Abstract
The popularity of laparoscopic repair of ventral hernias is increasing due to the apparent advantages of the procedure, but this approach is still a controversial technique. The aim of our study was to evaluate the mortality rate of laparoscopic ventral hernia repair and analyse the literature. The authors performed a prospective study in 90 patients with ventral hernia who were treated by laparoscopic repair. Clinical parameters and intra- and postoperative complications were evaluated. A case of mortality was reported due to a nonrecognised bowel injury. The mean follow-up (100%) was 42 months (range: 1–5 years). A bibliographical analysis was carried out (MEDLINE). Four bowel injuries were presented (4.4%): three recognised, which required conversion (two treated with minilaparotomy and completed afterwards by laparoscopy, and one by laparotomy); and one nonrecognised, which was re-operated on but evolved to sepsis and multiorgan failure and resulted in death in 48 h (1.1%). Four further mortality rates have been documented in the literature (0.6%, 1.1%, 3.1%, and 3.4% of their series). Bowel injury and mortality show a statistically significant tendency to decrease with the number of operations (P<0.05). In conclusion, in our study the risk of mortality with laparoscopic ventral hernia repair has been higher than 1%, which must be made known. It is a risk that depends on the surgeon’s experience but which does not seem to be predictable.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The laparoscopic ventral hernia repair is a technical option that attempts to improve the results of conventional surgery, and its popularity is increasing due to the apparent advantages of the procedure, but is still a controversial technique. This approach appears to modify the complications that can be expected after surgery. With open repair, the morbidity rate depends almost exclusively on the wound, but with the laparoscopic approach, the risk of visceral lesions and subsequent sepsis with fatal consequences might be significant [1, 2, 3, 4, 5, 6, 7]. The present study reports a personal case of nonrecognised bowel injury and death, and analyses the bibliography that exists on this problem.
Patients and methods
Patients
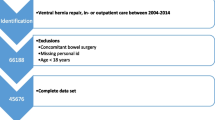
Between January 1998 and December 2002, 90 patients with ventral hernia were operated on by laparoscopic repair. All the patients were assessed in an Abdominal Wall Unit and duly informed of the process, for which their signed consent was obtained. Included were all patients aged over 30 years and giving their signed consent, with a hernia measuring >4 cm and <15 cm (except nonmidline hernias), and no cutaneous lesions. Excluded were neoplastic patients, those with acute infection or risk of sepsis, mentally disordered patients, and those not giving their signed consent.
Surgical technique
The repair was done using general anaesthesia and pneumoperitoneum, according to the closed technique (Veress needle). The position of the trocars depended on the size, location, and number of abdominal wall defects, usually three in a line along the left flank. After complete adhesiolysis of the abdominal wall without electrocautery (with endoscopic scissors or harmonic scalpel), the defect was covered with a double-layer mesh (Parietex, Sofradim, Trevoux, France), overlapping the edges of the defect by 5 cm all around, and fixed using helicoidal staples every 1 cm (Tacker, Origin Medsystems Inc., Menlo Park, Calif., USA).
Main outcome measures
All the patients were included in a follow-up protocol at the Surgery Day Hospital and reviewed as outpatients at 1 week, 1 month, 6 months, and each year. The parameters assessed were: clinical factors (age, sex, associated diseases, prior surgery, and hernia type according to Chevrel’s classification) and complications (bowel injury, seromas, haematomas, infection, abdominal wall pain, ileus, bowel obstruction, etc.). The mean follow-up (100%) was 42 months (median 40; range: 10–52 months).
Bibliographical analysis
Literature search
Computer searches of MEDLINE database for the dates January 1998 to May 2003 were performed using the keywords “ventral hernia”, “incisional hernia”, and “laparoscopy”. A manual search of the bibliographies of the identified papers was carried out to identify any additional articles.
Exclusion criteria
Criteria for exclusion were articles published in a language other than English, nonabdominal wall surgery (gynaecologic or urologic articles), letters or editorials, and articles with incomplete information (lacking rates of conversions, bowel lesions, re-operations, or mortality).
