Abstract
Bicarbonate buffered local anaesthetic solutions are known to reduce the pain of infiltration. However, its efficacy in reducing the pain of infiltration in patients undergoing inguinal hernia repair has never been tested. This study aims to test the efficacy of bicarbonate buffered solution in reducing the pain of infiltration and pain for the total surgical procedure in a series of patients undergoing elective inguinal hernia repair. Forty consecutive male patients with unilateral, reducible inguinal hernias were studied prospectively. All patients underwent surgery under local anaesthesia, the first 20 with unbuffered solution and the next 20 using buffered solution. Pain scores were obtained for the infiltration in the anaesthetic room and for the total surgical procedure. In addition, satisfaction scores were obtained at the end of the procedure. The mean pain score for the initial infiltration of unbuffered anaesthetic was 3.00 (range 0–5), and for the buffered anaesthetic it was 1.45 (range 0–4), P=0.02. The mean pain score for the entire procedure for the unbuffered group was 3.05 (range 0–6), and for the buffered group it was 1.45 (range 0–5), P=0.02. The patient satisfaction rate was higher with the buffered solution compared to unbuffered solution (P<0.05). There were no complications reported with either solution. Buffered local anaesthetic solution significantly reduces the perceived pain of inguinal hernia repair, both during the infiltration and during the procedure itself. It is safe to administer and it results in a high rate of patient satisfaction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgical repair of groin hernias is one of the most commonly performed procedures in the Western world [1]. Several randomised and retrospective studies have shown that inguinal hernia repair under local anaesthesia results in less postoperative analgesic requirements and side-effects, reduced hospital stay, lower costs and shorter recovery times [2–5]. However, one of the commonly perceived problems of local anaesthesia is the pain of infiltration. This has been likened to a burning, stinging sensation, and can be extreme enough for patients to be dissatisfied with the procedure [6] and decline further local anaesthetic surgery [7].
Several strategies were suggested previously to reduce the amount of pain at infiltration including warming the local anaesthetic agent to body temperature [8, 9] slow administration of the local anaesthetic [10], withdrawing the needle while injecting [11], and application of topical anaesthetic ointment [12] but with little success.
The pain associated with local anaesthetic infiltration is mostly due to the hydrogen ion concentration which imparts an acidic nature to local anaesthetic solutions [13, 14]. Recent randomised trials have confirmed the efficacy of buffered local anaesthetic mixture with bicarbonate in reducing the amount of pain perceived during a variety of operations [7, 15]. This applies especially to the amide group of local anaesthetics such as lignocaine and bupivacaine. An addition of 8.4% sodium bicarbonate to local anaesthetic solution regardless of the presence of adrenaline buffers the solution without risk of precipitation [16].
Several authors have used bicarbonate buffered local anaesthetic solution for local anaesthetic inguinal hernia repair [17–20], but to date no study has compared this with unbuffered local anaesthetic solution in reducing the pain of infiltration during inguinal hernia repair. One of the commonly encountered problems during local anaesthetic inguinal hernia repair is the shortage of local anaesthetic solution, especially in obese patients, who require large volumes. We have developed a large volume mixture of 100 ml of buffered local anaesthetic with adrenaline to counter this problem. The purpose of this study was to assess the difference in pain scores and the patient satisfaction for local anaesthetic inguinal hernia repair both during infiltration and the surgical procedure using buffered and unbuffered local anaesthetic solution.
Methods
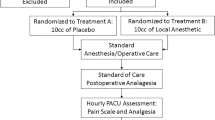
Forty consecutive male patients with unilateral, reducible inguinal hernias were recruited into the study. The first 20 patients underwent surgery under local anaesthesia using unbuffered local anaesthetic solution. The remaining 20 patients underwent surgery using a buffered local anaesthetic solution. All patients had a tension-free Lichtenstein inguinal hernia repair without pre-medication or sedation, and were monitored during surgery by pulse oximetry. A member of the operating theatre staff accompanied the patient throughout the procedure.
