Abstract
In adults with schizophrenia, early response/non-response (ER/ENR) to antipsychotics at 2 weeks robustly predicts ultimate response/non-response (UR/UNR). However, less data about the predictive value of ER/ENR exist in adolescents with schizophrenia. Post hoc analysis of a 6-week trial in adolescents aged 13–17 with schizophrenia were randomized 2:1 to olanzapine or placebo. ER was defined as ≥20 % reduction in Brief Psychiatric Rating Scale-children (BPRS-C) total score at week 2 (ER2) or 3 (ER3); UR was defined with increasing stringency as total BPRS-C score reduction ≥20, ≥30, ≥40 or ≥50 %; remission was defined cross-sectionally using Andreasen et al. (2005) criteria. By week 2 (n = 69) and 3 (n = 66), olanzapine-treated youth achieved 73.3 and 85.5 % of their overall BPRS-C score reduction at 6 weeks last observation carried forward. ER and ENR patients did not differ significantly regarding baseline demographic, illness and treatment variables. ER 2 (frequency = 68.1 %) and ER 3 (frequency = 65.2 %) significantly predicted UR and remission (p = 0.0044–p < 0.0001), with ER3 having more predictive power. A ≥ 20 % BPRS-C reduction threshold for ER had best predictive validity (area under the curve = 0.88–0.92). At 6 weeks, patients with ER had significantly greater improvements in BPRS-C, Clinical Global Impressions Improvement and Severity scores, greater cross-sectional remission and less all-cause discontinuation (p = 0.047–p < 0.0001). Adverse event profiles were similar in the ER and ENR groups. Adolescents with schizophrenia experienced the majority of symptomatic improvement early during olanzapine treatment. ER predicted UR and remission, with ER3 having best predictive power. A ≥ 20 % improvement threshold for defining ER was confirmed as a robust outcome indicator.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Up to one-third of patients with schizophrenia have their first symptoms of psychosis before the age of 18 [1]. Functional impairment occurs most rapidly in the early illness phase [2] and may correlate with a decrease in cerebral gray matter [3, 4]. Moreover, the percent of time spent psychotic in the early illness phase predicts future outcome [5]. Therefore, reducing time of ineffective treatment is crucial. In this context, early prediction of later response to antipsychotic medication and the time course of response to antipsychotics are of considerable interest [6–12]. The lack of biomarkers for antipsychotic response [2] make the use of early response patterns an attractive tool that can be used to guide clinicians in individual decisions regarding the timing of continuation or discontinuation of an antipsychotic trial in patients with schizophrenia [13].
Adults with schizophrenia have shown greater symptomatic improvement in the first 2 weeks of antipsychotic treatment than in subsequent weeks measured as reductions in total scores on the Brief Psychiatric Rating Scale (BPRS, [14]) and Positive and Negative Syndrome Scale (PANSS, [15]) [6, 16], although symptom improvement might be somewhat slower in patients with a first-episode or recent onset psychosis [15–17]. A body of evidence has shown that in adults with schizophrenia, lack of noticeable reduction in total BPRS or PANSS scores at week one or two are statistically significant and clinically relevant predictors of later response status [7–12, 20, 21]. In addition to predicting greater symptom reduction at study endpoint, several post hoc analyses have demonstrated that early responders and early non-responders also differ significantly on outcomes not related to the instrument that defines early response/non-response. For example, compared to early non-responders, early responders have had longer time to all-cause treatment discontinuation [22], lower overall and non-medication related treatment cost [12], and higher levels of social and physical functioning as measured by the medical outcome survey–short form 36 (SF-36) [12].
While the validity and utility of early response/non-response for predicting ultimate outcome has been fairly well established in adults with schizophrenia [13], much less information is available in pediatric patients. Predicting antipsychotic response in the adolescent population is crucial, as youth with early-onset schizophrenia may have lower response patterns than adults [23] and as adolescents undergo crucial biological, psychosocial and educational maturation processes that need to be disturbed for as short a period as possible to not seriously affect the still all too often unfavorable long-term trajectory of the illness [24].
