Abstract
Deficits in motor and imitation abilities are a core finding in autism spectrum disorders (ASD), but impaired motor functions are also found in attention deficit/hyperactivity disorder (ADHD). Given recent theorising about potential aetiological overlap between the two disorders, the present study aimed to assess difficulties in motor performance and imitation of facial movements and meaningless gestures in a sample of 24 ADHD patients, 22 patients with ASD, and 20 typically developing children, matched for age (6–13 years) and similar in IQ (>80). Furthermore, we explored the impact of comorbid ADHD symptoms on motor and imitation performance in the ASD sample and the interrelationships between the two groups of variables in the clinical groups separately. The results show motor dysfunction was common to both disorders, but imitation deficits were specific to ASD. Together with the pattern of interrelated motor and imitation abilities, which we found exclusively in the ASD group, our findings suggest complex phenotypic, and possibly aetiological, relationships between the two neurodevelopmental conditions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The recently published DSM-5 [1] has imposed major changes on the classification of child and adolescent psychiatric disorders, including the classification of attention deficit/hyperactivity disorder (ADHD) and autism spectrum disorders (ASD) as “neurodevelopmental disorders”, alongside other specific disorders.
This new classificatory convention was based on converging clinical [2, 3], familial [4], and genetic [5, 6] evidence that has suggested not only phenomenological, but also aetiological, overlap between the two disorders [7]. Indeed, while ADHD is one of the most frequent psychiatric conditions in childhood and adolescence (5.29 % worldwide prevalence of ADHD according to [8] and a comparatively infrequent 1–2.65 % prevalence of ASD [9–11]), there is substantial comorbidity of ASD and ADHD symptoms, varying between 30 and 80 % of cases in clinical assessments [7]. The inconsistent rates of comorbidity are probably due to different thresholds in establishing diagnostic criteria for an additional ADHD diagnosis, since symptoms of (social) inattention, fidgety behaviour, and irritability can also be intrinsic to the autistic phenotype. However, studies using factor analysis or modelling the classification of subjects according to typical questions used to detect symptomatology have previously revealed a good differentiation between the two clusters of symptoms [12, 13].
Although the clinical, familial, and genetic evidence is strongly suggestive of an aetiological overlap, examination of specific functions that may be aetiologically relevant reveals a more complicated pattern. Firstly, increased intra-subject variability (ISV) of performance, measured typically as an increase in the intra-subject standard deviation of reaction times seems to be a core abnormality of ADHD [14, 15] and a promising endophenotype of the disorder [16]. However, there is early evidence that increased ISV is not associated with ASD unless patients also suffer from ADHD [17]. Secondly, although executive dysfunctions appear to be present in both ASD and in ADHD [7], the validity of specific and differential profiles of deficits for each disorder is still a matter of debate [18–20]. Thirdly, deficits in Theory of Mind (e.g. emotion recognition, understanding of others’ minds) and weak central coherence are discussed as being specific to ASD, but have rarely been studied in ADHD [7]. Moreover, methodological problems due to the complexity of the ToM concept, a lack of a consensual definition of its basic components [21], and the potential influence of executive abilities on the development of ToM in young individuals with ASD [22–24] raise doubt about its validity as a specific marker of ASD.
Among the putative mechanisms for the development of social cognition, imitation abilities in particular have been intensively studied in ASD and found to be impaired [25] or at least delayed in their development [26]. The nature of the imitation deficits and their contribution to early social skills, however, is still controversial, mostly due to the wide range of methods and conceptual approaches that have been employed to study imitation abilities in autistic persons, hampering direct comparison between studies [27, 28]. Whatever the reason for imitation problems in ASD might be, the ability of “copying behaviour” implies a genuine motor connotation, that is reproducing any type of “action”, and has been mainly explored in tasks exploring imitation of action on objects, gestural skills or facial expressions [25, 27]. This implicit link between imitation and motor/gestural abilities is remarkable from several points of view. Firstly, the mirror neuron system (MNS) theory postulates a motor substrate for the development of social behaviour including imitative behaviour as well as understanding of others’ minds, which could be impaired in ASD [29]. While the role of mirror neurons in imitation is controversial, there is substantial empirical evidence that parieto-frontal mirror neurons circuits offer a plausible, though not unique, neural substrate for action and intention understanding, which is the basis of imitative behaviour [30, 31]. Secondly, Mostofsky et al. [32] claimed that deficits in imitation are secondary to a general dyspraxia in ASD that is, in turn, due to abnormal sensory–motor integration. Finally, Gowen [33] underlined the importance of action kinematics in correctly imitating goal-less/meaningless actions and postulated a deficit in ASD in perceiving and reproducing kinematics in observed actions. Cook et al. [34] found that individuals with autism even show atypical kinematic profiles when simply asked to move their arm back and forth.
However, while a variety of motor problems (e.g. gross-motor delay, hypotonia, reduced ankle mobility with odd postures and ambulation [“toe-walking”], stereotyped movements, mannerisms, motor apraxia and clumsiness) are associated with ASD [35], not all appear to be specific to this disorder. In fact, difficulties in motor planning and control or problems with repetitive, rapid limb movements, for instance, are also commonly found in ADHD [36–38]. Atypical motor learning patterns and deficits in perceptual-motor integration, by contrast, appear to be specific to ASD, as they have not been found in patients with ADHD in two recent studies [37, 39].
Given the nosological implications of phenomenological, and potentially aetiological, overlap between disorders that have been grouped together as “neurodevelopmental” in DSM-5, and recognising the importance of both motor and imitation abilities for the understanding of ASD, the aims of the present study were as follows. Firstly, and foremost, we wanted to determine the presence and extent of both motor and imitation deficits in patients with ADHD in direct comparison to autistic patients and typically developing (TD) children and adolescents. Secondly, we aimed to determine the potential impact of comorbid ADHD on motor and imitation abilities of ASD patients, which has so far only rarely been studied [40, 41]. Finally, we aimed to compare the interrelationships between motor and imitation abilities as well as potential differences herein in patients with ASD or ADHD.
