Abstract
Purpose
The aim of this study was to comparatively evaluate the use of a three-dimensional (3D) square-shaped plate for the treatment of mandibular angle fractures.
Materials and methods
Synthetic mandible replicas were used to evaluate the effectiveness of the 3D square plate along with three other mandibular angle plating techniques. The plating techniques consisted of: (1) a 3D miniplate (2 × 2 holes, square, 2 mm); (2) a 3D miniplate (6 × 2 holes, curved, 2 mm); (3) two miniplates (four holes, straight, 2 mm and 1.6 mm); and (4) one single miniplate (four holes, straight, 2 mm). Each group was subjected to incisal and homolateral molar region loading by a tensile materials testing machine (Monsanto Tensometer 20). Load stiffness values and peak measurements of the fracture gap distraction at the superior aspect of the mandible were measured. The mean values (±standard deviation) were derived and compared using one-way analysis of variance, with statistical significance set at p < 0.05.
Results
For homolateral molar loading, statistically significant differences existed within groups (p < 0.05). For incisal edge loading, no statistically significant differences were found for stiffness among the fixation methods tested. Gap distraction at the superior aspect of the mandible was limited for three of the groups tested.
Conclusion
Under the conditions tested, the 3D square plate system provided the most favorable mechanical behavior.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fractures of the mandibular angle are common and account for 25–35% of all mandibular fractures [1]. For decades, closed reduction has been the preferred method of treatment. With the introduction of plating techniques, the need for maxillomandibular fixation (MMF), if used at all, varies from 2 to 4 weeks [2].
Many methods of osteosynthesis for angle fractures have been described, including fixation of fragments with lag screws, reconstruction plates, compression plates, and miniplates [3–7]. Much debate exists about the use of either one or two plates for treating angle fractures. According to Gear et al. [8], the most common surgical treatment for angle fractures is the use of a single miniplate with or without MMF, with the next most common being the two-miniplate technique.
The purpose of this study was to evaluate the biomechanical behavior of the most clinically accepted methods of fixation and to compare them with two three-dimensional (3D) approaches.
Materials and methods
Synthetic mandibles from Synbone® (Malans, Switzerland) were used for the experiment. Synthetic mandibles were chosen because they are made to match human dimensions, proportions, and anatomy. They have a dense outer layer resembling cortical bone and a porous inner core that resembles cancellous bone. Because of their uniformity, they can be used to eliminate many variables associated with human cadaveric or animal mandibles.
All mandibles were prepared for the experiment by drilling a socket in each of the coronoid regions and by making the same fracture in the angle region. Both sockets and fractures were standardized for the experiment with the help of a prefabricated surgical guide.
After performing the necessary osteotomies, all plates were precontoured accordingly, such that they were evenly applied on the mandible. Reduction forceps were used to reduce the fractured sites, while all screw holes were drilled perpendicular to the mandible. All plates and screws were composed of titanium alloy (Stryker-Leibinger, Freiburg, Germany). The self-tapping screws were 2.0 mm and 1.6 mm in diameter and 7 mm in length.
Twenty mandibles were divided into four groups. All holes were filled with adequate screws. The following plating systems were used for the experiment:
-
Group 1:
3D miniplates (2 × 2 holes, square, 2 mm). These plates were placed in the upper border of the external oblique ridge and the upper buccal side of the mandible.
-
Group 2:
3D miniplates (6 × 2 holes, curved, 2 mm ) were placed in the middle of the buccal surface of the mandible.
-
Group 3:
Two-plate systems consisting of a miniplate (four holes, longitudinal, 2 mm) fixed on the upper border of the external oblique ridge and a standard (four holes, longitudinal, 1.6 mm) in the inferior border of the mandible.
-
Group 4:
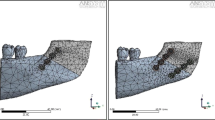
Single miniplates (four holes, longitudinal, profile height 2 mm) fixated on the upper border of the external oblique ridge (Fig. 1).
In order to study the performance of the above fixation approaches, the mandible models were divided into four subgroups of five. Therefore, each technique was tested with five independent specimens, each one used for one testing procedure only.