The local anaesthetic mixture consisted of:
-
20 ml of 2% lignocaine with 1:200,000 adrenaline (Hameln, UK)
-
30 ml of 0.5% bupivacaine with 1:200,000 adrenaline (Astrazeneca, UK)
-
50 ml of 0.9% saline
This results in a total volume of 100 ml (400 mg of Lignocaine and 150 mg of Bupivacaine based on a 70 kg man). (The maximum dose of lignocaine with adrenaline is 7 mg/kg, and of bupivacaine with adrenaline is 3 mg/kg). To buffer the lignocaine, 6 ml of 8.4% sodium bicarbonate (Fresenius, UK) was added, giving a pH of 7.0.
1.5 g of intravenous cefuroxime was administered in the anaesthetic room to all patients. In the anaesthetic room, approximately 20 ml of the local anaesthetic mixture was infiltrated along the line of incision in the subcutaneous plane, around the pubic tubercle and the deep ring. The patients were asked to give a pain score (0 representing no pain, and 10 representing the worst pain they can possibly imagine) for the initial injection in the anaesthetic room.
A skin and external oblique aponeurosis incision was then performed, after which subaponeurotic infiltration of the mixture deep to the external oblique layer was undertaken. Further infiltration was performed into the spermatic cord avoiding the testicular vessels, nerves and the vas deferens. The sac was either reduced or excised according to the surgeon’s preference and Lichtenstein repair was performed. In all cases, the mesh was soaked in iodine antiseptic prior to the tension-free mesh repair. At the end of the procedure, patients were asked to give a pain score for the whole procedure. In addition, satisfaction scores were obtained for the total procedure. The patients were planned for discharge later the same day provided they were not living alone.
Results
We recruited patients into the study by taking 40 consecutive patients who were on the waiting list for unilateral inguinal hernia repair under local anaesthetic. The median age of the study group was 68 years (range 29–83). The median body mass index (BMI) of the study group was 30 (range 20.9–34.6).
The mean pain score for the initial infiltration of non-buffered anaesthetic was 3.00 (range 0–5), and for the buffered anaesthetic it was 1.45 (range 0–4), P=0.02 (Fig. 1). The mean pain score for the entire procedure for the unbuffered group was 3.05 (range 0–6), and for the buffered group it was 1.45 (range 0–5), P=0.02 (Fig. 2). The results are further summarised in Table 1. The P values were calculated using the Wilcoxon rank test.
The number of patients who were highly satisfied with the procedure was higher in the buffered group compared to the unbuffered group 12 versus 3 (P<0.05). One patient in the unbuffered group was dissatisfied with the procedure.
Discussion
This study demonstrates that addition of sodium bicarbonate to buffer local anaesthetic solution significantly reduces the perceived pain of inguinal hernia repair, both during the administration of the local anaesthetic solution and during the procedure itself. Buffered local anaesthetic solution is associated with a higher level of patient satisfaction.
Since Mackay et al. [21] first reported the efficacy of buffered lidocaine in reducing the pain of infiltration, several studies have shown that such solutions decrease the pain of administration without decreasing the onset of duration of anaesthesia [22–26]. Local anaesthetics work by diffusing through the perineural sheath and attaching to sodium channels. Only the non-ionised fraction of the drug is able to cross the nerve membrane. Commercial preparations of anaesthetics are marketed at a pH of 6 for maximum solubility and stability, and at this pH only 1% of the drug is non-ionised [13]. The addition of adrenaline to local anaesthetics further increases the acidity and decreases the non-ionised fraction. By neutralising the solution with sodium bicarbonate to a pH of 7, closer to the pKa of the drug, the fraction of non-ionised molecules increases to 11%. This reduction of pH reduces the tissue irritation associated with infiltration of a more acidic compound and also the onset of analgesia can be more rapid [27, 28]. Interestingly, some studies have shown that nociceptors may be less sensitive to the non-ionised form [21] thereby reducing the pain of infiltration.
A recent study [15] has shown that buffered lignocaine reduces the pain of infiltration but no significant difference was found in the pain scores for the whole procedures. In contrast, results from our study have shown that buffered solution not only reduces the pain of infiltration but also the perceived pain for the whole procedure, specifically for inguinal hernia repair.
Specialist hernia centres performing regular local anaesthetic hernia repairs routinely administer intravenous sedatives (midazolam) during local anaesthetic inguinal hernia repair [18, 29]. In this study, none of the patients in either group received any form of sedation facilitating accurate estimation of pain scores at infiltration and for the total procedure.