To this end, motor performance was systematically tested by means of a comprehensive and well-established battery, the Zurich Neuromotor Assessment (ZNA; [42]), in three age-matched and IQ-parallelised groups of TD, ASD, and ADHD children. Imitation abilities, furthermore, were assessed with test batteries of face [43] and ideomotor apraxia [25, 44]. Both test batteries had been employed already in previous studies with ASD subjects [26, 45, 46].
Method
Participants
All 66 participants were aged 6–13 years, male, had IQ > 80, and had neither epilepsy nor any other neurological diseases. Forty-six children were recruited from our in- and out-patient populations with a confirmed diagnosis of ASD or ADHD (see Table 1). All 22 patients with ASD met the criteria for an “autism” or “autism spectrum” diagnosis according to the Autism Diagnostic Observation Schedule diagnostic algorithm (ADOS-G) [47] and were above the cut-off in at least two of the three autism domains of the Autism Diagnostic Interview-Revised (ADI-R) [48]. For both patient groups the diagnostic interview K-SADS-PL [49] was applied to confirm ADHD diagnosis and to screen for ADHD comorbidity within the ASD group. Accordingly, 11 ASD children also fulfilled DSM-IV criteria for ADHD (ASD+: 9.3 ± 2.5 years, IQ = 106.45 ± 16.81 SD) while 11 ASD patients had no ADHD comorbidity (ASD−: 10.8 ± 2.1 years, IQ = 107.01 ± 13.33 SD). Children taking stimulant medication (in almost all cases long-acting methylphenidate) were free from medication for more than 24 h prior to neuromotor and imitation testing, which has been shown to be sufficient time for observing on/off MPH effects on motor functions [50]. N = 20 participants with typical development were recruited from local schools. They had no history of developmental, psychiatric or neurological disorders. The children samples with ASD and typical development have already been analysed and published as part of a larger subjects sample in a previous paper [26].
For cognitive assessment of all participants, WISC-III or -IV were routinely used [51]. If IQ had last been assessed more than 1.5 years prior to a subject’s testing, an updated IQ-score was obtained using the shorter Raven’s Standard Progressive Matrices [52]. Handedness was assessed with the Edinburgh Handedness Inventory [53]. In the total subject sample, two of the 22 ASD, none of the children with ADHD, and two of the 20 TD children, respectively, were left-handed.
Assessment of motor performance
The ZNA is a neuromotor assessment battery in German that provides highly standardised separate measures of timed motor performance and quality of movement, two components of motor competence that show differential developmental courses and substantial inter-individual variation [54, 55]. Furthermore, the ZNA differentiates between so-called “pure” motor tasks (basic simple repetitive, alternating foot and hand movements as well as repetitive and sequential finger movements, and diadochokinesis) and adaptive motor performance (the pegboard task testing coordination of fine-motor skills and tasks of gross-motor coordination and balance such as the dynamic and the static balance task, which are complex sensorimotor tasks requiring an adjustment of motor functions to task demand) [42].
Motor performance was videotaped throughout the assessment. After verbal instructions, along with a brief demonstration of the task through the examiner, children were allowed to practice movements, in order to ensure that they had understood the task, and were instructed to perform the movement as fast as possible. A stopwatch measured the time required for the sequence of movements in each task to be completed according to the manual instructions (timed performance). Quality of movements was provided by counting the degree and frequency of unwanted or superfluous associated movements occurring during all tasks (grouped together as associated movements) and degree of arm deviation during pronation and supination of the hand in the diadochokinesis.
ZNA additionally defines “block components” which aggregate statistically highly redundant variables (e.g. movements of the left and the right limb are pooled together). Block components have been defined to improve intra- and inter-rater reliability as well as test–retest reliability (in excess of 0.9 and 0.7 for block components of timed performance or associated movements, respectively) and consequently do not need further reduction [26, 56].
The following six ZNA block components were used as dependent variables for statistical analyses: four measures of timed motor performance, including (1) pure motor performance (foot, hand, and finger movements); (2) adaptive performance in the pegboard; (3) adaptive performance of dynamic balance and (4) static balance; and the two measures of quality of movement, including (5) diadochokinesis and (6) associated movements (see Table 2).
For all measures, the ZNA provides normative data as z scores for different age groups and gender.
Assessment of imitation abilities
Imitation abilities were assessed in two test batteries explicitly asking participants to imitate a series of oral–facial movements in the (a) German version of the Face Apraxia Tasks (FAT) [43] and socially meaningless hand, finger, and combined finger/hand gestures that were novel, and not object-directed in the (b) Test Battery of Ideomotor Apraxia (TBIA) [44]. During each imitation task the examiner stood in front of the subject and demonstrated the facial expression, the finger and/or hand postures that was to be imitated.
Ad (a) The FAT includes items representing actions of the upper or lower face that are in general familiar but not embedded in a social context in the test situation. Additional verbal instruction is allowed only after direct imitation of the facial expression has been unsuccessful. The two subscales consist of 9 for the upper and 29 items for the lower facial movements. Performance in each item is assessed on a 4-point rating scale (imitation after one attempt (4) or after two attempts (3) and movement execution on first verbal request (2), on second verbal request (1), or no movement execution at all (0)) and thus yield maximum scores of 36 or 116, respectively.
Ad (b) In the TBIA, subjects have to imitate either different configuration of the fingers (finger gestures) or different positions of the hand in relation to the head, with or without additional configuration of the fingers (combined hand–finger gestures and hand gestures alone). All gestures are non-familiar and unrelated to social or tool-use contexts. Equal numbers of trials are performed with the left and right hand. Each gesture imitation is assessed on a 3-point rating scale (no imitation (0), correct imitation with two attempts (1) or correct imitation with one attempt (2)). Each task group includes 14 items and thus yields a maximum score of 28 points. Further details of all test batteries used are given in Biscaldi et al. [26].
