Abstract
Introduction
Intercostal herniation of abdominal contents through a diaphragmatic defect is rare. We report a case of transdiaphragmatic intercostal hernia secondary to blunt trauma, initially misdiagnosed as lipoma, later confirmed by CT scan.
Methods
We present a case of a 77-year-old who was involved in a motor vehicle accident and sustained a hand fracture. Later that year his wife noticed an egg-shaped soft swelling on his right chest wall. He was seen in the minor operative clinic, and a lipoma excision was attempted when it was found to be an intercostal hernia. Colon was seen in the hernial pouch.
Results
Anatomically, the chest wall is weak from the costochondral junction to the sternum because of lack of external intercostal muscle support, and from the costal angle posteriorly to the vertebrae because of lack of internal intercostal musculature. The integrity of the thoracic cage is disrupted by tears of the intercostal musculature between fractured ribs. This defect leads to separation of the ribs and development of a potential weakened space for hernia. This chest wall muscular weakness can occur anywhere and can be more pronounced if it occurs at anatomically weakened areas. In the presence of associated diaphragmatic rupture, there is herniation of abdominal viscera. The treatment includes immediate surgical repair either by abdominal or thoracoabdominal approach.
Conclusions
A thorough physical examination may suggest the diagnosis, but confirmation by chest radiograph, CT scan, and sometimes by gastrointestinal contrast studies is often helpful for preoperative planning. A high index of suspicion for diaphragmatic injury or intercostal herniation during the initial evaluation, coupled with chest and abdominal diagnostic testing once the patient is stable, can avert undue delay in diagnosis and catastrophe from incarceration of a hernia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Transdiaphragmatic intercostal hernias attributable to blunt trauma have rarely been reported in the literature. The first descriptions of traumatic diaphragmatic rupture (TDR) are credited to Sennertus (1541) and Ambroise Paré (1579) [1]. A comprehensive review of medical literature was published by Carter et al. in 1951 [2], Hood in 1971 [3], and others later on [4, 5].
Chest wall intercostal hernias occur primarily as herniation of lung tissue with a positive cough impulse. Roland is credited with reporting the first case of hernia of the lung in 1499 [6].
Intercostal herniation of abdominal contents through the diaphragmatic defect is a very rare occurrence. Croce and Mehta [7] first coined the term intercostopleuroperitoneal hernia in a publication with a case report in 1979. Maurer and Blades [6] had given an excellent description of four such cases 33 years earlier in 1946. Cole et al. [8] presented a new case with the term transdiaphragmatic intercostal hernia (TDIH).
We report a case of transdiaphragmatic intercostal hernia secondary to blunt trauma from a head-on collision initially misdiagnosed as lipoma, later confirmed by CT scan.
Case report
The patient is a 77-year-old man who was seen in the thoracic surgery clinic earlier this year for evaluation of his right intercostal hernia. Early last year he was a passenger in a motor vehicle that was involved in a head-on collision. The patient sustained only fracture of his hand during the accident. Later the patient’s wife noticed an “egg-shaped lump” on his right chest wall. The patient noted progressive enlargement of the soft lump over the year.
The past history was marked by obesity, diabetes mellitus, hypertension, hyperlipidemia, gout, vitamin B12 deficiency, low testosterone, degenerative disk disease, depression, chronic myofascial pain syndrome, peripheral edema, prostatism, and urinary urgency. On admission his physical examination was unremarkable. The patient, a retired watch maker, was an elderly frail Asian male who looked his age.
The patient was seen in the minor surgery clinic, and a lipoma excision was attempted. It was found at that visit to represent not a lipoma, but a hernia on the right chest wall. Examination of the right lateral chest wall showed a reducible defect, which appeared to be filled with bowel in its hernia sac over the lower right chest in the area of the eighth, ninth, and tenth ribs. A CT scan followed; the findings confirmed the diagnosis.
