed with physical examination and USG. Patient complaints regarding ostomy site hernias were also determined.
Materials and methods
All patients undergoing enterostomy closure of any type from January 2002 to August 2006 at the Marmara University Hospital General Surgery Unit, Istanbul, Turkey, were included in the study. All contacted patients were invited for interview, physical examination, and ultrasound evaluation. The operative details, risk factors for hernia formation, such as age, gender, body mass index (BMI), ostomy type, and surgical site infections, were determined. Patients were also inquired about their complaints regarding the enterostomy closure site.
In patients with loop ostomies, the intestinal continuity was maintained through the ostomy site without additional laparotomy. In cases with end ostomies, laparotomy was performed for intestinal anastomosis. Fascial defects at the enterostomy sites were closed with interrupted no. 0 or 1 polypropylene sutures. All patients were given prophylactic antibiotics. The wounds at the ostomy closure sites were left open and were closed after 3–4 days with 3.0 polypropylene or silk sutures. In patients requiring laparotomy, the fascial closure was performed with continuous no. 1 PDS suture and the skin was closed with a stapler.
Physical examinations to detect hernias were performed both in standing and supine positions for all patients and also during increased abdominal pressure by the Valsalva maneuver. Both repaired enterostomy sites and abdominal incision sites were examined. On physical examination, a hernia was defined as a bulging during the Valsalva maneuver and palpation of the fascial defect. USG was performed by a radiologist with a GE pro 500, 3 MHz and both repaired enterostomy sites and abdominal incision sites were investigated for the presence of hernias. A loop of intestine or any abdominal organ, as well as omentum, protruding through the defective abdominal wall with an acoustic shadow was considered as a hernia.
Statistical analysis was performed by the computer-based program, SPSS version 11.5 (Chicago, Illinois). Continuous variables such as age and BMI were evaluated by Students’ t-test and gender, surgical site infection, and ostomy type were evaluated by the χ2 and Fisher’s exact tests, where appropriate. p<0.05 was considered to be statistically significant. Odds ratios and 95% confidence intervals were also calculated.
Results
In the 4.5-year period from January 2002 to August 2006, enterostomies were closed in 66 patients. Colostomy closures were carried out in 48 and ileostomy closures in 18 patients. Fifteen of these patients had died at the time of the study. Of the remaining 51 patients, 31 patients (61%) accepted the invitation to be included. All cases were examined at the general surgery and radiology units by different physicians. Sixteen patients had a Hartmann’s procedure as the index operation (52%) and, for the remaining patients, loop colostomies in eight, loop ileostomies in four, and end ileostomies in three patients were performed. Neoplastic diseases (74%) and colonic diverticulitis (13%) were the underlying pathology in most of the patients. The median follow-up time was 26 months (range 3–118 months) for the entire group. The median time between the index operation and ostomy closure time was 5.7 months (range 1–14 months).
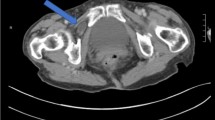
In patients with closed enterostomies, with physical examination, four (13%) were found to have hernias at the closure site. When USG was performed for the 31 patients, six patients (19%) were found to have hernias at the ostomy closure site. USG evaluation could not detect hernia in one patient with a hernia on physical examination. This patient was further evaluated with computed tomography and was confirmed to have fascial defect and hernia. USG was able to detect three clinically undiagnosed hernias. In the study group, three other patients were found to be operated for symptomatic enterostomy site hernias with polypropylene mesh and none had a recurrence. Taken altogether, 10 out of 31 patients (32%) had hernias at the closed enterostomy sites detected with physical examination and/or radiological investigation.
Six out of the ten patients with hernia have or had pain due to herniation at the enterostomy closure site. Age, surgical site infection, type of ostomy, gender, BMI, and ostomy closure time had no significant effect on hernia formation at the ostomy site. (Table 1).
Fourteen patients (45%) had an incisional hernia at the abdominal incision with physical examination alone. When USG was used, 16 patients (52%) were found to have incisional hernias. In two patients where incisional hernias were found with physical examination, USG could not detect a fascial defect. On the other hand, in four patients with normal physical examination findings, fascial defects were detected with USG. Overall, 18 patients (58%) were diagnosed as having incisional hernias on physical examination and/or USG. With ultrasonographic examination, no communicating defect between the midline and stoma closure hernias was observed.
Age, surgical site infection, type of ostomy, gender, BMI, and ostomy closure time did not significantly contribute to incisional hernia formation at the ostomy site. Patients with incisional hernias at the laparotomy wound were found to have an increased risk (OR: 4.4) of having hernias at the ostomy closure site (Table 2).