To our knowledge, currently only 2 published studies have examined this issue in adolescents with early-onset schizophrenia [25, 26]. In one post hoc analysis of a large randomized, placebo-controlled trial of aripiprazole in 200 adolescents aged 12–17, reduction of PANSS total scores by ≥20 % at week 2 and, even more so, at week 3 were significantly predictive of ultimate response status at week 6, defined as a ≥ 40 % total PANSS score reduction [25]. In the other study, 79 youth aged 6–19 years with schizophrenia (29 %) or psychotic disorder not otherwise specified (71 %) received naturalistic treatment with clinicians’ choice second-generation antipsychotics (77 % antipsychotic-naïve). Early response was defined as a Clinical Global Impressions Improvement (CGI-I, [27]) rating of at least minimally improved at week 4, which significantly predicted ultimate response at week 12, defined as a CGI-I rating of much or very much improved [26]. These data suggested for the first time that simple and fast CGI-I ratings in the early treatment course could be used in clinical care to identify patients in whom treatment will not yield meaningful efficacy, so that antipsychotics could be changed earlier aiming for sparing of ineffective treatments and possibly faster achievement of ultimate response due to earlier treatment switches.
Since most of the adult data on the early response/non-response paradigm are available for olanzapine and risperidone [8–12, 19, 21], we aimed to examine whether in adolescents with schizophrenia treated for 6 weeks with olanzapine (1) the improvement in total psychopathology is also largest in the first 2 weeks, and (2) early response/non-response defined as a percentage improvement on the BPRS-C total score are significant predictors of response/non-response and remission/non-remission at study endpoint. Based on the adult data and early findings in adolescents reviewed above, we hypothesized that early non-response at week 2 and, possibly, even more so at week 3 would predict ultimate non-response and related poorer outcomes at study endpoint in adolescents with schizophrenia treated with olanzapine both in a statistically and clinically significant way.
Methods
This study was a post hoc analysis of data derived from a randomized, placebo-controlled, multisite 6 week double-blind trial comparing olanzapine and placebo in adolescents with schizophrenia [28]. A brief description of the parent study is provided below; additional details have been published previously [28].
Study design and participants
The RCT study included 107 adolescents aged 13–17 years and diagnosed with schizophrenia according to DSM-IV-TR criteria and by interview and assessment with the schedule for affective disorders and schizophrenia for school-age children––present and lifetime (K-SADS-PL, [29]). Patients could be either inpatients or outpatients and were recruited from multiple sites in the United States (20 sites) and Russia (5 sites) from November 2002 to April 2005. Patients were required to have a total score of 35 or higher on the anchored version of the Brief Psychiatric Rating Scale for children (BPRS-C, [14]), with a score of 3 or higher on at least one of the following BPRS-C items at enrollment and randomization: hallucinations, delusions, or peculiar fantasies.
Eligible patients were randomly assigned in a 2:1 ratio to either olanzapine in flexible doses (2.5–20.0 mg/day) or placebo. Olanzapine was titrated to at least 10.0 mg/day by the third week. Thereafter, investigators were instructed to increase the dose of study medication to the highest tolerated dose, provided there were no tolerability concerns. The present post hoc analyses included only those patients who were allocated to the olanzapine arm (n = 72) and who had at least two post-baseline assessments (at 2 or 3 weeks to assess early response and at least one additional assessment to determine ultimate response) (n = 69).
Efficacy and safety assessments
The primary efficacy measure was the mean change in the BPRS-C total score. Other efficacy outcomes measures included the Positive and Negative Syndrome Scale (PANSS, [15]), the Clinical Global Impressions-Severity Scale (CGI-S, [27]) the Overt Aggression Scale (OAS, [30]) and the Child Health Questionnaire Parent Form 50 (CHQ-PF50, [31]). In addition, changes in the Clinical Global Impressions Improvement Scale (CGI-I, [27]) were evaluated at endpoint.
Safety outcomes included frequency of adverse events and changes in body weight and metabolic measures. Extrapyramidal side effects (EPS) were assessed by the Simpson–Angus Scale (SAS [32]), the Barnes Akathisia Scale (BARS, [33]) and the Abnormal Involuntary Movement Scale (AIMS, [34]). Tests were performed at protocol-specified time-points, when clinically indicated, and when a patient completed the 6-week study period or discontinued early from the study. Fasting (≥8 h) glucose and lipids were collected at baseline and endpoint.