Statistical analysis
Statistical analysis comprised two steps. Firstly, for all dependent measures of neuromotor assessment and imitation abilities, a three-way multivariate analysis of variance (MANOVA) was carried out with the independent factor DIAGNOSIS (TD versus ASD versus ADHD). In order to control for possible associations of all motor and imitation variables with general mental abilities, an additional multivariate analysis of covariance (MANCOVA) was computed with IQ as covariate. Post hoc Gabriel’s tests for unequal sample sizes were done to test for significant between-group differences. After splitting the ASD group in ASD+ and ASD− patients, separate ANOVAs compared performance for all motor and imitation variables in these two subgroups. Secondly, since in a previous paper imitation variables were highly correlated within task groups [26], we explored the dimensionality of the imitation variables and possible group differences herein by carrying out Pearson’s correlations (r) and Principal Component Analyses (PCA) for each clinical group separately. Further, after controlling for age effects by normalisation (normative data for motor variables) or residualisation (imitation variables) (see [26]), we determined the interdependencies between the resulting imitation factor (PCA) on the one hand and motor variables on the other, once again using Pearson’s correlations (r) separately for the three groups. For all statistical analyses, a significance level of α = 0.05 was adopted.
Results
Descriptive data for our three groups of participants are shown in Table 1. There were no significant group differences in age (F 2,63 = 0.84, p = 0.43), but we found a significantly higher IQ in the TD as compared with the ADHD group (F 2,63 = 7.62, p = 0.001). In spite of this bias, controlling for IQ made little difference to the results reported below (compare the “MANOVA” and “MANCOVA” columns in Tables 2, 3). To deal with the ambiguity that still surrounds the question of controlling for IQ in studying neurodevelopmental disorders (for a methodological discussion, see Dennis and colleagues [57]), both groups of results, with and without IQ as covariate, are illustrated in the tables.
Neuromotor performance (ZNA)
The MANOVA and MANCOVA results for the neuromotor group comparisons are documented in Table 2. The columns “MANOVA” and “Gabriel” together with the MANCOVA results of this table reveal that, with two exceptions, both patients with ASD and ADHD show similarly impaired motor performance when compared to TD children. The first exception is a lack of any group difference for the variable “Pegboard”; the second exception refers to the balance variables. While patients with ASD showed poorer “dynamic balance” than patients with ADHD and controls, patients with ADHD performed inferior than the other two groups in “static balance”. It should be noted that while the finding of inferior “static balance” in the ADHD group was significant in the MANOVA (F 2,63 = 4.07, p = 0.022), it fell to the trend level after controlling for IQ (F 2,62 = 3.02, p = 0.056).
The separate ANOVA with the two ASD subgroups (ASD− and ASD+) revealed no influence of additional ADHD comorbidity on most of the variables (Fs < 2.71). Only in “static balance”, was there a trend towards poorer performance of ASD+ patients compared to ASD− patients (p = 0.059), consistent with the findings above, linking ADHD symptoms and static balance.
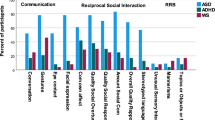
Imitation
Table 3 summarises the MANOVA and MANCOVA results for the imitation variables. The variable “imitation of upper facial movements” (very common everyday facial expressions such as “close your eyes” or “close one eye”, “wrinkle your nose”, “frown”, “blink”) was associated with a ceiling effect in all groups, probably because they were very simple and hence easy to be reproduced by the high-functioning autistic children of this study. All other imitation variables yielded robust overall group differences that were exclusively due to poorer imitation abilities in patients with ASD. Conversely, in none of the imitation variables were ADHD patients impaired. The within-group standard deviations and ranges, however, show that the ASD group as a whole performed more heterogeneously than the other two groups across all aspects of imitation behaviour. As mentioned before, controlling for IQ only slightly reduced our test statistics.
In the separate ANOVA, ASD+ patients underperformed ASD− patients only in the imitation of lower facial movements (F 1,20 = 6.43, p = 0.02).
Relationships between ZNA and imitation variables, and intelligence
While correlations between intelligence and imitation abilities were mostly negligible (0 ≤ rs ≤ 0.25), correlations between intelligence and motor abilities covered a range from small to large (0.13 ≤ r ≤ 0.40), according to conventional effect size classifications [58]. Additionally, IQ was a significant predictor of the block-component pure motor performance (F 1,62 = 5.91, p = 0.018). Consequently, including IQ as a covariate had some effect on the group comparisons in motor variables, but no effect on group differences in the imitation variables (Tables 2, 3, MANCOVA column).
Relationships between ZNA and imitation variables
Since imitation variables generally exhibited high inter-correlations (0.539 ≤ rs ≤ 0.784), a PCA run for all three groups yielded a single imitation factor (called “IMI”), explaining 72 % of the variance in imitation abilities, with factor loadings between 0.802 and 0.903. Within groups, this factor was readily replicable in the TD (explained variance: 69 %, bivariate correlations: .412 ≤ rs ≤ 0.746) and ASD groups (66.3 %; 0.464 ≤ rs ≤ 0.800) (see also [26]). The ADHD group, by contrast, showed correlations that varied between r = −0.326 and r = 0.414 and required 2 factors for their reconstruction (factor 1 loaded finger, combined gestures and facial movements with factor loadings: 0.751, 0.856 and 0.553, respectively; factor 2 loaded hand gestures and again facial movements: 0.853 and −0.706, respectively).
Correlations between the age-residualised IMI factor and the age-normalised ZNA variables, for all three groups separately, revealed large associations only in the ASD group for the block components pure motor performance, peg board, and static balance (0.470 ≤ r ≤ 0.614, ps < 0.05). Correlations corresponded to medium effect sizes in the TD group (r = 0.351, p = 0.13 for the block component associated movements) and negligible-to-medium ones in ADHD children (0.017 ≤ rs ≤ 0.310).
