Abstract
Conduct disorder (CD) is a heterogeneous pattern of rule-breaking and aggressive symptoms. Until now it has been unclear whether valid, clinically useful symptom profiles can be defined for populations in youth at high-risk of CD. Interview-based psychiatric disorders, CD symptoms and officially recorded offences were assessed in boys from a detention facility and a forensic psychiatric hospital (N = 281; age 11.2–21.3 years). We used latent class analyses (LCA) to examine CD subtypes and their relationships with comorbid psychiatric disorders, suicidality, and criminal recidivism. LCA revealed five CD subtypes: no CD, mild aggressive CD, mild covert CD, moderate CD, and severe CD. The severe and, to a lesser degree, the moderate CD subtype were related to comorbid attention deficit hyperactivity disorder, substance use disorder, affective disorder, and suicidality. Time to violent criminal re-offending was predicted by severe CD (OR 5.98, CI 2.5–13.80) and moderate CD (OR 4.18, CI 1.89–9.21), but not by any other CD subtype in multivariate Cox regressions (controlling for age, low socioeconomic status and foreign nationality). These results confirm the existence of different CD symptom profiles in a high-risk group. Additional variable-oriented analyses with CD symptom count and aggressive/rule-breaking CD-dimensions further supported a dimensional view and a dose–response relationship of CD and criminal recidivism. Classifying high-risk young people according to the number of aggressive and rule-breaking CD symptoms is of major clinical importance and may provide information about risk of violent recidivism.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Conduct disorder (CD) is a frequent psychiatric disorder that goes along with serious social, emotional, and academic impairments in children and adolescents [1] and increases the risk of later criminality [2]. The presence of CD in childhood and adolescence was also found to be related to neurobiological impairment (e.g., [3]). However, patterns of CD symptoms can vary widely. According to the 5th edition of the Diagnostic and statistical manual of mental disorders (DSM-5), the 15 CD symptoms fall into four main categories: (A) aggression towards people and animals (1. frequent threatening or bullying behaviour, 2. initiation of physical fights, 3. use of weapons, 4. hurting of people, 5. hurting of animals, 6. robbery, and 7. sexual coercion); (B) destruction of property (8. fire setting and 9. property damage); (C) deceit or theft (10. burglary, 11. frequent lying, and 12. theft); (D) serious rule violations (13. staying out late, 14. running away from home, and 15. frequent truancy). DSM-IV, DSM-5, and the 10th and 11th versions of the International Classification of Diseases (ICD-10 and ICD-11) only require 3 out of 15 symptoms to be present for a diagnosis of CD; hence there are 32,647 valid symptom combinations for CD [4]. DSM-5 and ICD-10 and -11 allow subtyping of CD by severity (mild; moderate; severe) but neither manual provides clear definitions of these diagnostic sub-categories.
A number of studies have addressed the symptom heterogeneity of CD through factor analysis and reported that there are two or more factors underlying CD (e.g., [5,6,7]). Although there are minor differences in the number of factors identified and the variance explained, overall these studies suggest that young people should be classified using a multidimensional approach, based on both physical aggression and rule-breaking/covert symptoms. These two dimensions were typically found to be correlated (r = 0.4–0.6, [8]), but were also found to be distinguishable with respect to aetiology, course and comorbidity [8].
Other studies have used person-centred methods such as latent class analysis (LCA) to reveal specific CD subtypes in community samples and they have produced strikingly similar findings [9,10,11]: the majority of young people do not have CD (60.7–89.8%), a small subgroup shows severe and pervasive symptoms (3.1–4.3%), a small subgroup shows only physical aggression symptoms (1.5–2.3%), and one to three subtypes show only covert symptoms (13.9–32.2%). Compared with the no-CD subtype, the other subtypes are at increased risk of developing psychiatric disorders [11] and subsequent self-reported antisocial behaviours (e.g., selling drugs, gang membership, weapon use, physical assault, and police contact [9, 10]). All three studies [9,10,11] suggest there is a dose–response relationship, with more severe forms of CD increasing the probability of developing psychiatric disorders and showing criminal behaviour.