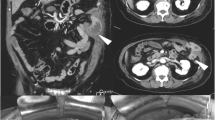
Contrast-enhanced CT study of abdomen and pelvis
There was a focal upper abdominal wall defect in the lateral aspect at about the seventh, eighth or ninth intercostal space (Fig. 1). Opacified ascending colon was noted within the hernia pouch (Fig. 2). The superior lateral aspect of the gallbladder fundus was in close proximity to the ascending colon. The partially opacified bowel loops were otherwise unremarkable without evidence of an obstruction. Enhancement of small bowel mesentery was unremarkable without evidence of an ischemic change.
The liver, gallbladder, pancreas, spleen, and right adrenal gland were unremarkable. The bladder and distal ureters were unremarkable. Interstitial prominence was noted in the right anterior lung base with possible tiny lung nodule in the subpleural space measuring about 3.0 mm in size. No pleural effusion was noted.
Procedure in detail
The patient was taken to the operating theater and placed in a lateral posture. The abdomen and right chest were prepped and draped in standard sterile manner.
Through a supraumbilical incision, a Veress needle was inserted and pneumoperitoneum established. A 45-degree laparoscope was then advanced through a 5-mm port in the midline. Three additional working ports were placed in a subcostal location on the right. A 10-mm port was placed most inferiorly toward the iliac fossa.
The right colon and omentum were found to leave the peritoneal cavity proper through a sac in a defect over the right lateral abdominal wall over the arch of the right costal region. By traction on the contents and sharp dissection, the colon and omentum were taken down from within the hernia sac. The defect, now visualized, was measured. A composite Gore–Tex Marlex mesh material was then sized and advanced into the peritoneal cavity through the right lower 10-mm port. The grasping suture in the central portion of the patch was then passed through the skin in the mid-portion of the defect to allow for placement of the patch onto the abdominal wall. Using an autosuture tacking device, the composite patch was secured to the abdominal wall sequentially over its lateral edges.
Marcaine(0.25%) was infiltrated at the port sites. The port sites were inspected for hemostasis. The pneumoperitoneum was released and the ports removed. The skin was closed with a #4-0 Biosyn subcuticular suture. An occlusive dressing was applied. The patient was extubated and transferred to the recovery room in stable condition.
Discussion
Transdiaphragmatic intercostal hernias resulting from blunt trauma are rare, with few cases of this type reported in the literature. In a review of world literature [9], only 11 published cases were reported [6–14]. TDIH resulted after penetrating trauma in six cases and direct blunt trauma in three cases. The remaining three patients had chronic obstructive pulmonary disease and a hernia that developed after spontaneous rib fractures that were induced by violent coughing episodes [7, 8, 10].
The time interval between the initial trauma and the repair of the hernia varied greatly, from immediately after the trauma to 36 years later. The average duration was 5 months. All of the patients were men, ranging in age from 19 to 73 years. TDR has been reported to occur more commonly on the left side. In two recent comprehensive reviews of medical literature, the incidence of TDR was 68.5 to 77% on the left side [4, 5]. TDR is associated with a high incidence of rib fractures [3, 15–19], with an overall incidence of 47% (range 23–70%) [19]. In TDIH, associated rib fractures were reported more frequently [10 of 12 cases (83%)]. The ninth and tenth ribs were the most commonly fractured. TDIH developed in the ninth interspace in 75% of the cases (9 of 12).
Hruska et al. [14] reported a case of TDIH where bowel herniated between fractured seventh and eigthth ribs [19]. Immediate surgery revealed disruption of intercostal musculature from the posterior axillary line to the costochondral junction of the seventh and eighth ribs. Although rib fractures may be associated with diaphragmatic rupture, concomitant disruption of intercostal musculature is rarely seen. Intercostal pulmonary hernia commonly involves the anterolateral midthoracic cage; however, it can occur anywhere.