Discussion
In accordance with the recent debate about potential aetiological overlap between ASD and ADHD [7], the present study set out to investigate impairments in motor and imitation abilities in patients with ASD or ADHD that hitherto have been reported primarily for patients with ASD [26, 45, 46]. Our results reveal (1) basic motor dysfunctions in both groups as well as no (significant) differences between the ASD+ and ASD− subgroups; (2) imitation deficits in ASD patients only; and (3) differential patterns of correlations between motor and imitation variables for the ASD (and control) and ADHD groups. These results suggest, that motor dysfunctions may reflect aetiological commonalities between ASD and ADHD, and possibly neurodevelopmental disorders in general. Imitation deficits, by contrast, appear to be specific to ASD and may thus not be part of an overlapping neurodevelopmental aetiology.
Ad (1) The Zurich Neuromotor Assessment revealed on the one hand a similar pattern of deficits in both patient groups, including slower basic movements of fingers/hand, decreased quality of movement (dysdiadochokinesia) with increased involuntary associated movements, but no deficits in fine-motor skills as assessed with the Pegboard test. On the other hand, balance difficulties were once again found in both groups, but were specific for different sets of tasks.
Firstly, we confirm the existence of a similar basic motor deficit both in ASD and ADHD [37, 59] which involves both speed and quality of movements and can be attributed at least partially to problems in the cortico-cerebellar motor networks also involving the basal ganglia and the brainstem [60–62]. Abnormalities in the cortico-brainstem circuitry can be probed with saccade tasks that have recently provided evidence of impaired functioning in ASD patients [63]. The commonality between ADHD and ASD with regard to a general basic motor impairment, reflecting a genuine motor component less dependent on sensory experience and motor learning, is consistent with the putative aetiological links between the two disorders [7], and confirms previous notions that motor deficits could be associated with neurodevelopmental disorders in general [60]. This holds all the more as there were no comorbid autistic disorders in our ADHD sample, as ascertained by our exclusion criteria. Therefore, our results contradict the claim that impaired motor performance in patients with ADHD can be specifically related to autistic traits that may be present but are usually not assessed in the ADHD diagnostic process [41]. Having said that, social responsiveness as a broader ASD-related trait was not directly quantified in our sample. Therefore, we cannot rule out the possibility of a more subtle “sub-clinical” relationship between motor performance and social impairment [40].
Secondly, in spite of these similarities, the findings point to some differences that are worthy of discussion. Whereas the deficit in dynamic balance was more pronounced in those with ASD, static balance problems were found in both groups, but more so in patients with ADHD and in ASD+, compared to ASD− patients, suggesting that impaired static balance is principally related to ADHD symptoms, independent of their co-occurrence with ASD. Although in the present study it narrowly failed to reach significance, the trend is in line with findings previously reported in the literature [64, 65]. Furthermore, while this finding is somewhat sensitive to IQ differences between the samples, the potential link between static balance and ADHD symptoms is also supported by findings showing that postural stability and motor problems in general, like ADHD symptoms, improve with methylphenidate treatment [50, 64, 66]. Yet, further research is necessary to confirm these findings and highlight the mechanisms of this improvement. However, if this finding of balance difficulties in children with ADHD can be replicated, it could be primarily due to their attentional/hyperactivity problems, and this could also be the case when these problems are comorbid with autism. By contrast, the clear impairment in dynamic balance in ASD, independent of comorbidity with ADHD, could point to the aforementioned cortico-cerebellar circuitries via basal ganglia and brainstem, which are responsible for sensorimotor control [60]. Furthermore, this deficit shows a clear persistence in older individuals with ASD [26].
Indeed, the few studies that have recently investigated motor performance in ASD and ADHD have reported that, while such deficits can be found in both groups, they seem to be more severe and persistent in those with ASD [59, 67–69]. This finding indicates that, although motor problems may be present in both ASD and ADHD and thus constitute, on the face of it, a commonality between the two neurodevelopmental disorders, their causes and correlates may be different. Whereas motor problems of ADHD seem to be at least partly associated with their hyperactive–impulsive symptoms [66], motor deficits in ASD are often explained in the light of specific kinematics and sensorimotor problems [34, 37, 70], as also stated by Trevarthen and Delafield-Butt [71].
Moreover, although the sensorimotor circuitry involving the cerebellum may also be related to the balance problems described in ADHD [72], the deficits in dynamic balance in ASD were more severe than those in ADHD. This could point to difficulties in the autism group with increasing task complexity, challenging integration of sensory input with motor output [26, 60]. Increasing difficulties in motor coordination in ASD due to increasing motor complexity have previously been shown for the pegboard test [73]. In our study, however, patients showed no impairment in the pegboard task, relative to the control sample.
Ad (2) In contrast to the commonalities of motor problems deficits, Dewey and colleagues [59] reported a generalised deficit of instructed or imitated gestures in patients with ASD only. In this study, only ASD patients without comorbid ADHD were included. The results of the present study complement Dewey and colleagues’ findings, showing for the first time that ADHD comorbidity is unrelated to the imitation problems of children with ASD. We also show that ASD-specific deficits involve both familiar (facial movements) and completely novel actions and postures that require subjects to copy the form of a demonstrated action without a goal [25]. The results of Dewey and colleagues’ and the present study, furthermore, together suggest that imitation deficits in ASD are independent of intelligence across a wide range of general mental abilities, ranging from intellectual disability (IQ < 70) and low IQ (<80) in Dewey’s sample to average intelligence in the high-functioning autistic patients of the present study. Hence, imitation impairments are specific to ASD and present across the intellectual spectrum (see also [25] and [74]. Moreover, Vivanti et al. [75] tested spontaneous imitative behaviour in pre-schoolers with ASD, in comparison to TD and children with global developmental delay using a more naturalistic setting. They found specific imitation difficulties in ASD, such as reduced spontaneous imitation, reduced attention to faces, and a tendency ‘to emulate’, that is to pursue the goal of an action without reproducing its form and meant meaning. These results extend the findings of imitation difficulties in ASD to settings challenging in the first place attentional mechanisms focusing on others’ actions and motivational mechanisms to imitate them [71]. Intriguingly, individuals with autism are also impaired in recognising [76] and imitating [77] the “style” or “vitality form” (i.e. the dynamic components of movement, form, timing, intention) of an action, that is “how” an action is performed. Vivanti et al. [75], Rochat et al. [76], and Hobson and Hobson [77] are excellent examples of experiments in laboratory settings that nevertheless try to provide some of the naturalistic context in which spontaneous imitation and recognition or, respectively, imitation of emotional components of motor acts normally occurs. Nevertheless, even these studies are somewhat limited in the ecological validity and thus generalisability to proper naturalistic contexts with their high motivational and emotional saliency.Footnote 1 A potential solution to this problem would be designing field studies addressing the spontaneous behaviours of children with ASD in different environments, and associated emotional states. The obvious gain in ecological validity of such a study, however, would be achieved at the expense of its internal validity and thus clarity.