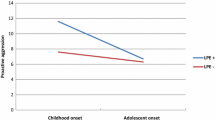
The broad evidence for the validity of the CD diagnosis in children and adolescents is based on large number of studies from community and psychiatry samples (e.g., [1]). A smaller number of studies have examined CD and its subtypes in forensic youth settings (psychiatric care settings of juvenile justice involved youth) and partly confirmed that CD subtypes based on the time of onset (childhood or adolescence) and the additional CD specifier of limited prosocial emotions (LPE) are valid and useful diagnostic categories (e.g., [12,13,14]). However, no previous study has investigated CD symptom profiles in high-risk young people in forensic settings. Identifying CD subtypes in this group would enhance understanding of specific forms of aggression and delinquent behaviour in young people and improve psychiatric assessments in forensic settings and thus contribute to prevention of criminality. Developing and applying preventive interventions is an important challenge for child and adolescent psychiatry [15].
To enhance the understanding of CD in forensic youth, we performed data-driven, person-centered analyses in a sample of boys from two forensic facilities to determine whether clinically meaningful subtypes (e.g. a no CD subtype and specific aggressive, rule-breaking, and severe CD subtypes) would emerge. We tested associations between subtypes and comorbid psychiatric disorders and suicidality. We analysed CD subtypes as predictors of criminal recidivism. Based on previous findings in community samples of young people, we expected to identify a severe CD subtype and a no/mild CD subtype as well as two moderate CD subtypes with predominantly aggressive or covert/rule-breaking symptoms. We assumed that boys with severe CD, predominantly aggressive CD or covert CD would show higher rates of comorbid disorders and suicidality than boys with no/mild CD. We assumed that boys with severe CD would have the highest risk of violent recidivism whilst controlling for effects of age, low socio-economic status (SES), and foreign nationality. An alternative approach to address severity of CD is a score based on the number of CD symptoms. Based on previous findings on CD symptoms as a predictors of antisocial personality disorders [16], we further performed variable-oriented analyses using a CD symptom count and aggressive/rule-breaking CD dimensions as predictors of psychiatric comorbidity and criminal recidivism.
Method
Participants and procedures
The participants were drawn from two facilities, (1) the Zurich Juvenile Detention Centre and (2) the Child and Adolescent Forensic Service Centre of the University Hospital of Psychiatry Zurich, Switzerland. Because of the small number of females available, we only considered male adolescents in the present study. All study participants were informed about the general purpose of the study (investigation of the relationship between psychopathology and criminal behaviour), but they were blind to the specific aims. The minimum age of criminal responsibility in Switzerland is 10 years (it is higher in some other European countries).
Detained group
Male adolescents were recruited from the Zurich Juvenile Detention Centre from September 2010 to November 2012. The study procedure is described in more detail elsewhere [17]. Exclusion criteria were insufficient knowledge of the German language, significant medical conditions (e.g., acute state of human immunodeficiency virus, hepatitis or other infectious diseases), neurological disorders (e.g., epilepsy), mental retardation, and current psychotic symptoms. Out of a total of 226 juveniles, 4 (1.7%) refused to participate and 6 (2.7%) were excluded as they were released before data collection took place. Thirty-one of the remaining 216 adolescents (14.4%) were excluded because they had insufficient knowledge of the German language and 9 (4.2%) due to mental retardation or the presence of psychotic symptoms. A further 52 (24.1%) juveniles were excluded because of missing or incomplete data on psychopathology (18, 8.3%) or criminal recidivism (for the youth living outside of the Canton of Zurich, see below; n = 34, 15.7%). The final prisoner group consisted of 122 boys aged 13.9–19.2 years (M = 16.8 years, SD = 1.1 years) who had been detained for between 1 and 754 days (M = 33.3, SD = 95.9).
Forensic outpatient group
From September 2011 to December 2015 data were collected from youth referred by juvenile justice authorities for comprehensive forensic assessment by the Child and Adolescent Forensic Outpatient Unit of the University Hospital of Psychiatry, Zurich (n = 167). Exclusion criteria were insufficient knowledge of the German language, mental retardation, and current psychotic symptoms. One adolescent (0.6%) refused to participate in the study. Four of the remaining 166 boys (2.4%) were excluded due to insufficient knowledge of German or mental retardation. Another 3 (1.8%) were excluded because they were detained during the assessment period and were thus considered part of the prisoner sample. The final forensic outpatient group consisted of 159 boys aged 11.2–21.5 years (M = 16.5, SD = 1.7).
Ethical considerations
All participants gave written informed consent to participation. Ethical approval was granted by the Swiss Federal Institute of Health (for the detention centre sample) and by the ethics committee of the Canton of Zurich (for the outpatient forensic sample).