Anatomically, the chest wall is weak from the costochondral junction to the sternum because of lack of external intercostal muscle support, and from the costal angle posteriorly to the vertebrae because of lack of internal intercostal musculature [20]. The integrity of the thoracic cage is disrupted by tears of the intercostal musculature between fractured ribs. This defect leads to separation of the ribs and development of a potential weakened space for hernia [10]. This chest wall muscular weakness can occur anywhere and can be more pronounced if it occurs at anatomically weakened areas. This weakness can lead to development of intercostal herniation of the lung. However, in the presence of associated diaphragmatic rupture, there is herniation of abdominal viscera (TDIH) [19]. The forces of violent coughing can tear the intercostal muscles and even fracture the osteoporotic ribs in debilitated patients [21].
The delayed presentation of intercostal hernia results from progressive strain and stretching on the damaged intercostal musculature on resumption of physical activity and rehabilitation [12]. At the same time, there is further enlargement of associated diaphragmatic tears with larger herniation of intra-abdominal viscera. The dynamics of physical activity, respiration, coughing or straining, and the peritoneal pleural pressure gradient lead to gradual enlargement of the intercostal hernia, typically with a delayed presentation. The diaphragm also can become severed from its attachment to the ribs, especially if it is damaged or fractured with subsequent hernia [12]. TDIH presents months to years after the initial traumatic insult. Positive pressure ventilation in a seriously injured patient may initially delay herniation through the diaphragmatic defect. The omentum or adjoining viscus (liver on the right side) may plug a small rent. Diaphragmatic ruptures progressively enlarge over time with symptomatic hernia, as noted in this report.
The diagnosis of TDIH resulting from blunt trauma may be easier than diagnosing blunt diaphragmatic rupture alone. The diagnosis of diaphragmatic rupture is delayed in 5–35% of cases, with delays from several days to 48 years reported [17, 21]. All authors agree that a high index of suspicion is essential during initial evaluation of the patient with blunt thoracoabdominal trauma to avoid overlooking diaphragmatic injury, because the signs on physical examination can be subtle. Intercostal hernias, on the other hand, are usually more obvious and should be suspected in any patient who has a reducible thoracic wall mass.
Clinically, all patients with TDIH presented with a reducible palpable soft tissue lump in the lower chest wall with a positive cough impulse. By positioning the patient on his or her contralateral side, a defect is usually visible as a large furrowed defect between the ribs [10]. An increase in swelling on inspiration and a decrease in the size of the hernia on expiration suggest TDIH. In contrast, a paradoxical change in size of the hernia occurs in pulmonary intercostal hernia [19]. A pulmonary hernia increases on expiration and decreases on inspiration.
Physical examination, chest radiograph, and CT scan studies are diagnostic of TDIH [18]. Clinical findings and chest radiograph were not diagnostic initially in the present case report.
The treatment of transdiaphragmatic intercostal hernias resulting from acute blunt trauma should include immediate surgical repair. An abdominal approach is favored by some authors because of the large number of associated intra-abdominal injuries [22, 23]. In a case in which diagnosis was delayed for 3 months as in this present one, surgeons often used a thoracoabdominal incision and repaired the costal margin first to stabilize the chest wall and remove tension from the diaphragmatic margins [12]. In the absence of any concomitant abdominal injuries, this would be a favorable approach. There are some proponents of initial thoracotomy for right-sided diaphragmatic ruptures because of the difficulty of most right-sided repairs when approached from the abdomen, and in the absence of abdominal injury this would be appropriate. Most authors recommend evaluation of each patient individually to determine which approach is most suitable based on the extent of associated injuries. In the setting of delayed diagnosis, repair will usually require an initial thoracotomy to facilitate the takedown of adhesions and direct irrigation of the thorax if visceral rupture has occurred [17, 24].
Conclusion
Transdiaphragmatic intercostal hernias are rarely reported in the literature. A thorough physical examination may suggest the diagnosis, but confirmation by chest radiograph, CT scan, and sometimes by gastrointestinal contrast studies is often helpful for preoperative planning. A high index of suspicion for diaphragmatic injury or intercostal herniation during the initial evaluation, coupled with chest and abdominal diagnostic testing once the patient is stable, can avert undue delay in diagnosis and catastrophe from incarceration of a hernia.