Two loading modes were used in this study: an incisal edge loading and a homolateral molar loading. Incisal edge loading was applied to reproduce vertical loads, while homolateral molar loading was applied to reproduce torsional forces. The latter loading simulates mastication forces during a left lateral movement of the mandible, where the left condylus stays close to its position while the right condylus starts a protrusion. The connection between the condylus and the rotation point of the protrusion can be considered as the rotation axis for this movement [9].
The mandibles were loaded through two different custom-made jigs, one for each loading mode (Fig. 2). The jigs were adapted to a tensile materials testing machine (Monsanto Tensometer 20, Dorcan, Swinton, Wiltshire, UK). For incisal edge loading, the samples were secured with a stainless steel rod passing through the sockets in the coronoid region, as described by Haug et al. [10]. The proximal fragment of the mandible was thus immobilized through the contact of the mandible condyles on the metal base of the jig and the steel rod. For the homolateral molar loading, the reconstructed side of the synthetic mandible was secured with a stainless steel rod through the coronoid region. The condyle region was permitted to rest on the jig. The activator applied vertical loads to the molar region of the distal fragment, thus resulting in torsion between the two parts of the reconstructed area of the mandible.
The behavior of the plating systems was evaluated within a 0 to 200 N range, following a 100 N preloading test, at incisal edge loading, and within a 0 to 100 N range at homolateral molar loading. Measurements of fracture gap distraction at the superior aspect of the experimental fracture were recorded before the load application and at the application of loads of 100 and 200 N on the incisal edge of the mandible by using known digital photography techniques and subsequent AutoCAD-based procedures, with an accuracy of about 0.1 mm [11].
Using raw data, load versus displacement graphs were plotted and construct stiffness values calculated using linear regression. Changes of gap distraction at the superior aspect of the experimental fracture versus load were also plotted. Mean and standard deviations of eight measurements of bending and torsional stiffness were derived from each fixation technique and compared for statistical significance by one-way analysis of variance. A p < 0.05 was considered significant. To assess the differences, each fixation technique was compared to the proposed technique (group 1).
Results
The typical load–displacement diagram for the determination of the bending stiffness of group 1 can be seen in Fig. 3. This diagram shows that for forces up to 200 N, the bending stiffness displays a linear elastic behavior. Torsional loading was limited to 100 N due to deviation from linearity of three of the fixation techniques (groups 2 and 4) above this load. There was only one plate fracture recorded during testing of the plating systems, which was in group 3.
The mean values and standard deviations of stiffness under incisal edge loading and homolateral molar loading are presented in Figs. 4 and 5. High standard deviation values were observed for bending stiffness, in contrast to the corresponding values of torsional stiffness. Possible reasons for these high standard deviations might be the misalignment of the holes at the coronoid region through which a stainless steel rod secured the mandibles in place, misalignments in osteosynthesis, or a slight slippage of the condyles on the metal base of the jig.
The results of the statistical analysis are summarized in Table 1. Group 1 presented statistically significant higher torsional stiffness compared to any of the other studied groups (p < 0.05). On the contrary, concerning bending stiffness, no statistically significant difference among the studied groups was observed (p > 0.05).
With respect to fracture gap distraction at the superior aspect of the experimental fracture, the results of the present study showed that three of the tested mandible plating techniques, groups 1, 3, and 4, demonstrated limited gap change during bending loading. This finding was expected, as these techniques comprised a plate bridging the fracture gap at the superior aspect (Fig. 6).
Discussion
The angle region is one of the most frequent sites for mandibular fractures, with direct application of miniplates as dictated by Champy et al. [12, 13] being the most commonly used fixation technique (Gear et al. [8]). Debate still exists concerning the optimal treatment of mandibular angle fractures [14, 15]. Miniplate osteosynthesis provides rigid fixation that may be easily adapted to the curvature of the bone, and requires only a simple operation. The AO/ASIF approach seems to be less preferred due to the need for an extra oral approach and increased complication rates [16, 17].