Ad (3) The reported correlation analyses indicate strong associations between the three block components of pure motor performance, pegboard, and static balance, and the imitation factor only in the ASD group, whereas in the TD group one correlation with medium effect size could be found for the block component of associated movements. By contrast, and rather surprisingly, in patients with ADHD these correlations were patchy and not reducible to a single factor.
Since sample sizes were rather small, one should be cautious in interpreting the specific pattern of related parameters. Bearing in mind this limitation, the results are interesting and deserve some discussion. Biscaldi and colleagues [26] already argued that in children with ASD motor coordination skills could be related more specifically to imitation abilities whilst typically developing children show a less specific association between delayed motor functions (measured by the number of needless associated movements) and imitation. With regard to this specific association in autism, the reported deficits in (sensory-) motor coordination and imitation abilities could have been linked through action kinematics.
Action kinematics are impaired in ASD [34, 78] and considered fundamental for the development of social responses [33]. They provide qualitative information of the movement, e.g. about its velocity, acceleration, trajectory and displacement, which is essential to understand the purpose of a motor action and therefore contribute to learning and communication skills [33]. A disruption of this function in ASD is corroborated by the aforementioned study by Rochat et al. [76], who found a deficit in recognising the vitality form or style of an action (also called the “how” a person is doing something) in this group.
Action kinematics thus provide a further link between neural motor “substrates” and the more “cognitive” nature of imitative behaviour beyond the theory of a disruption in the neural network sub-serving the organisation and understanding of motor chains [79]. Considering that children with ASD are also impaired in the imitation of meaningful gestures such as skilled motor acts pretending to use an object [59], this link could be seen in one of the postulated parieto-frontal circuits involving the ventral intraparietal area (VIP) that are supposed to be responsible for mirror mechanisms of body-directed motor acts [30]. This putative relationship seems to be developmentally transient though, as the motor deficits may persist at least into young adulthood, whereas imitation deficits disappear and the relationship between motor variables and imitation weakens during adolescence [26]. Interestingly, Rochat et al. [76] found that the deficit in recognising the vitality form of an action in children with ASD remains stable in adolescents. Furthermore, they stated that, in line with the development of ToM functions, deficits in cognitive-driven processes such as action understanding but not the impaired basic sensorimotor mechanisms necessary for recognising and reproducing the form (including the vitality form) of an action may improve with age.
The strong link between motor and imitation abilities that we found in the ASD patients of our study was greatly reduced in those with ADHD, apparently pointing to another difference between the two disorders. Patients with ADHD, however, show excessive short-term fluctuation of performance that has been called “intra-subject variability” (ISV; [15, 16, 80]). While the stability of individual differences in ISV shows that this construct reflects a trait [81], the variance in performance created by ISV overlays inter-individual differences in (motor or imitation) performance in idiosyncratic ways, thus diminishing correlations between tests (or reliabilities of tests). In line with this reasoning, greater differentiation (that is, more factors) has been reported for ADHD patients compared to controls in a previous study employing a much more homogeneous battery of (cognitive) tests than used here [15].
Limitations of the study
Although subjects were accurately selected, diagnosed and well matched for age, we could not avoid some differences in intelligence level due to bias effects in recruiting subjects with typical development. Additionally, testing of imitation abilities was confined to gestures removed from social or meaningful context. In future research it would be useful to directly compare both kinds of imitation with and without objects to explore the relationship between basic motor functions, the ability of reproducing the motor “form” but also the goal of an action. Furthermore, the exploration of similarities and differences between ADHD and ASD in comparison with comorbid forms would benefit from extending the present results to tasks also eliciting spontaneous imitation and imitation of emotional states.
Conclusion
In conclusion, pending replication in larger samples and more complex study designs, the findings of the present study suggest partial overlap in deficits that have so far mainly been postulated for ASD, in patients with ASD and ADHD. While motor dysfunctions appear common to both disorders and have been shown to be developmentally stable in ASD, imitation deficits appear specific to ASD and decrease during the course of childhood and adolescence [26, 69]. However, longitudinal studies will be necessary to confirm the present findings.
Moreover, ADHD seems to be characterised by increased variability and impulsivity (which may, in turn, reduce motor control). ASD, by contrast, may be better characterised by a genuine impairment of complex sensorimotor integration, leading to stable motor deficits and impaired recognition of kinematics and forms of action and hence reduced ability in reproducing (correctly imitating) gestures and facial expressions. The present study has shown how valuable the joint exploration of basic motor functions and more complex imitation abilities can be when addressing the potential aetiological overlap between these two disorders
It is this “mixture” of disorder-specific and -overlapping features that makes the concept of neurodevelopmental disorders so challenging [82].
Notes
We are grateful to an anonymous reviewer of this article for making us aware of this problem.