References
Hamby W (1960) The case reports and autopsy records of Ambroise Paré. Charles C Thomas, Springfield, IL
Carter BN, Giuseffi J, Felson B (1951) Traumatic diaphragmatic hernia. AJR Am J Roentgenol 65:56–72
Hood RM (1971) Traumatic diaphragmatic hernia. Ann Thorac Surg 12:311–324
Sharma O (1999) Pericardio-diaphragmatic rupture: five new cases and literature review. J Emerg Med 17:963–968
Shah R, Sabanathan S, Mearns AJ, Choudhury AK (1995) Traumatic rupture of diaphragm. Ann Thorac Surg 60:1444–1449
Maurer E, Blades B (1946) Hernia of the lung. J Thorac Surg 15:77–98
Croce EJ, Mehta VA (1979) Intercostal pleuroperitoneal hernia. J Thorac Cardiovasc Surg 77:856–857
Cole FH, Miller MP, Jones CV (1986) Transdiaphragmatic intercostal hernia. Ann Thorac Surg 41:565–566
Sharma OP, Duffy B (2001) Transdiaphragmatic intercostal hernia: review of the world literature and presentation of a case. J Trauma 50(6):1140-1143
Rogers FB, Leavitt BJ, Jensen PE (1996) Traumatic transdiaphragmatic intercostal hernia secondary to coughing: case report and review of the literature. J Trauma 41:902–903
Francis D, Barnsky WC (1979) Intercostal herniation of abdominal contents following a penetrating chest injury. Aust N Z J Surg 49:357–358
Serpell JW, Johnson WR (1994) Traumatic diaphragmatic hernia presenting as an intercostal hernia: case report. J Trauma 36:421–423
Jain SK (1995) Delayed, traumatic intercosto-diaphragmatic hernia of colon. Injury 26:204–206
Hruska LA, Corry D, Kealey GP (1998) Transdiaphragmatic intercostal hernia resulting from blunt trauma: case report. J Trauma 45:822–824
Ward RE, Flynn TC, Clark WP (1981) Diaphragmatic disruption secondary to blunt abdominal trauma. J Trauma 21:35–38
Williams RS (1982) Traumatic rupture of the diaphragm. Med J Aust 1:208–211
Johnson CD (1988) Blunt injuries of the diaphragm. Br J Surg 75:226–230
Beauchamp G, Khalfallah A, Girard R, Dube S, Laurendeau F, Legros G (1984) Blunt diaphragmatic rupture. Am J Surg 148:292–295
McElwee TB, Myers RT, Pennel TC (1984) Diaphragmatic rupture from blunt trauma. Am Surg 50:143–149
Saw EC, Yokoyama T, Lee EC, Sargent EN (1976) Intercostal pulmonary hernia. Arch Surg 111:548–551
Arendrup HC, Jensen BS (1982) Traumatic rupture of the diaphragm. Surg Gynecol Obstet 154:526
Adamthwaite DN (1983) Traumatic diaphragmatic hernia. Surg Ann 15:73
Asensio JA, Demetriades D, Rodriguez A (1996) Injury to the diaphragm. In: Feliciano DV, Moore EE, Mattox KL (eds) Trauma, 3rd edn. Appleton and Lange, Stanford, pp 474–477
Lee WC, Chen RJ, Fang JF et al (1994) Rupture of the diaphragm after blunt trauma. Eur J Surg 160:479
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Biswas, S., Keddington, J. Soft right chest wall swelling simulating lipoma following motor vehicle accident: transdiaphragmatic intercostal hernia. A case report and review of literature. Hernia 12, 539–543 (2008). https://doi.org/10.1007/s10029-008-0342-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-008-0342-8