The stability of single miniplate fixation of angle fractures was challenged by several biomechanical studies based on 3D models. Kroon et al. [18] and Choi et al. [19] both observed bony gaps along the inferior fracture border, and this fracture movement was thought to contribute to subsequent complications, including infection. The use of a second plate was suggested to reduce anterior–posterior separation of the fracture line as well as lateral displacement, which is frequently observed. Until now, it has not been clarified how the placement of a second miniplate affects complication rates [20, 21].
3D miniplates are new, but are already commonly used by surgeons. A biomechanical study in sheep mandibles by Wittenberg et al. [22] showed acceptable to good results. Our goal in this study was to compare fixation with two 3D miniplates with the most clinically accepted miniplate intraoral fixation methods. For this study, we used a 3D miniplate (group 2) that was placed in the buccal aspect of the mandible and a square-shaped miniplate that was contoured so as to lie passively in the external oblique ridge region (group 1). The 3D plates can be considered a two-plate system, with two miniplates joined by interconnecting crossbars.
Only a few studies have investigated the selection of an appropriate load level to simulate in vivo biting forces, and these report only qualitative results with no data. Most studies of bite forces have been reported on healthy persons, dental prosthesis wearers, and postoperative bite forces [23]. The bite forces of healthy persons vary between 127 and 721 N depending on age, sex, and method of measurement [24]. The differences in the data on bite forces demonstrate the difficulty in measuring those forces in vivo. Ellis et al. [25] have found that bite forces in the acute postoperative period are much lower than bite forces recorded later in the postoperative period or in the non-operated population. This observation was echoed by Harada et al. [26] when assessing orthognathic surgery candidates preoperatively and postoperatively. Mastication forces have been shown to decrease dramatically after a fracture (25–66 N), with the values gradually returning to normal as healing progresses. These findings were supported by Tate et al. [27] who found molar bite forces in patients with angle fractures to be significantly less than those of controls for several weeks after surgery. Based on these studies of bite force in postoperative patients, we made the assumption that meaningful information regarding mechanical behavior would be obtained within the 200-N range for incisal loading and within the 100-N range for molar loading.
As discussed above, stiffness measurements were taken for all groups after placing an incisal or homolateral load in an attempt to reproduce vertical and torsional forces. During incisal loading, there were no statistical differences among groups. On the other hand, a significant difference in the results was observed during molar loading, with groups 1 and 3 being significantly different from the other groups (p < 0.05). In addition, group 1 showed the best mean value. Similar results were also found by Haug et al. [10]. For incisal edge loading, only minor differences were found within categories, and no differences were found between those groups representing their categories. For homolateral molar loading, statistically significant differences existed within and among categories.
From the above-described results, we can make the assumption that 3D plates can reproduce similar biomechanical scores to the traditional plating techniques. Furthermore, Champy’s investigations with the “ideal lines of osteosynthesis” in the mandible also apply to these 3D plates, as seen with group 1.
Our biomechanical study shows that it is reasonable to use 3D plates for fixation of mandibular angle fractures. In addition, the use of a square-shaped 2.0 mm 3D plate, properly contoured as described, seems to have optimal biomechanical behavior in simulated bending and torsional forces. These plates are easier to place intraorally than reconstruction or compressive fixation systems, a feature that may increase their clinical use in the future. However, this outcome should be confirmed by further clinical studies.