Statistical analysis
A descriptive statistical study was conducted of the data obtained. Proportions of categorical variables were analysed using the chi-square test and linear trend test. Statistical analysis was performed using SPSS statistical analysis software (SPSS Inc., v10.0, Chicago, Ill., USA). A P value of <0.05 was considered significant.
Results
The patients’ clinical features are shown in Table 1 and mortality in Table 2. During the operation, three bowel injuries were detected. In two patients, a small bowel enterotomy was exteriorised through a small laparotomy incision, enterorrhaphy and reinserted into the abdomen; no contamination occurred, and laparoscopy was completed. One patient required conversion to open procedure.
Case report
A 69-year-old ASA II woman presented with a history of gynaecologic surgery (hysterectomy and double adnexectomy), urologic surgery (colposuspension), and intestinal surgery (appendicectomy). She had a 6-cm-maximum-diameter infraumbilical midline ventral hernia. After preoperative tests (including CT), the patient was programmed for ambulatory surgical treatment. Surgery confirmed the defect, and when the adhesiolysis manoeuvres were begun, there was a block reduction of the hernia contents located subcutaneously in the ventral sac. The intestine was reviewed, but no leaks or bleeding were noted. In the immediate postoperative period, the patient presented with vomiting and was, therefore, admitted to hospital. Abdominal exploration was normal. Hypotension and coldness were reported at 24 h, signs of hypoperfusion were noted, and the patient was transferred to the ICU. Due to haemodynamic instability with no cardiogenic focus, abdominal CT was performed, which informed of abundant free fluid. With the suspicion of intra-abdominal sepsis, the patient underwent re-operation, which revealed a bowel perforation. Segmental ileal resection with anastomosis was performed and the mesh removed, and primary closure was done of the abdominal wall. The patient progressed to multiorgan failure and died 8 h after the re-operation (48 h after initial laparoscopic surgery).
Bibliographical analysis
Fifty-seven bowel injuries (3.4%) have been published: 45 observed and 12 unobserved (Table 3). Of the latter, eight developed sepsis and required treatment in intensive care units, and five died: four from multiorgan failure and one associated with hepatic disease during the early postoperative period. All the cases of mortality occurred between the first and third day postoperatively. We report the first case of mortality acknowledged in our country. The statistical analysis yields the following data: the total risk of bowel injury in the laparoscopic ventral hernia repair is 3.4%, that of unobserved lesions 0.7%, and that of mortality 0.3%. The number of bowel injuries and the mortality show a statistically significant tendency to decrease with the number of operations performed (P<0.05) (Table 4).
Discussion
Laparoscopic surgery of ventral hernias has proved to be an easy-to-perform technique, and most surgeons have begun to use it before its efficiency has been demonstrated by appropriate randomised studies. The first meta-analyses seem to confirm the benefit of the laparoscopic approach over open surgery in two specific parameters (morbidity and hospital stay), but they warn of the need to design more complete long-term studies that allow more reliable and final conclusions [1, 2, 3, 4, 5, 6, 7]. In this context, it seems that this approach has modified the complications that can be expected after surgery. With open repair, morbidity depends almost exclusively on the wound; it is rarely necessary to enter the abdominal cavity, but if it is entered, the viscera can be controlled directly and any injury visualised and repaired easily. With the laparoscopic approach, the risk of visceral lesions and mortality might be higher as supposed before. Including our case, the literature [8, 9, 10] contains five cases of mortality (0.6%, 1.1%, 3.1%, and 3.4% of