References
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th edn. Author, Washington, DC
Leyfer OT, Folstein SE, Bacalman S, Davis NO, Dinh E, Morgan J, Tager-Flusberg H, Lainhart JE (2006) Comorbid psychiatric disorders in children with autism: interview development and rates of disorders. J Autism Dev Disord 36:849–861
Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G (2008) Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry 47:921–929
van Steijn DJ, Richards JS, Oerlemans AM, de Ruiter SW, van Aken MAG, Franke B, Buitelaar JK, Rommelse NNJ (2012) The co-occurrence of autism spectrum disorder and attention-deficit/hyperactivity disorder symptoms in parents of children with ASD or ASD with ADHD. J Child Psychol Psychiatry 53:954–963
Reiersen AM, Constantino JN, Volk HE, Todd RD (2007) Autistic traits in a population-based ADHD twin sample. J Child Psychol Psychiatry 48:464–472
Ronald A, Simonoff E, Kuntsi J, Asherson P, Plomin R (2008) Evidence for overlapping genetic influences on autistic and ADHD behaviours in a community twin sample. J Child Psychol Psychiatry 49:535–542
Rommelse NNJ, Geurts HM, Franke B, Buitelaar JK, Hartman CA (2011) A review on cognitive and brain endophenotypes that may be common in autism spectrum disorder and attention-deficit/hyperactivity disorder and facilitate the search for pleiotropic genes. Neurosci Biobehav Rev 35:1363–1396
Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA (2007) The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry 164:942–948
Fombonne E (2009) Epidemiology of pervasive developmental disorders. Pediatr Res 65:591–598
Baird G, Simonoff E, Pickles A, Chandler S, Loucas T, Meldrum D, Charman T (2006) Prevalence of disorders of the autism spectrum in a population cohort of children in South Thames: the Special Needs and Autism Project (SNAP). Lancet 368:210–215
Kim YS, Leventhal BL, Koh YJ, Fombonne E, Laska E, Lim EC, Cheon KA, Kim SJ, Kim YK, Lee H, Song DH, Grinker RR (2011) Prevalence of autism spectrum disorders in a total population sample. Am J Psychiatry 168:904–912
Ghanizadeh A (2010) Factor analysis on ADHD and autism spectrum disorder DSM-IV-derived items shows lack of overlap. Eur Child Adolesc Psychiatry 19(10):797–798
Grzadzinski R, Di Martino A, Brady E, Mairena MA, O’Neale M, Petkova E, Lord C, Castellanos FX (2011) Examining autistic traits in children with ADHD: does the autism spectrum extend to ADHD? J Autism Dev Disord 41(9):1178–1191
Feige B, Biscaldi M, Saville Christopher WN, Kluckert C, Bender S, Ebner-Priemer U, Hennighausen K, Rauh R, Fleischhaker C, Klein C (2013) On the temporal characteristics of performance variability in attention-deficit hyperactivity disorder (ADHD). PLoS One 8(10):e69674
Klein C, Wendling K, Huettner P, Ruder H, Peper M (2006) Intra-subject variability in attention-deficit hyperactivity disorder. Biol Psychiatry 60:1088–1097
Kuntsi J, Klein C (2012) Intraindividual variability in ADHD and its implications for research of causal links. Curr Top Behav Neurosci 9:67–91
Karalunas SL, Geurts HM, Konrad K, Bender S, Nigg JT (2014) Annual research review: reaction time variability in ADHD and autism spectrum disorders: measurement and mechanisms of a proposed trans-diagnostic phenotype. J Child Psychol Psychiatry 55:685–710
Willcutt EG, Doyle AE, Nigg JT, Faraone SV, Pennington BF (2005) Validity of the executive function theory of attention-deficit/hyperactivity disorder: a meta-analytic review. Biol Psychiatry 57:1336–1346
Happé F, Booth R, Charlton R, Hughes C (2006) Executive function deficits in autism spectrum disorders and attention-deficit/hyperactivity disorder: examining profiles across domains and ages. Brain Cogn 61:25–39
David AS (1992) Frontal lobology—psychiatry’s new pseudoscience. Br J Psychiatry 161:244–248
Schaafsma SM, Pfaff DW, Spunt RP, Adolphs R (2015) Deconstructing and reconstructing theory of mind. Trends Cogn Sci 19(2):65–72
Pellicano E (2007) Links between theory of mind and executive function in young children with autism: clues to developmental primacy. Dev Psychol 43(4):974–990
Pellicano E (2010) The development of core cognitive skills in autism: a 3-year prospective study. Child Dev 81(5):1400–1416
Brunsdon VE, Happé F (2014) Exploring the ‘fractionation’ of autism at the cognitive level. Autism 18(1):17–30
Edwards LA (2014) A meta-analysis of imitation abilities in individuals with autism spectrum disorders. Autism Res 7:363–380
Biscaldi M, Rauh R, Irion L, Jung NH, Mall V, Fleischhaker C, Klein C (2014) Deficits in motor abilities and developmental fractionation of imitation performance in high-functioning autism spectrum disorders. Eur Child Adolesc Psychiatry 23:599–610
Sevlever M, Gillis JM (2010) An examination of the state of imitation research in children with autism: Issues of definition and methodology. Res Dev Disabil 31:976–984
Vanvuchelen M, Van Schuerbeeck L, Roeyers H, De Weerdt W (2013) Understanding the mechanisms behind deficits in imitation: do individuals with autism know ‘what’ to imitate and do they know ‘how’ to imitate? Res Dev Disabil 34:538–545
Rizzolatti G, Fabbri-Destro M, Cattaneo L (2009) Mirror neurons and their clinical relevance. Nat Clin Pr Neurol 5:24–34
Rizzolatti G, Sinigaglia C (2010) The functional role of the parieto-frontal mirror circuit: interpretations and misinterpretations. Nat Rev Neurosci 11(4):264–274