Despite receiving widespread acceptance overseas, local anaesthetic inguinal hernia repair is not popular with surgeons in the UK. Previous studies have shown that only 5–10% of inguinal hernia repairs are performed under local anaesthesia with the majority of repairs being performed either under general or regional anaesthesia [30–33]. The majority of local anaesthetic hernia repairs are being performed either in private specialist hernia centres [18] or district general hospitals with established hernia service [29]. In the published literature, the use of buffered local anaesthetic solution for inguinal hernia repair is limited only to such centres.
Previous studies have reported higher patient satisfaction rates with local anaesthetic inguinal hernia repair [1, 2, 34]. However, one study [35] has reported a patient dissatisfaction rate of 8% following local anaesthetic inguinal hernia repair, mainly due to intraoperative discomfort or pain and it has been suggested that a large dose ilioinguinal–iliohypogastric block in combination with stepwise infiltration might result in reduced intraoperative discomfort. We feel the large volume of the local anaesthetic mixture used in our study has achieved this objective. The number of patients with higher satisfaction scores was greater in the buffered group compared to the non-buffered group.
Previous studies have used sparing amounts of local anaesthetic solution due to the potential to produce systemic toxicity with large volumes of local anaesthetic [3, 5]. The local anaesthetic mixture used in this study allowed us to use large quantities of the solution especially necessary for obese patients (the median BMI of the study group was 30).
In summary, this study demonstrates that buffered local anaesthetic solution significantly reduces the perceived pain of inguinal hernia repair. The use of large volume buffered local anaesthetic solution is safe and effective for repair of inguinal hernias in both obese and non-obese patients and more widespread use is recommended.
References
Baskerville PA, Jarret PEM (1983) Day case inguinal hernia. Ann R Coll Surg Engl 65:224–225
Song D, Grelich NB, White PF, Tongier WK (2000) Recovery profiles and costs of anaesthesia for outpatient unilateral inguinal herniorrhaphy. Anaesth Analg 91:876–881
Gonullu NN, Cubukcu A (2002) Comparison of local and general anesthesia in tension-free (Lichtenstein) hernioplasty: a prospective randomised trial. Hernia 6:29–32
Ozgun H, Nil Kurt M, Kurt I, Cevikel MH (2002) Comparison of local, spinal and general anaesthesia for inguinal herniorrhaphy. Eur J Surg 168:455–459
Merhav H, Rothstein H (1993) A comparison of pulmonary functions and oxygenation following local, spinal and general anaesthesia in patients undergoing inguinal hernia repair. Int Surg 78:257–261
Callesen T, Bech K, Nielsen R, Anderson J, Hesselfeldt P, Roikjaer O, Kehlet H (1998) Pain after groin repair. Br J Surg 85:1412–1414
Masters JE (1998) Randomised control trial of pH buffered lignocaine with adrenaline in outpatient operations. Br J Plast Surg 51:385–387
Bloom LH, Scheie HG, Yanoff M (1984) The warming of local anaesthetic agents to decrease discomfort. Opthal Surg 15:603
Finkel LI, Berg DJ (1987) Heating lidocaine appears to prevent painful injection (letter). AJR Am J Roentgenol 148:658
Rund DA (1986) Essentials of emergency medicine, 2nd edn. Norwalk conn: Appleton-century-crofts, p 274
Lipchik EO (1988) A technique to decrease the pain of lidocaine injection (letter). AJR Am J Roentgenol 150:950–951
McMillan AS, Walshaw D, Meechan JG (2002) The efficacy of Emla and 5% lignocaine gel for anaesthesia of human gingival mucosa. Br J Oral Maxillofac Surg 38(1):58–61
Matsumoto AH, Reifsnyder AC, Hartwell GD, Angle JF, Bayne Selby J Jr, Tegtmeyer CJ (1994) Reducing the discomfort of Lidocaine administration through pH buffering. J Vasc Intervent Radiol 5:171–175