Measures
Psychiatric disorders and suicidality
Conduct symptoms and disorders as well as comorbid affective disorders, anxiety disorders, attention-deficit-hyperactivity disorder (ADHD), substance use disorders, and current suicidality were assessed using the Mini-International Neuropsychiatric Interview for Children and Adolescents (MINI-KID), a structured clinical diagnostic interview designed to assess the presence of psychiatric disorders in children and adolescents [18]. Diagnoses were based on an algorithm that is appropriate for symptom count, age, duration, and impairment according to DSM-IV criteria. All diagnostic interviews were performed by experienced and approved psychiatrists or clinical psychologists. The MINI-KID has been shown to have good reliability and validity when compared with the Schedule for Affective Disorders and Schizophrenia for School Aged Children—Present and Lifetime Version [18] and was found to be an accurate method of assessing psychiatric disorders in other samples of boys [17, 19]. CD symptom count and CD dimension were based on z-transformed sum scores for MINI-KID CD items (0 = not present; 1 = present). In line with previous research [8, 20] the aggressive CD dimension consisted of seven CD items (threat, fight, weapon use, hurting people, hurting animals, robbery, and sexual coercion) whereas the covert/rule-breaking CD dimension consisted of eight items (fire setting, property damage, burglary, lying, theft, staying out late, running away, and truancy).
Demographic information
Age, nationality and reason for current detention/assessment (according to the Swiss penal code) were coded directly from the case files. SES coding was based on the occupations of maternal and paternal caregivers, which were coded according to ISCO-08 guidelines [21] ranging from 1 (management position) to 9 (unskilled worker); unemployed caregivers were coded 10. Participants were classified as having low SES when the SES of both caregivers was coded as 9 or 10 or the SES of one caregiver was missing and the SES of the other caregiver was coded as 9 or 10. Reason for detention/assessment was classified as violent crime (e.g., sexual coercion, manslaughter, robbery), property crime (e.g. theft, defraud), drug-related crime, or other crime.
Criminal register data
Information on criminal history and adolescent and adult recidivism were drawn from the crime registry of the canton of Zurich. This computerised database contains all past and current transactions from all prosecution institutions and prisons in the canton of Zurich including information on the date of charges, types of offences, dates of convictions or penalty orders, and the beginnings and endings of detentions or incarcerations. As a limitation, the database does not contain sentence or court information. We used the information on new charges to measure re-offending. All adolescents from the detention sample had been released from prison and were followed for 365 days. All youth from the forensic outpatient sample were followed for 365 days after the initial assessment. As well as counting new criminal offences we also counted new violent offences (defined as new charges or convictions for crimes that involved physical violence e.g., robbery, manslaughter, or sexual assault) separately.
Statistical analysis
To investigate CD subtypes we entered responses to the 15 MINI-KID items on CD to LCA in Mplus 7.31 [22]. LCA is a form of categorical data analysis based on the hypothesis that symptom profiles of individual participants can be assigned to a number of mutually exclusive classes. We started by fitting a one-class model and increased the number of classes one at a time, setting 100 random starting values. One- to six-class models were compared with respect to the Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), adjusted Bayesian Information Criterion (aBIC), and entropy to determine the number of classes that represented the data best [23]. We also used the Lo–Mendell–Rubin Likelihood Ratio-Test (LMR LRT) and the bootstrapped parametric Likelihood Ratio Test (BLRT); both these tests compare a model with a certain number of classes (K) to a model with K − 1 classes. It should be noted, however, that when choosing a latent class model, one should consider how reasonable a model is with respect to the research questions being investigated and the generalisability of the model to other populations [23] as well as purely statistical measures.
Logistic regressions (LR) were performed to analyse the relationships between CD subtypes and comorbid affective disorders, anxiety disorders, ADHD, substance use disorders, and suicidality. Cox regressions were used to examine CD subtypes and time to criminal and/or violent recidivism during the first 365 days after release (with and without controlling for effects of age, foreign nationality, and low SES). The no CD subtype and severe CD subtype (see below) were chosen as reference categories in different regression analyses. The proportional hazard assumption was tested for predictors and covariates. The explained variance was estimated with Nagelkerke’s R2 in LR.