Discussion
Parastomal hernias have been investigated more commonly than ostomy closure site hernias because the latter is considered as a less significant problem. In this study, a 32% hernia rate at the ostomy closure site after a median follow-up of 26 months indicates that this problem has been underestimated. USG in this study was able to diagnose clinically undetectable cases. However, USG had a significantly high false negativity in diagnosing both closure site and abdominal incisional hernias. This study has stressed that, for the diagnosis of ostomy closure site and abdominal incisional hernias, physical examination and USG are complementary. In our previous study, hernias were found at the enterostomy closure site in 26% of patients with physical examination alone and, when CT was used, the incidence increased to 48% [4]. USG was preferred in this study as it is less expensive, more practical and without the use of ionizing radiation, and it has been proven to be clinically efficient.
Thomson and Hawley [10] reported a 2.9% incidence of hernias at the ostomy closure site; however, the authors also admit that they had followed only 46% of their patients for more than a year and this figure probably does not represent the true incidence. In another study by Porter et al. [11], six hernias were reported after the closure of 43 colostomies (14%). In our study, clinically evident ostomy site hernias were found in 23% (7/31) of patients with closed ostomies and three of these patients were operated for symptomatic hernias. All ostomy site hernias were repaired with on-lay polypropylene mesh. With the use of USG, the incidence increased to 32% (10/31). BMI, age, gender, ostomy type, and surgical site infection did not have a significant effect for ostomy closure site hernia formation, although the small sample size should be considered while interpreting these findings.
It is obvious that the incidence will increase with a longer follow-up period. Here, a 32% incidence of enterostomy closure site hernia is similar to the 36–49% recurrence rate of incisional hernias treated with suture repair [12, 13]. In this study, all enterostomy fascial closures were performed with interrupted polypropylene sutures and with this high hernia incidence, the necessity of a more secure way of closing enterostomies is obvious. Although the use of interrupted sutures instead of running polypropylene sutures might be a concern still, closure of the enterostomy site should be regarded as a hernia repair rather than a simple fascial closure.
While there are some recommendations for the treatment and prevention of parastomal hernias with prosthetic mesh [14–17], currently, there is no recommendation for ostomy closure site hernia prevention. The use of prophylactic mesh for the prevention of parastomal hernias has given promising results [16, 17] and this might also be a strategy for the prevention of ostomy closure site hernias. Although the use of nonabsorbable mesh for the repair of fascial defects in the presence of an open bowel is an important concern, Geisler et al. [18] state that, after bowel preparation, nonabsorbable mesh can be used with minimal risk of infection. Prophylactic sub-lay mesh at the time of closure for the prevention of ostomy site hernias may be an alternative and should be investigated. The transfer of experimental research to daily practice might offer some hope. The use of transforming growth factor beta (TGF-β) and fibroblast growth factor with promising results for the prevention of incisional hernias in experimental models [19, 20] might be translated into clinical options.
In this study, 6 out of 10 patients with ostomy closure site hernias had symptoms related to the presence of hernia, with pain being the most common. None of the patients with USG-detected hernias had symptoms. Therefore, recommendations for the treatment of these USG-detected hernias remains unclear. In our previous study, only 33% of patients with a parastomal hernia complained of minor symptoms and, therefore, only a minority had hernia repair. On the other hand, high rates of morbidity (65%) and the recurrence (38%) of parastomal hernia repairs prohibits surgery as a choice for these patients [21]. But it appears that ostomy closure site hernias are more commonly symptomatic and surgery is more commonly required. Surgery for these hernias is technically easier and the success rate is higher when compared with parastomal hernias. Ostomy closure site hernias should be regarded as incisional hernias and repaired with mesh [22].
In this study, we found a high rate of abdominal incisional hernia of 45% with physical examination alone, and this rate increased to 58% when USG was combined. This is a very high incisional hernia rate, but 52% of these patients had a Hartmann’s procedure as the initial operation and, thus, they had a re-laparotomy using the previous incision for closure. Interestingly, the group of patients having incisional hernias have a four-fold increased risk of having closed ostomy site hernias. This might be due to mechanical unfavorable properties of the abdominal wall in patients with incisional hernias. This issue is addressed in the study of DuBay et al. [23], in which incisional herniation has been found to be responsible for inducing decreased abdominal wall compliance via oblique muscle atrophy and fibrosis. BMI, age, gender, ostomy type, and surgical site infection did not have a significant effect on incisional hernia formation.
Only 61% of alive patients were evaluated in this study; the remainder did not accept the invitation to be included. At the same time, the median 26-month follow-up is a relatively short period for the development of hernias and, therefore, the incidences are subject to change. However, a 32% incidence of ostomy closure site hernia and a 58% incidence of incisional hernia at the laparotomy wound reflect a significant long-term consequence of ostomy formation. Closure of the enterostomy site should be regarded as a hernia repair rather than a simple fascial closure. USG is a valuable tool in determining the true incidence of hernias through enterostomy closure sites.