Casartelli L, Molteni M (2014) Where there is a goal, there is a way: what, why and how the parieto-frontal mirror network can mediate imitative behaviours. Neurosci Biobehav Rev 47:177–193
Mostofsky SH, Dubey P, Jerath VK, Jansiewicz EM, Goldberg MC, Denckla MB (2006) Developmental dyspraxia is not limited to imitation in children with autism spectrum disorders. J Int Neuropsychol Soc 12:314–326
Gowen E (2012) Imitation in autism: why action kinematics matter. Front Integr Neurosci 6:117
Cook JL, Blakemore SJ, Press C (2013) Atypical basic movement kinematics in autism spectrum conditions. Brain 136:2816–2824
Fournier KA, Hass CJ, Naik SK, Lodha N, Cauraugh JH (2010) Motor coordination in autism spectrum disorders: a synthesis and meta-analysis. J Autism Dev Disord 40(10):1227–1240. doi:10.1007/s10803-010-0981-3
Fliers E, Rommelse N, Vermeulen SHHM, Altink M, Buschgens CJM, Faraone SV, Sergeant JA, Franke B, Buitelaar JK (2008) Motor coordination problems in children and adolescents with ADHD rated by parents and teachers: effects of age and gender. J Neural Transm 115:211–220
MacNeil LK, Mostofsky SH (2012) Specificity of dyspraxia in children with autism. Neuropsychology 26:165–171
Steger J, Imhof K, Coutts E, Gundelfinger R, Steinhausen HC, Brandeis D (2001) Attentional and neuromotor deficits in ADHD. Dev Med Child Neurol 43:172–179
Izawa J, Pekny SE, Marko MK, Haswell CC, Shadmehr R, Mostofsky SH (2012) Motor learning relies on integrated sensory inputs in ADHD, but over-selectively on proprioception in autism spectrum conditions. Autism Res 5:124–136
Papadopoulos N, Rinehart NJ, Bradshaw JL, Taffe J, McGinley J (2015) Is there a link between motor performance variability and social-communicative impairment in children with ADHD-CT: a kinematic study using an upper limb fitts’ aiming task. J Atten Disord 19(1):72–77. doi:10.1177/1087054712454569
Papadopoulos N, Rinehart N, Bradshaw JL, McGinley JL (2013) Brief report: children with ADHD without co-morbid autism do not have impaired motor proficiency on the movement assessment battery for children. J Autism Dev Disord 43:1477–1482
Largo RH, Fischer JE, Caflisch JA, Jenni OG (eds) (2007) Zürcher Neuromotorik. AWE-Verlag, Zurich
Bizzozero I, Costato D, Sala SD, Papagno C, Spinnler H, Venneri A (2000) Upper and lower face apraxia: role of the right hemisphere. Brain 123:2213–2230
Goldenberg G (1996) Defective imitation of gestures in patients with damage in the left or right hemispheres. J Neurol Neurosurg Psychiatry 61:176–180
Freitag CM, Kleser C, Schneider M, von Gontard A (2007) Quantitative assessment of neuromotor function in adolescents with high functioning autism and Asperger Syndrome. J Autism Dev Disord 37:948–959
Freitag CM, Kleser C, von Gontard A (2006) Imitation and language abilities in adolescents with Autism Spectrum Disorder without language delay. Eur Child Adolesc Psychiatry 15:282–291
Rühl D, Bölte S, Feineis-Matthews S, Poustka F (2004) Diagnostische Beobachtungsskala für Autistische Störungen Deutsche Fassung der Autism Diagnostic Observation Schedule (ADOS) von Catherine Lord, Michael Rutter, Pamela C. Dilavore und Susan Risi. Huber, Bern
Bölte S, Rühl D, Schmötzer G, Poustka F (2005) Diagnostisches Interview für Autismus – Revidiert. Deutsche Fassung des Autism Diagnostic Interview - Revised (ADI-R) von Michael Rutter, Ann Le Couteur und Catherine Lord. Huber, Bern
Kaufman J, Birmaher B, Brent D, Rao U, Ryan N (2001) Kiddie-Sads-Present and Lifetime Version (K-SADS-PL) Version 1.0 of October 1996. German adaptation by K-SADS-Arbeitsgruppe. K-SADS-Arbeitsgruppe, Berlin, Bern, Köln, Frankfurt/M., Hamburg, Jena, Mannheim, Rostock
Bart O, Daniel L, Dan O, Bar-Haim Y (2013) Influence of methylphenidate on motor performance and attention in children with developmental coordination disorder and attention deficit hyperactive disorder. Res Dev Disabil 34:1922–1927
Petermann F, Petermann PU (2008) Hamburg-Wechsler-Intelligenztest für Kinder IV (HAWIK-IV). Huber, Bern
Raven JH (2003) Manual for Raven’s progressive matrices and vocabulary scales. Pearson, San Antonio
Oldfield RC (1971) The assessment and analysis of handedness: the Edinburgh inventory. Neuropsychologia 9:97–113
Largo RH, Caflisch JA, Hug F, Muggli K, Molnar AA, Molinari L, Sheehy A, Gasser ST (2001) Neuromotor development from 5 to 18 years. Part 1: timed performance. Dev Med Child Neurol 43:436–443
Largo RH, Caflisch JA, Hug F, Muggli K, Molnar AA, Molinari L (2001) Neuromotor development from 5 to 18 years. Part 2: associated movements. Dev Med Child Neurol 43:444–453
Rousson V, Gasser T, Caflisch J, Largo R (2008) Reliability of the Zurich Neuromotor Assessment. Clin Neuropsychol 22:60–72
Dennis M, Francis DJ, Cirino PT, Schachar R, Barnes MA, Fletcher JM (2009) Why IQ is not a covariate in cognitive studies of neurodevelopmental disorders. J Int Neuropsychol Soc 15(3):331–343
Cortina JM, Nouri H (2000) Effect size for ANOVA designs higher-order repeated measures designs. Sage Publications, Thousand Oaks
Dewey D, Cantell M, Crawford SG (2007) Motor and gestural performance in children with autism spectrum disorders, developmental coordination disorder, and/or attention deficit hyperactivity disorder. J Int Neuropsychol Soc 13:246–256
Gowen E, Miall RC (2005) The cerebellum and motor dysfunction in neuropsychiatric disorders. Cerebellum 6:268–279