Statistical analysis
The focus of this study was to characterize and predict the trajectory of treatment response in adolescents with schizophrenia treated with olanzapine.
For the purpose of this post hoc analysis, early response (ER) was defined as a ≥20 % reduction in BPRS-C total score at week 2 (ER2) or week 3 (ER3). ENR was defined as a <20 % reduction in BPRS-C total score at week 2 (ENR2) or week 3 (ENR3). Ultimate response (UR) was defined as a percent BPRS-C total score reduction at study endpoint (week 6) of ≥20 % (UR20), ≥30 % (UR30), ≥40 % (UR40) or ≥50 % (UR50) (last observation carried forward, LOCF). Remission was defined at the end of the double-blind phase (LOCF), using the symptom severity component of the standardized remission criteria [35], i.e., a score of ≤3 on 7 BPRS-C indicators, including items 4: conceptual disorganization, 7: mannerisms/posturing, 8: grandiosity, 11: suspiciousness, 12: hallucinatory behavior, 15: unusual thought content, and 16: blunted affect. The time criterion (6 months) of the consensus criteria was not applied owing to the study duration of 6 weeks.
Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were evaluated to determine the value of ER2/NER2 and ER3/NER3 for predicting presence or absence of ultimate response and remission at week 6. Sensitivity was defined as the proportion of ultimate responders who were correctly classified as early responders at week 2 or 3. Specificity was defined as the proportion of ultimate non-responders who were correctly classified as early non-responders at week 2 or 3. PPV was defined as the proportion of early responders at week 2 or 3 who remained responders at week 6, and NPV was defined as the proportion of early non-responders at week 2 or 3 who remained non-responders at week 6.
ER and ENR groups were compared on different variables using descriptive statistics for patient demographics and baseline characteristics, as well as for the proportionate weekly PANSS-T score change relative to the overall PANSS-T score change. ER and the ENR groups were also compared on the BPRS-C total, PANSS total, CGI-S, CGI-I, OAS, CHQ-PF50 scores and all-cause discontinuation, using Chi squared test or t test for categorical and continuous variables, respectively. Furthermore, receiver operating characteristic curves (ROC curves) were calculated for ER2 and ER3 regarding the BPRS-C total score reduction (predicting ≥20, ≥30, ≥40 or ≥50 %) at week 6, to determine the BPRS-C total score improvement threshold at week 2 and week 3 with the best predictive power for ultimate response at week 6.
Finally, stepwise elimination logistic regression models for response and remission (in patients randomized to olanzapine) were performed using baseline variables only or baseline variables, ER status at week 2 or 3 and extrapyramidal side effects (EPS) post-baseline to examine which demographic, illness and treatment characteristics predicted treatment response (defined a priori as ≥40 % reduction in BPRS-C total score) or remission at endpoint.
Although this was a placebo-controlled trial like in prior analyses of early antipsychotic response, we focused on response prediction of patients randomized to olanzapine only; placebo response patterns are the focus of a separate report.
Results
Patient population
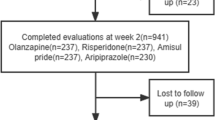
Of 107 adolescents with schizophrenia randomized to 6 weeks of treatment with olanzapine (n = 72) or placebo (n = 35), 69 patients with at least two follow up visits, one of which included week 2 or week 3 were included in the analyses.
Patient disposition has been described in detail previously [28]. Briefly, 49/72 (68.1 %) olanzapine-treated patients completed the 6 week double-blind trial. Of the 23 patients discontinuing early, 10 (13.9 %) discontinued due to lack of efficacy and 5 (6.9 %) due to adverse events.
Baseline demographic, illness and treatment characteristics are shown in Table 1. The majority of patients were male, white and most had been treated previously with antipsychotics. There were no differences between ENR and ER patients in baseline variables except for more ER3 than ENR3 patients having EPS at baseline [15 (35.7 %) vs. 2 (8.7 %), p = 0.02].