Shafi T, Koay P (1998) Randomised prospective masked study comparing patient comfort following the instillation of topical proxymetacaine and amethocaine. Br J Ophthalmol 82:1285–1287
Fitton AR, Ragbir M, Milling MAP (1996) The use of pH adjusted lignocaine in controlling operative pain in the day surgery unit: a prospective, randomised trial. Br J Past Surg 49:404–408
Milner QJ, Guard BC, Allen JG (2000) Alkalinization of amide local anaesthetics by addition of 1% sodium bicarbonate solution. Eur J Anaesth 17(1):38–42
Gianetta E, De Cian F, Cuneo S, Friedman D, Vitale B, Marinari G, Baschieri G, Camerini G (1997) Hernia repair in elderly patients. Br J Surg 84:983–985
Kark AE, Kurzer MN, Belsham PA (1998) Three thousand one hundred seventy-five primary inguinal hernia repairs: advantages of ambulatory open mesh repair using local anaesthesia. J Am Coll Surg 186(4):447–456
Subramaniam P, Leslie J, Gourlay C, Clezy JKA (1998) Inguinal hernia repair: a comparison between local and general anaesthesia. Aust N Z J Surg 68:799–800
Amid PK, Shulman AG, Lichtenstein IL (1994) Local anesthesia for inguinal hernia repair step-by-step procedure. Ann Surg 220:735–737
Mackay W, Morris R, Mushlin P (1987) Sodium bicarbonate attenuates pain on skin infiltration with lidocaine, with or without epinephrine. Anaesth Analg 66:572–574
Christoph RA, Buchanan L, Begalla K, Schwartz S (1988) Pain reduction in local anaesthetic administration through Ph buffering. Ann Emerg Med 17:117–120
Orlinsky M, Hudson C, Chan L, Deslauriers R (1992) Pain comparison of unbuffered versus buffered lidocaine in local wound infiltration. J Emerg Med 10:411–415
Metzinger SE, Bailey DJ, Boyce RG, Lyons GD (1992) Local anaesthesia in rhinoplasty: a new twist? Ear Nose Throat J 71:405–406
Eccarius SG, Gordon ME, Parelman JJ (1990) Bicarbonate-buffered lidocaine-epinephrine-hyaluronidase for eyelid anaesthesia. Ophthalmology 97(11):1499–1501
Stewart JH, Chinn SE, Cole GW, Klien JA (1990) Neutralized lidocaine with epinephrine for local anaesthesia-11. J Dermatol Surg Oncol 16:842–845
DiFazio CA, Carron H, Grosslight KR, Moscicki JC, Bolding WR, Johns RA (1986) Comparison of ph-adjusted lodocaine solutions of epidural anaesthesia. Anaesth Analg 65:760–764
DeJong RH (1977) Local anaesthetics. Springfield 111:Charles C Thomas, pp 42–50
Kingsnorth AN, Bowley DMG, Porter C (2003) A prospective study 1000 hernias: results of the Plymouth Hernia Service. Ann R Coll Surg Engl 85:18–22
Bay-Nielsen M, Kehlet H, Strand L, Malmstrom J, Andersen FH, Wara P, Juul P, Callesen T (2001) Quality assessment of 26,304 herniorrhapies in Denmark: a prospective nationwide study. Lancet 358:1124–1128
Hair A, Paterson C, Wright D, Baxter JN, O, Dwyer PJ (2001) Diagnosis of a femoral hernia in the elective setting. J R Coll Surg Edinburgh 46:117–118
Nilsson F, Anderberg B, Bragmark M, Eriksson T, Fordell R, Happaniemi S, Heuman R, Kald A, Stubberod A, Svensson P (1993) Hernia surgery in a defined population: improvements possible in outcome and cost effectiveness. Ambul Surg 1:150–153
O’ Riordan DC, Kingsnorth AN (1998) Audit of patient outcomes after herniorrhaphy. Surg Clin N Am 78:1129–1139
Flanagan LJR, Bascom JV (1981) Herniorrhaphies performed upon outpatients under local anaesthesia. Surgery Gynaecol Obstet 153:557–560
Callesen T, Bech K, Kehlet H (2001) One-thousand consecutive inguinal hernia repairs under unmonitored local anaesthesia. Anaesth Analg 93:1373–1376
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented at the 2nd International Hernia Congress: joint meeting of the AHS and EHS, June 2003, London.
Rights and permissions
About this article
Cite this article
Ball, E.L., Sanjay, P. & Woodward, A. Comparison of buffered and unbuffered local anaesthesia for inguinal hernia repair: a prospective study. Hernia 10, 175–178 (2006). https://doi.org/10.1007/s10029-005-0058-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-005-0058-y