Results
Descriptive findings
The combined detention and forensic outpatient sample consisted of 281 boys aged between 11.2 and 21.3 years (M = 16.7 years, SD = 1.5 years), of whom 115 (40.9%) were of foreign nationality and 69 (24.6%) were of low SES. Over half the sample (n = 164, 58.4%) met the DSM-IV criteria for CD. The aggressive and the covert/rule-breaking CD dimensions were moderately correlated (r = 0.61, p < 0.001).
There was no mean difference in the age of the detained group (M = 6.8 years, SD = 1.1) and outpatient group (M = 16.5 years, SD = 16.5; t(272) = 1.91, p = 0.059). Foreign nationality was more frequent in the detained group (n = 58, 47.5%) than the outpatient group (n = 57, 35.8%; χ2(1) = 3.90, p = 0.048). The frequency of low SES was similar in the two groups (prisoners: n = 85, 69.7%, outpatients: n = 79, 49.7%; χ2(1) = 2.86, p = 0.091). Further descriptive findings on reason for detention/assessment, presence of psychiatric disorders, and current suicidality of the outpatient and the detained group are presented in Table 1. Compared with the forensic outpatient group the detained group were more likely to have been detained in relation to violent other crimes, more likely to have psychiatric disorders, and were more frequently charged or convicted of further offences and violent offences following release.
LCA based on CD items
Table S1 (available Online) displays the comparisons of LCA models with one to six subtypes. Although values of the AIC and the BIC were lowest for the models with six and three subtypes, respectively, the five-subtype model had the smallest aBIC. The likelihood ratio tests (LMR, LRT, and BLRT) indicated that the three-subtype solution fit the data significantly better than the two-subtype solution and that the five-subtype solution fit the data significantly better than the four-type solution. The five-subtype model yielded the highest entropy value of the models compared and produced subtypes that could be interpreted reasonably well. Thus, further analyses were based on the assignments to the five-subtype model, which consisted of a no-CD subtype, a mild covert CD subtype, a mild aggressive CD subtype, a moderate CD subtype and a severe CD subtype (Fig. 1). Descriptive statistics for the five CD subtypes are shown in Table 2. DSM-IV CD-criteria were met in 3.3% of the no-CD cases and in 73.4–100% of cases of the other four CD subtypes.
Associations of CD subtypes and dimensions with comorbid disorders
Associations of CD subtypes with comorbid disorders and suicidality are shown in Table 3. Compared with the no-CD subtype, (1) the odds of the presence of comorbid affective disorders, anxiety disorders, substance use disorder, ADHD, and suicidality were higher in the severe CD subtype; (2) the odds of affective disorders, substance use disorders, and ADHD were higher in the moderate CD subtype; (3) the odds of substance use and ADHD were higher in the mild covert CD subtype; (4) only the odds of ADHD were increased in the mild aggressive CD subtype. We also carried out analyses of a reduced sample excluding all no-CD cases, with the severe CD subtype as the reference category (Supplemental Table S2). The odds of affective disorders and ADHD were lower in the mild covert, mild aggressive, and moderate CD subtypes than in the severe CD subtype. Furthermore, the odds of anxiety disorders and substance use disorders were lower in the moderate CD subtype than the severe CD subtype. CD symptom count was related to all comorbid disorders and suicidality. The aggressive CD dimension was related to ADHD only. The rule-breaking CD dimension was related to affective disorders, substance use and ADHD.
Prediction of time to criminal and violent recidivism
Frequencies and χ2-statistics for criminal and violent recidivism in the CD subtypes are presented in Table 2. Univariate and multivariate Cox regressions with CD subtypes as predictors and times to criminal and violent recidivism as outcomes are presented in Table 4. Both the severe CD subtype and the moderate CD subtype positively predicted time to criminal recidivism and time to violent recidivism with the no-CD subtype as the reference group. These relationships remained when controlling for age, foreign nationality, and low SES (multivariate model). Of the remaining CD subtypes, only the mild aggressive subtype positively predicted recidivism (time to criminal recidivism but not time to violent recidivism). CD symptom count and the aggressive CD dimension but not the rule-breaking CD dimension predicted both time to criminal recidivism and time to violent recidivism.
Additional analyses were performed in a subsample by excluding the no-CD cases and using the severe CD subtype as reference category (Supplemental Tables S2 and S3). These additional analyses show significantly decreased OR of mild covert, mild aggressive, and moderate CD subtypes compared to the severe CD subtype for predicting comorbid psychopathology and criminal recidivism.