their series), but the number of patients who progressed to sepsis and required intensive care was more than double. Thus, 18.5% of bowel injuries with the laparoscopic approach have not been observed during surgery, and this has led some patients to peritonitis and intra-abdominal sepsis, involving intensive care and a 0.3% risk of mortality [11, 12, 13]. Unlike the traditional approach, the laparoscopic technique always requires prior parietal adhesiolysis to carry out the repair. Therefore, the risk of bowel injury—whether or not observed—and subsequent evolution to sepsis, multiorgan failure, and death becomes a real possibility. This rapid evolution means that the follow-up time in the first few postoperative hours is fundamental for establishing a diagnosis of suspicion and proceeding to an early re-operation as the only means of preventing this process of peritoneal contamination, sepsis, multiorgan failure, death. Two bowel injury mechanisms have been described: (1) direct trauma from scissors or scalpel but with no intraoperative manifestation and (2) indirect lesion from some energy source and formation of a slough or ischaemic tissue, which subsequently necrotises and falls away, causing the perforation [14, 15, 16]. The most dangerous step in this technique is the adhesiolysis. We avoid electrosurgery as much as possible and do not recommend any other energy sources. We use sharp dissection for the majority of operations and never use harmonic scissors near the bowel. Harmonic scissors can be used for adhesiolysis of the hernial sac or scar surface. Our experience shows that traction and external-pressure manoeuvres reduce the contents of the sac in a cavity with multiple adhesions, and a high pneumoperitoneum can also cause a bowel injury without the aggressive agent coming into direct contact with the intestinal wall. As some authors have suggested, we find that bowel injury and mortality show a significant tendency to decrease as the surgeon’s experience increases, with the possibility of occurrence falling to below 1% after 50 cases [8, 9, 14, 15, 16]. Even if mortality depends on the surgeon’s experience, we must ask ourselves two questions: (1) Is it wise to perform this technique on an ambulatory basis? and (2) Is a “high-risk” group of patients predictable from hernia type, history, or CT? Our case shows that visceral lesions are not exclusive to large defects or patients considered high risk, as our patient was selected for ambulatory surgery because she was considered low-risk. Furthermore, this approach has enabled us to repair, without any problem, large lumbar hernias classed as high-risk because they required mobilisation of the colon. Therefore, any patient treated with this technique is susceptible to an intestinal lesion, which means that an adequate postoperative follow-up must always be guaranteed. If the ambulatory regimen is used, at least 8 h postoperative follow-up and a very strict fulfillment of the criteria for discharge must be guaranteed [17, 18]. In conclusion, laparoscopic ventral hernia repair implies a risk of mortality that must be made known, a risk that seems to depend on the surgeon’s experience but which does not appear to be predictable preoperatively.
References
Cassar K, Munro A. (2002) Surgical treatment of incisional hernia. Br J Surg 89:534–545
Goodney PP, Birkmeyer CM, Birkmeyer JD (2002) Short-term outcomes of laparoscopic and open ventral hernia repair. A meta-analysis. Arch Surg 137:1161–1165
Arnaud JP, Cervi C, Tuech JJ, Cattan F (1997) Surgical treatment of postoperative incisional hernias by intraperitoneal insertion of a Dacron mesh. A report on 220 cases. Hernia 1:97–99
Marchal F, Brunaud L, Sebbag H, Bresler L, Tortuyaux JM, Boissel P (1999) Treatment of incisional hernias by placement of an intraperitoneal prothesis: a series of 128 patients. Hernia 3:141–147
Martinez DA, Vazquez JL, Pellicer E, Aguayo JL, Morales G, Moreno-Egea A (1999) Results of expanded polytetrafluoroethylene patches in moderate and large incisional hernias. Hernia 3:149–152