Nayate A, Bradshaw JL, Rinehart NJ (2005) Autism and Asperger’s disorder: are they movement disorders involving the cerebellum and/or basal ganglia? Brain Res Bull 67:327–334
Mostofsky SH, Burgess MP, Gidley Larson JG (2007) Increased motor cortex white matter volume predicts motor impairment in autism. Brain 130:2117–2122
Schmitt LM, Cook EH, Sweeney JA, Mosconi MW (2014) Saccadic eye movement abnormalities in autism spectrum disorder indicate dysfunctions in cerebellum and brainstem. Mol Autism 5(1):47
Stray LL, Stray T, Iversen S, Ruud A, Ellertsen B (2009) Methylphenidate improves motor functions in children diagnosed with Hyperkinetic Disorder. Behav Brain Funct 5:21
Mao HY, Kuo LC, Yang AL, Su CT (2014) Balance in children with attention deficit hyperactivity disorder-combined type. Res Dev Disabil 35:1252–1258
Brossard-Racine M, Shevell M, Snider L, Bélanger SA, Majnemer A (2012) Motor skills of children newly diagnosed with Attention Deficit Hyperactivity Disorder prior to and following treatment with stimulant medication. Res Dev Disabil 33:2080–2087
Kopp S, Beckung E, Gillberg C (2010) Developmental coordination disorder and other motor control problems in girls with autism spectrum disorder and/or attention-deficit/hyperactivity disorder. Res Dev Disabil 31:350–361
Pan CY, Tsai CL, Chu CH (2009) Fundamental movement skills in children diagnosed with autism spectrum disorders and attention deficit hyperactivity disorder. J Autism Dev Disord 39:1694–1705
Van Waelvelde H, Oostra A, Dewitte G, Van Den Broeck C, Jongmans MJ (2010) Stability of motor problems in young children with or at risk of autism spectrum disorders, ADHD, and or developmental coordination disorder. Dev Med Child Neurol 52(8):e174–e178. doi:10.1111/j.1469-8749.2009.03606.x
Whyatt C, Craig C (2013) Sensory-motor problems in Autism. Front Integr Neurosci 7:51
Trevarthen C, Delafield-Butt JT (2013) Autism as a developmental disorder in intentional movement and affective engagement. Front Integr Neurosci 7:49
Buderath P, Gärtner K, Frings M, Christiansen H, Schoch B, Konczak J, Gizewski ER, Hebebrand J, Timmann D (2009) Postural and gait performance in children with attention deficit/hyperactivity disorder. Gait Posture 29:249–254
Duffield TC, Trontel HG, Bigler ED, Froehlich A, Prigge MB, Travers B, Green RR, Cariello AN, Cooperrider J, Nielsen J, Alexander A, Anderson J, Fletcher PT, Lange N, Zielinski B, Lainhart J (2013) Neuropsychological investigation of motor impairments in autism. J Clin Exp Neuropsychol 35:867–881
Williams JHG, Whiten A, Singh T (2004) A systematic review of action imitation in autistic spectrum disorder. J Autism Dev Disord 34:285–299
Vivanti G, Trembath D, Dissanayake C (2014) Mechanisms of imitation impairment in autism spectrum disorder. J Abnorm Child Psychol 42(8):1395-1405. doi:10.1007/s10802-014-9874-9
Rochat MJ, Veroni V, Bruschweiler-Stern N, Pieraccini C, Bonnet-Brilhault F, Barthélémy C, Malvy J, Sinigaglia C, Stern DN, Rizzolatti G (2013) Impaired vitality form recognition in autism. Neuropsychologia 51(10):1918–1924
Hobson RP, Hobson JA (2008) Dissociable aspects of imitation: a study in autism. J Exp Child Psychol 101(3):170–185
Wild KS, Poliakoff E, Jerrison A, Gowen E (2012) Goal-directed and goal-less imitation in autism spectrum disorder. J Autism Dev Disord 42:1739–1749
Cattaneo L, Fabbri-Destro M, Boria S, Pieraccini C, Monti A, Cossu G, Rizzolatti G (2007) Impairment of actions chains in autism and its possible role in intention understanding. Proc Natl Acad Sci USA 104:17825–17830
Kofler MJ, Rapport MD, Sarver DE, Raiker JS, Orban SA, Friedman LM, Kolomeyer EG (2013) Reaction time variability in ADHD: a meta-analytic review of 319 studies. Clin Psychol Rev 33:795–811
Saville CWN, Dean RO, Daley D, Intriligator J, Boehm S, Feige B, Klein C (2011) Electrocortical correlates of intra-subject variability in reaction times: average and single-trial analyses. Biol Psychol 87:74–83
Bishop D, Rutter M (2008) Neurodevelopmental disorders: conceptual approaches. In: Rutter M, Bishop D, Pine D, Scott S, Stevenson J, Taylor E, Thapar A (eds) Rutter’s child and adolescent psychiatry. Blackwell, Oxford, pp 32–41
Acknowledgments
The authors wish to thank Prof. Dr. Christine Freitag for giving us the permission of applying her adapted imitation tasks and for training our doctoral candidates in correctly performing them to assure intra- and inter-rater liability. We also acknowledge her for inspiring us to this study and giving us precious suggestions and commentaries.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical standards
The study protocol has been approved by the local ethics committee and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. The children who volunteered to participate in the study as well as their parents signed an informed consent form before testing began.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Biscaldi, M., Rauh, R., Müller, C. et al. Identification of neuromotor deficits common to autism spectrum disorder and attention deficit/hyperactivity disorder, and imitation deficits specific to autism spectrum disorder. Eur Child Adolesc Psychiatry 24, 1497–1507 (2015). https://doi.org/10.1007/s00787-015-0753-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-015-0753-x