Discussion
This study of CD and its subtypes in a sample of boys detained or referred for forensic assessment in which psychopathology was prevalent confirms and expands previous findings from clinical and community samples with low symptom rates [5, 8,9,10,11]. The replication of findings from community samples is important because the detention situation and criminal proceedings were found to influence the information on psychopathology [19, 24]: Some youth were repressing and denying behavioural problems while fearing legal consequences, and others reported higher levels of psychopathology due to increased stress from incarceration. A number of previous studies have confirmed the validity of CD and its subtypes as defined in DSM-IV/-5 and ICD-10/-11 such as age of onset related subtypes and/or the presence of LPE (e.g., [13, 25,26,27]) in detained and/or delinquent youth but none of these studies specifically addressed symptom profiles in forensic youth so far.
Five CD subtypes were identified empirically. Approximately 66% of the sample belonged to the four pathological subtypes (severe, moderate, mild aggressive and mild covert CD) and the majority of these participants met DSM-IV criteria for CD. Approximately 33% of the sample belonged to the non-pathological subtype (no CD subtype) and the majority of these participants did not meet DSM-IV criteria for CD. The absence of CD in boys from forensic youth settings may seem astonishing but was in line with our hypotheses. There are a number of possible explanations. First, some boys carry out isolated acts of delinquency or only display delinquency during adolescence; their behaviour is not considered psychopathological [28]. Second, adolescents may have been charged or convicted for behaviours not captured by DSM-IV CD-criteria such as non-forced child sexual abuse or drug dealing [29]. Third, CD classification was based solely on interview information and some boys may have been reluctant to admit to additional criminal behaviour due to fear of the legal consequences.
LCA yielded two subtypes representing milder forms of CD: A mild aggressive subtype associated with verbal and physical aggression towards people and a mild covert subtype associated with theft, property damage, and rule-breaking were identified. These two subtypes align with the CD-dimensions described previously [5, 8, 30]. Our findings are in line with a previously developed model of CD that distinguished physically aggressive, non-aggressive, and mixed forms; they are also consistent with a developmental model of CD with overt vs. covert behaviours as starting points for delinquent courses [31]. Although boys with mild forms of CD had lower rates of comorbidity and were at less risk of committing offences they still require psychiatric treatment. Young people with these milder, more circumscribed forms of CD may respond better to specific CD treatment programmes [32] than youth with severe forms of CD and comorbid disorders.
The severe and moderate CD subtypes encompassed a high number of CD symptoms and rather non-specific symptom profiles. The severe CD subtype was positively related to a variety of additional mental health problems. Compared with no-CD cases, severe CD cases were 28 times more likely to have a substance use disorder, 17 more likely to have ADHD and 9 more likely to have an affective disorder. Furthermore, severe CD cases were also more likely to be affected by affective disorders and ADHD than cases of the other pathological subtypes. Severe CD may be associated with a cascade of associated life stressors, such as impaired family relations, school problems and/or imprisonment, which increase the likelihood of comorbid affective and substance-related disorders [33]. ADHD has consistently been reported to be a major risk factor for juvenile delinquency and to be highly comorbid with CD (e.g., [29]). These findings were further supported by a dimensional perspective: CD symptom count was found related to all categories of comorbidity and to suicidality. Aggressive and rule-breaking symptoms were associated with specific comorbid disorders only. Mental health services and suicide prevention programmes should, therefore, be targeted at boys with an accumulation of CD symptoms. Given that 86% of the severe CD cases were from the prisoner group it is crucial to provide access to mental health services in prisons and other criminal detention facilities. Treatment of young offenders with CD should take into account the high comorbidity rates with other disorders.
Our findings based on LCA and CD symptom count variables suggest a dose–response relationship between CD and criminality, with more serious forms of CD being associated with higher probabilities of future criminal and violent behaviour [9,10,11]. The severe and moderate CD subtypes were found to be at increased risk of criminal or violent recidivism compared with the no-CD subtype. When only the pathological subtypes were considered, the severe and moderate subtypes had higher odds of recidivism than the mild covert and mild aggressive subtypes (Supplemental Table S3). This finding suggests that there are meaningful differences between boys who meet diagnostic criteria for CD and that they should be taken into account in forensic samples. A diagnosis of severe/moderate CD seems a particularly good marker for risk of persistent criminality, including violent criminality. Boys with a high number of CD symptoms appear to be at the highest risk of later antisocial personality disorders [16, 20, 34]. We further found the number of aggressive symptoms of CD but not the number of rule-breaking symptoms related to criminal and violent re-offences. This finding supports the assumption that the presence of overt and physical forms of aggression represents a somewhat more severe form of CD with an unfavourable prognosis (e.g., [35]). Several risk assessment instruments are currently available for estimating the probability of future offending in young people but none of these instruments directly rely on the number of CD symptoms. Further studies may examine if interview-based CD-severity and/or weighted CD-item scores are useful as additional risk factors to further improve the validity of current risk assessment instruments.