Scott Roth J, Park AE, Witzke D, Mastrangelo MJ (1999) Laparoscopic incisional/ventral herniorrhaphy: A five-year experience. Hernia 3:209–214
LeBlanc KA, Booth WV, Whitaker JM, Bellanger DE (2001) Laparoscopic incisional and ventral herniorrhaphy: Our initial 100 patients. Hernia 5:41–45
Salameh JR, Sweeney JF, Graviss EA, Essien FA, Williams MD, Awad S, Itani KM, Fisher WE (2002) Laparoscopic ventral hernia repair during the learning curve. Hernia 6:182–187
Wright BE, Niskanen BD, Peterson DJ, Ney AL, Odland MD, VanCamp J, Zera RT, Rodriguez JL (2002) Laparoscopic ventral hernia repair: are there comparative advantages over traditional methods of repair? Am Surg 68:291–296
Koehler RH, Voeller G (1999) Recurrences in laparoscopic incisional hernia repairs: a personal series and review of the literature. JSLS 3:293–304
Ben-Haim M, Kuriansky J, Tal R, Zmora O, Mintz Y, Rosin D, Ayalon A, Shabtai M (2002) Pitfalls and complications with laparoscopic intraperitoneal expanded polytetrafluoroethylene patch repair of postoperative ventral hernia. Lesson from the first 100 consecutive cases. Surg Endosc 16:785–788
Chari R, Chari V, Eisenstat M, Chung R (2000) A case controlled study of laparoscopic incisional hernia repair. Surg Endosc 14:117–119
Ramshaw BJ, Esartia P, Schwab J (1999) Comparison of laparoscopic and open ventral herniorrhaphy. Am Surg 65:827–831
Heniford BT, Ramshaw BJ (2000) Laparoscopic ventral hernia repair: a report of 100 consecutive cases. Surg Endosc 190:645–650
Carbajo MA, Martín del Olmo JC, Blanco JI, Cuesta C, Toledano M, Martin F, Vaquero C, Inglada L (2003) Laparoscopic approach to incisional hernia. Surg Endosc 17:118–122
LeBlanc KA, Booth WV, Whitaker JM, Drake E, Bellanger E (2000) Laparoscopic incisional and ventral herniorrhaphy in 100 patients. Am J Surg 14:419–423
Moreno-Egea A, Aguayo JL (2002) Ambulatory laparoscopic repair of inferior Lumbar or Petit Hernia: a case report. Surg Endosc 16:1107
Moreno-Egea A, Castillo JA, Girela E, Torralba JA, Aguayo JL (2002) Outpatient laparoscopic incisional hernioplasty: our experience in 55 cases. Surg Laparosc Endosc Percutan Tech 12:171–174
Kirshtein B, Lantsberg L, Avinoach E, Bayme M, Mizrahi S (2002) Laparoscopic repair of large incisional hernias. Surg Endosc 16:1717–1719
Eitan A, Bickel A (2002) Laparoscopically assisted approach for postoperative ventral hernia repair. J Laparoendosc Adv Surg Tech A 12:309–311
Parker HH, Nottingham JM, Bynoe RP, Yost MJ (2002) Laparoscopic repair of large incisional hernias. Am Surg 68:530–533
Berger D, Bientzle M, Muller A (2002) Postoperative complications after laparoscopic incisional hernia repair. Incidence and treatment. Surg Endosc 16:1720–1723
Bageacu S, Blanc P, Breton C, Gonzales M, Porcheron J, Chabert M, Balique JG (2002) Laparoscopic repair of incisional hernia: a retrospective study of 159 patients. Surg Endosc 16:345–348
Robbins SB, Pofahl WE, Gonzalez RR (2001) Laparoscopic ventral hernia repair reduces wound complications. Am Surg 67:846–900
Szymanski J, Voitk A, Joffe J, Alvarez C, Rosenthal G (2000) Technique and early results of outpatient laparoscopic mesh onlay repair of ventral hernias. Surg Endosc 14:582–584
Kyzer S, Alis M, Aloni Y, Charuzi I (1999) Laparoscopic repair of postoperation ventral hernia: early postoperation results. Surg Endosc 13:928–931
Holzman MD, Purut CM, Reintgen K, Eubanks S, Pappas TN (1997) Laparoscopic ventral and incisional hernioplasty. Surg Endosc 11:32–35
Bencini L, Sánchez LJ, Scatizzi M, Farsi M, Boffi B, Moretti R (2003) Laparoscopic treatment of ventral hernias. Prospective evaluation. Surg Laparosc Endosc Percutan Tech 13:16–19
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Egea, D.A.M., Martinez, J.A.T., Cuenca, G.M. et al. Mortality following laparoscopic ventral hernia repair: lessons from 90 consecutive cases and bibliographical analysis. Hernia 8, 208–212 (2004). https://doi.org/10.1007/s10029-004-0214-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-004-0214-9