References
Hoffman MS, Barton DPJ, Gates J, Roberts WS, Fiorica JV, Finan MA, Cavanagh D (1992) Complications of colostomy performed on gynecologic cancer patients. Gynecol Oncol 44:231–234
Jänes A, Cengiz Y, Israelsson LA (2004) Preventing parastomal hernia with a prosthetic mesh. Arch Surg 139:1356–1358
Londono-Schimmer EE, Leong AP, Phillips RK (1994) Life table analysis of stomal complications following colostomy. Dis Colon Rectum 37:916–920
Cingi A, Cakir T, Sever A, Aktan AO (2006) Enterostomy site hernias: a clinical and computerized tomographic evaluation. Dis Colon Rectum 49:1559–1563
Parks SE, Hastings PR (1985) Complications of colostomy closure. Am J Surg 149:672–675
Berne JD, Velmahos GC, Chan LS, Asensio JA, Demetriades D (1998) The high morbidity of colostomy closure after trauma: further support for the primary repair of colon injuries. Surgery 123:157–164
Wong KS, Remzi FH, Gorgun E, Arrigain S, Church JM, Preen M, Fazio VW (2005) Loop ileostomy closure after restorative proctocolectomy: outcome in 1,504 patients. Dis Colon Rectum 48:243–250
van de Pavoordt HDWM, Fazio VW, Jagelman DG, Lavery IC, Weakley FL (1987) The outcome of loop ileostomy closure in 293 cases. Int J Colorectal Dis 2:214–217
Jamadar DA, Jacobson JA, Moraq Y, Girish G, Dong Q, Al-Hawary M, Franz MG (2007) Characteristic locations of inguinal region and anterior abdominal wall hernias: sonographic appearances and identification of clinical pitfalls. AJR Am J Roentgenol 188:1356–1364
Thomson JP, Hawley PR (1972) Results of closure of loop transverse colostomies. Br Med J 3:459–462
Porter JA, Salvati EP, Rubin RJ, Eisenstat TE (1989) Complications of colostomies. Dis Colon Rectum 32:299–303
Hesselink VJ, Luijendijk RW, de Wilt JH, Heide R, Jeekel J (1993) An evaluation of risk factors in incisional hernia recurrence. Surg Gynecol Obstet 176:228–234
van der Linden FT, van Vroonhoven TJ (1998) Long-term results after surgical correction of incisional hernia. Neth J Surg 40:127–129
Carne PW, Robertson GM, Frizelle FA (2003) Parastomal hernia. Br J Surg 90:784–793
Ballas KD, Rafailidis SF, Marakis GN, Pavlidis TE, Sakadamis AK (2006) Intraperitoneal ePTFE mesh repair of parastomal hernias. Hernia 10:350–353
Marimuthu K, Vijayasekar C, Ghosh D, Mathew G (2006) Prevention of parastomal hernia using preperitoneal mesh: a prospective observational study. Colorectal Dis 8:672–675
Israelsson LA (2005) Preventing and treating parastomal hernia. World J Surg 29:1086–1089
Geisler DJ, Reilly JC, Vaughan SG, Glennon EJ, Kondylis PD (2003) Safety and outcome of use of nonabsorbable mesh for repair of fascial defects in the presence of open bowel. Dis Colon Rectum 46:1118–1123
Franz MG, Kuhn MA, Nguyen K, Wang X, Ko F, Wright TE, Robson MC (2001) Transforming growth factor beta(2) lowers the incidence of incisional hernias. J Surg Res 97:109–116
Dubay DA, Wang X, Kuhn MA, Robson MC, Franz MG (2004) The prevention of incisional hernia formation using a delayed-release polymer of basic fibroblast growth factor. Ann Surg 240:179–186
Rieger N, Moore J, Hewett P, Lee S, Stephens J (2004) Parastomal hernia repair. Colorectal Dis 6:203–205
Burger JW, Luijendijk RW, Hop WC, Halm JA, Verdaasdonk EG, Jeekel J (2004) Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg 240:578–583
DuBay DA, Choi W, Urbanchek MG, Wang X, Adamson B, Dennis RG, Kuzon WM Jr, Franz MG (2007) Incisional herniation induces decreased abdominal wall compliance via oblique muscle atrophy and fibrosis. Ann Surg 245:140–146
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cingi, A., Solmaz, A., Attaallah, W. et al. Enterostomy closure site hernias: a clinical and ultrasonographic evaluation. Hernia 12, 401–405 (2008). https://doi.org/10.1007/s10029-008-0355-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-008-0355-3