This study has several strengths: psychopathology was assessed through a gold-standard clinical diagnostic interview and criminal recidivism was coded from official data. Our results converge with and expand on existing findings. Furthermore, our findings extend understanding of CD from a person-centred perspective. The limitations of the study include the restricted range of the sample, which was recruited from just two forensic institutions and consisted mostly of Caucasian boys living in the canton of Zurich, Switzerland. The cultural and gender specificity of the sample limits the generalisability of the findings to other juvenile justice samples. The age of the current sample ranged between 11.2 and 20.3 years and this wide age span may have influenced the current findings. Some CD symptoms are more prevalent in younger boys whereas others are more prevalent in older boys. Because sufficient knowledge of the German language was an inclusion criterion, our analyses did not include any non-German speakers. Psychopathology was assessed solely through interviews with participants; no third-party information, such as parent or teacher reports, was available. Data on criminal recidivism only included offences with which the participant had been charged, so un-registered (dark-field) offences were not included.
Conclusion
Specific CD subtypes should be taken into account in further research into the aetiology, course and outcomes of CD as well as evaluations of interventions for high-risk young people. We strongly encourage a detailed assessment of CD in forensic and clinical practice by assessing and reporting symptom severity and specific CD profiles with aggressive or rule-breaking symptom accumulation. In accordance with previous research from community/clinical studies [8,9,10,11], future revisions of CD classification systems should consider CD subtypes defined in terms of aggressive and covert or rule-breaking behaviours. The current findings further support a dimensional view of conduct problems based on chronic or temporary impairments in the domain of social cognition or mentalizing inspired by the NIMH Research Domain Criteria (RDoC) [36]. CD treatment in high-risk boys must be comprehensive and tailored to individual risk and need profiles. There is a need for more specific treatment programmes for forensic young people.
References
Frick PJ (2016) Current research on conduct disorders in children and adolescents. S Afr J Psychol 46(2):160–174. https://doi.org/10.1177/0081246316628455
Erskine HE, Norman RE, Ferrari AJ, Chan GC, Copeland WE, Whiteford HA, Scott JG (2016) Long-term outcomes of attention-deficit/hyperactivity disorder and conduct disorder: a systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry 55(10):841–850. https://doi.org/10.1016/j.jaac.2016.06.016
Blair RJ, Leibenluft E, Pine DS (2015) Conduct disorder and callous-unemotional traits in youth. N Engl J Med 372(8):784. https://doi.org/10.1056/NEJMc1415936
Lindhiem O, Bennett CB, Hipwell AE, Pardini DA (2015) Beyond symptom counts for diagnosing oppositional defiant disorder and conduct disorder? J Abnorm Child Psychol 43(7):1379–1387. https://doi.org/10.1007/s10802-015-0007-x
Burt SA, Donnellan MB, Iacono WG, McGue M (2011) Age-of-onset or behavioral sub-types? A prospective comparison of two approaches to characterizing the heterogeneity within antisocial behavior. J Abnorm Child Psychol 39(5):633–644. https://doi.org/10.1007/s10802-011-9491-9
Frick PJ, Lahey BB, Loeber R, Tannenbaum L, Van Horn Y, Christ MAG, Hart EA, Hanson K (1993) Oppositional defiant disorder and conduct disorder: a meta-analytic review of factor analyses and cross-validation in a clinic sample. Clin Psychol Rev 13(4):319–340. https://doi.org/10.1016/0272-7358(93)90016-F
Tackett JL, Krueger RF, Iacono WG, McGue M (2005) Symptom-based subfactors of DSM-defined conduct disorder: evidence for etiologic distinctions. J Abnorm Psychol 114(3):483. https://doi.org/10.1037/0021-843X.114.3.483