References
Fonseca R (2005) Oral and maxillofacial trauma (ed 3). Saunders, Philadelphia 486
Prein J, Schilli W, Hammer B et al (1991) Rigid fixation of facial fractures. In: Fonseca RJ, Walker RV (eds) Oral and maxillofacial trauma. Saunders, Philadelphia, pp 1206–1240
Choi BH, Kim KN, Kang HS (1995) Clinical and in vitro evaluation of mandibular angle fracture fixation with the two miniplate system. Oral Surg 79:692–695
Ellis E, Sinn D (1993) Treatment of mandibular angle fractures using two 2.4 mm dynamic compression plates. J Oral Maxillofac Surg 51:969–973
Ellis E (1993) Treatment of mandibular angle fractures using the AO reconstruction plate. J Oral Maxillofac Surg 51:2504
Ellis E III (1999) Treatment methods for fractures of the mandibular angle. Int J Oral Maxillofac Surg 28:243
Shetty V, Caputo A (1992) Biomechanical validity of the solitary lag screw technique for reducing mandibular angle fractures. J Oral Maxillofac Surg 50:63
Gear A, Apasova E, Schmitz J, Schubert W (2005) Treatment modalities for mandibular angle fractures. J Oral Maxillofac Surg 63:655–663
Weingärtner T, Dillmann R (1997) Simulation of jaw-movements for the musculoskeletal diagnoses. Stud Health Technolog Inform 39:401–410
Haug R, Fattahi T, Goltz MA (2001) Biomechanical evaluation of mandibular angle fracture plating techniques. J Oral Maxillofac Surg 59:1199–1210
Antoci A, Voor MJ, Seligson D et al (2004) Biomechanics of external fixation of distal extraarticular fractures. J Orthop Trauma 18:665–673
Champy M, Lodde JP, Jaeger JH et al (1976) Mandibular osteosynthesis according to the Michelet technic. II. Presentation of new material. Results. Rev Stomatol Chir Maxillofac 77:577
Champy M, Lodde JP, Jaeger JH et al (1976) Mandibular osteosynthesis according to the Michelet technic. I. Biomechanicalbases. Rev Stomatol Chir Maxillofac 77:569
Wagner WF, Neal DC, Alpert B (1979) Morbidity associated with extraoral open reduction of mandibular fractures. J Oral Surg 37:97
Chuong R, Donoff RB, Guralnick WC (1983) A retrospective analysis of 327 mandibular fractures. J Oral Maxillofac Surg 41:305
Iizuka T, Lindqvist C, Hallikainen D et al (1991) Infection after rigid internal fixation of mandibular fractures: a clinical and radiologic study. J Oral Maxillofac Surg 49:585
Potter J, Ellis E (1999) Treatment of mandibular angle fractures with a malleable noncompression miniplate. J Oral Maxillofac Surg 57:288
Kroon FH, Mathisson M, Cordey JR et al (1991) The use of miniplates in mandibular fractures. An in vitro study. J Craniomaxillofac Surg 19:199
Choi BH, Yoo JH, Kim KN et al (1995) Stability testing of a two miniplate fixation technique for mandibular angle fractures. An in vitro study. J Craniomaxillofac Surg 23:123
Ellis E, Walker L (1994) Treatment of mandibular angle fractures using two noncompression miniplates. J Oral Maxillofac Surg 52:1032
Schierle HP, Schmelzeisen R, Rahn B et al (1997) One- or two-plate fixation of mandibular angle fractures? J Craniomaxillofac Surg 25:162
Wittenberg J, Mukherjee D, Smith B, Kruse R (1997) Biomechanical evaluation of new fixation devices for mandibular angle fractures. Int J Oral Maxillofac Surg 26:68–73
Helkimo E, Carlsson GE, Helkimo M (1977) Bite force and state of dentition. Acta Odontol Scand 35:297
Fontijn-Tekamp FA, Slagter AP, van der Bilt A (2000) Biting and chewing in overdentures, full dentures, and natural dentitions. J Dent Res 79:1519
Ellis E, Throckmorton GS, Sinn DP (1996) Bite forces before and after surgical correction of mandibular prognathism. J Oral Maxillofac Surg 54:176
Harada K, Watanabe M, Ohkura K et al (2000) Measure of bite force and occlusal contact area before and after bilateral sagittal split ramus osteotomy of the mandible using a new pressure-sensitive device: a preliminary report. J Oral Maxillofac Surg 58:370
Tate GS, Ellis E, Throckmorton GS (1994) Bite forces in patients treated for mandibular angle fractures. J Oral Maxillofacial Surg 52:734
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kalfarentzos, E.F., Deligianni, D., Mitros, G. et al. Biomechanical evaluation of plating techniques for fixing mandibular angle fractures: the introduction of a new 3D plate approach. Oral Maxillofac Surg 13, 139–144 (2009). https://doi.org/10.1007/s10006-009-0163-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10006-009-0163-7