Burt SA (2012) How do we optimally conceptualize the heterogeneity within antisocial behavior? An argument for aggressive versus non-aggressive behavioral dimensions. Clin Psychol Rev 32(4):263–279. https://doi.org/10.1016/j.cpr.2012.02.006
Breslau J, Saito N, Tancredi DJ, Nock M, Gilman SE (2012) Classes of conduct disorder symptoms and their life course correlates in a US national sample. Psychol Med 42(5):1081–1089. https://doi.org/10.1017/S003329171100198X
Lacourse E, Baillargeon R, Dupere V, Vitaro F, Romano E, Tremblay R (2010) Two-year predictive validity of conduct disorder subtypes in early adolescence: a latent class analysis of a Canadian longitudinal sample. J Child Psychol Psychiatry 51(12):1386–1394. https://doi.org/10.1111/j.1469-7610.2010.02291.x
Nock MK, Kazdin AE, Hiripi E, Kessler RC (2006) Prevalence, subtypes, and correlates of DSM-IV conduct disorder in the National Comorbidity Survey Replication. Psychol Med 36(5):699–710. https://doi.org/10.1017/S0033291706007082
Colins OF (2016) The clinical usefulness of the DSM-5 specifier for conduct disorder outside of a research context. Law Hum Behav 40(3):310–318. https://doi.org/10.1037/lhb0000173
Colins OF, Vermeiren RR (2013) The usefulness of DSM-IV and DSM-5 conduct disorder subtyping in detained adolescents. J Nerv Ment Dis 201(9):736–743. https://doi.org/10.1097/NMD.0b013e3182a20e94
Pechorro P, Jiménez L, Hidalgo V, Nunes C (2015) The DSM-5 Limited Prosocial Emotions subtype of Conduct Disorder in incarcerated male and female juvenile delinquents. Int J Law Psychiatry 39:77–82. https://doi.org/10.1016/j.ijlp.2015.01.024
Aebi M, Giger J, Plattner B, Metzke CW, Steinhausen H-C (2014) Problem coping skills, psychosocial adversities and mental health problems in children and adolescents as predictors of criminal outcomes in young adulthood. Eur Child Adolesc Psychiatry 23(5):283–293. https://doi.org/10.1007/s00787-013-0458-y
Lahey BB, Loeber R, Burke JD, Applegate B (2005) Predicting future antisocial personality disorder in males from a clinical assessment in childhood. J Consult Clin Psychol 73(3):389–399. https://doi.org/10.1037/0022-006X.73.3.389
Aebi M, Barra S, Bessler C, Steinhausen HC, Walitza S, Plattner B (2016) Oppositional defiant disorder dimensions and subtypes among detained male adolescent offenders. J Child Psychol Psychiatry 57(6):729–736. https://doi.org/10.1111/jcpp.12473
Sheehan DV, Sheehan KH, Shytle D, Janavs J, Bannon Y, Rogers JE, Milo KM, Stock SL, Wilkinson B (2010) Reliability and validity of the mini international neuropsychiatric interview for children and adolescents (MINI-KID). J Clin Psychiatry 71(3):313–326. https://doi.org/10.4088/JCP.09m05305whi
Plattner B, Kraemer HC, Williams RP, Bauer SM, Kindler J, Feucht M, Friedrich MH, Steiner H (2007) Suicidality, psychopathology, and gender in incarcerated adolescents in Austria. J Clin Psychiatry 68(10):1593–1600. https://doi.org/10.4088/JCP.v68n1019
Le Corff Y, Toupin J (2014) Overt versus covert conduct disorder symptoms and the prospective prediction of antisocial personality disorder. J Pers Disord 28(6):864–872. https://doi.org/10.1521/pedi_2012_26_074
International Labour Organisation (2008) International Standard Classification Of Occupations (ISCO). http://www.ilo.org/public/english/bureau/stat/isco/isco08/. Accessed 10 Aug 2017
Muthen B, Muthen L (2012) Mplus user’s guide, 7th edn. Muthén & Muthén, Los Angeles
Nylund KL, Asparouhov T, Muthén B (2007) Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct Equ Model 14(4):535–569. https://doi.org/10.1080/10705510701575396
Imbach D, Aebi M, Metzke CW, Bessler C, Steinhausen HC (2013) Internalizing and externalizing problems, depression, and self-esteem in non-detained male juvenile offenders. Child Adolesc Psychiatry Ment Health 7(1):7
Fairchild G, van Goozen SH, Calder AJ, Goodyer IM (2013) Research review: evaluating and reformulating the developmental taxonomic theory of antisocial behaviour. J Child Psychol Psychiatry 54(9):924–940. https://doi.org/10.1111/jcpp.12102
Jambroes T, Jansen LM, Vermeiren RR, Doreleijers TA, Colins OF, Popma A (2016) The clinical usefulness of the new LPE specifier for subtyping adolescents with conduct disorder in the DSM 5. Eur Child Adolesc Psychiatry 25(8):891–902. https://doi.org/10.1007/s00787-015-0812-3
Kahn RE, Frick PJ, Youngstrom E, Findling RL, Youngstrom JK (2012) The effects of including a callous-unemotional specifier for the diagnosis of conduct disorder. J Child Psychol Psychiatry 53(3):271–282. https://doi.org/10.1111/j.1469-7610.2011.02463.x
Moffitt TE (1993) Adolescence-limited and life-course-persistent antisocial behavior: a developmental taxonomy. Psychol Rev 100(4):674–701
Vermeiren R, Jespers I, Moffitt T (2006) Mental health problems in juvenile justice populations. Child Adolesc Psychiatr Clin N Am 15(2):333–351. https://doi.org/10.1016/j.chc.2005.11.008
Burt SA (2009) Are there meaningful etiological differences within antisocial behavior? Results of a meta-analysis. Clin Psychol Rev 29(2):163–178. https://doi.org/10.1016/j.cpr.2008.12.004
Loeber R, Wung P, Keenan K, Giroux B, Stouthamer Loeber M, Van Kammen WB (1993) Developmental pathways in disruptive child behavior. Dev Psychopathol 5:103–133. https://doi.org/10.1017/S0954579400004296
Sawyer AM, Borduin CM, Dopp AR (2015) Long-term effects of prevention and treatment on youth antisocial behavior: a meta-analysis. Clin Psychol Rev 42:130–144. https://doi.org/10.1016/j.cpr.2015.06.009
Odgers CL, Caspi A, Broadbent JM, Dickson N, Hancox RJ, Harrington H, Poulton R, Sears MR, Thomson WM, Moffitt TE (2007) Prediction of differential adult health burden by conduct problem subtypes in males. Arch Gen Psychiatry 64(4):476–484. https://doi.org/10.1001/archpsyc.64.4.476
Washburn JJ, Romero EG, Welty LJ, Abram KM, Teplin LA, McClelland GM, Paskar LD (2007) Development of antisocial personality disorder in detained youths: the predictive value of mental disorders. J Consult Clin Psychol 75(2):221–231. https://doi.org/10.1037/0022-006X.75.2.221
Nagin D, Tremblay RE (1999) Trajectories of boys’ physical aggression, opposition, and hyperactivity on the path to physically violent and nonviolent juvenile delinquency. Child Dev 70(5):1181–1196
Fonagy P, Luyten P (2018) Conduct problems in youth and the RDoC approach: a developmental, evolutionary-based view. Clin Psychol Rev 64:57–76. https://doi.org/10.1016/j.cpr.2017.08.010
Acknowledgements
We thank Metin Aysel, MD, Silke Nessbach, MSc, Hellvig Spinka, MD, and Madleina Manetsch, MD, who helped with data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. Aebi and C. Bessler received in the last 5 years royalties from Hogrefe. Their work was supported in the last 5 years by the Swiss Federal Institute of Justice and the Juvenile Justice Authorities of the Canton Zurich. S. Walitza has received in the last 5 years royalties from Thieme Hogrefe, Kohlhammer, Springer, Beltz. S. Walitza has received lecture honoraria from Opopharma in the last 5 years. Her work was supported in the last 5 years by the Swiss National Science Foundation (SNF), diff. EU FP7s, HSM Hochspezialisierte Medizin of the Kanton Zurich, Switzerland, Bfarm Germany, ZInEP, Hartmann Müller Stiftung, Olga Mayenfisch, Gertrud Thalmann Fonds. Outside professional activities and interests are declared under the link of the University of Zurich http://www.uzh.ch/prof/ssl-dir/interessenbindungen/client/web/.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Aebi, M., Barra, S., Bessler, C. et al. The validity of conduct disorder symptom profiles in high-risk male youth. Eur Child Adolesc Psychiatry 28, 1537–1546 (2019). https://doi.org/10.1007/s00787-019-01339-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-019-01339-z