Efficacy outcomes
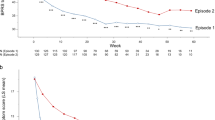
Symptom reduction with olanzapine occurred predominantly early in the first 2 weeks of treatment (Fig. 1). As early as by the end of week 1, on average, 51.1 % of the overall improvement was already achieved with an additional improvement of 22.2 % during week 2 (total = 73.3 %) and 12.2 % during week 3 (85.5 %).
At week 2, 47/69 patients (68.1 %) were ER, and at week 3, 43/66 patients (65.2 %) were ER (Table 2). Significantly more patients identified as early responders at 2 or 3 weeks achieved an ultimate response of ≥40 or ≥50 % reduction in BPRS-C total score at week 6, i.e., UR40: ER2 = 66.0 vs. ENR2 = 13.6 %, p < 0.001 and ER3 = 74.4 vs. ENR3 = 8.7 %, p < 0.001; UR50: ER2 = 51.1 vs. ENR2 = 9.1 %, p = 0.001 and ER3 = 60.5 vs. ENR3 = 0 %, p < 0.001 (Table 2).
Compared to ENR2 patients, ER2 patients had significantly greater improvements in BPRS-C total score at every study week (p = 0.003–p < 0.001) and LOCF endpoint (−16.6 ± 23.2 vs. −50.4 ± 21.2, p < 0.001) (Table 2). Likewise, compared to ENR3 patients, ER3 patients also had significantly greater improvements in BPRS-C total score at every study week and LOCF endpoint (−15.2 ± 20.6 vs. −53.7 ± 20.0, p < 0.001). In addition, ER2 and ER3 patients had significantly greater improvements in LOCF CGI-S and CGI-I scores compared to ENR2 and ENR3 patients (p = 0.047– <0.001). ER3 patients had significantly greater improvement in OAS score (p = 0.02) compared to ENR3 patients, whereas the change in OAS score was not significantly different between ER2 and ENR2 patients (p = 0.15). The changes in CHQ-PF50 were significantly different between ER and ENR patients (p = 0.025–0.006), except for the psychosocial summary mean at week 2 (Table 2). Finally, compared to early non-responders, all-cause discontinuation was significantly less likely in ER2 (p = 0.047) and ER3 (p = 0.018) subjects (Table 2).
Significantly more ER2 than ENR2 patients had remitted at study endpoint [33 (70.2 %) vs. 9 (40.9 %), p = 0.039]. The same was true for ER3 compared to ENR3 patients [34 (79.1 %) vs. 7 (30.4 %), p < 0.001].
Predictive value of early response and non-response
The results of the predictive value analyses of an early response of ≥20 % reduction in BPRS-C total score at week 2 or week 3 for predicting ultimate response and remission at week 6 are summarized in Table 3. Early response at week 3 generally had slightly better predictive power than early response at week 2 for both ultimate response and remission. The same was true for the prediction of ultimate non-response via presence of early non-response. For UR40 and UR50, the specificity (86–100 %) and PPV (91–100 %) were high, while the sensitivity (51–74 %) and NPV (46–66 %) were moderate.
Regarding the prediction of remission, ER2 and ER3 showed moderate and somewhat lower predictive validity than for UR. Consistent with the findings for UR, values for remission were higher regarding sensitivity (70–79 %) and PPV (79–83 %) than for specificity (59–70 %) and NPV (48–64 %), and ER3 had the best predictive validity for remission with both sensitivity and PPV of around 80 %.
Receiver operating characteristic (ROC) curves to determine the best cut-off for early response/non-response
To find the optimal cut-off threshold of the psychopathological improvement at 2 or 3 weeks to predict response/non-response or remission/non-remission at week 6, ROC curves were generated for the reduction in BPRS-C total score at week 2 and week 3 (Table 4). At 2 weeks, a cut-off threshold of 19.8 % reduction to predict ≥20 % reduction showed the highest accuracy (accuracy = 84 %) and the greatest area under the curve (AUC = 0.88). At 3 weeks, cut-off thresholds of 20.0 and 38.7 % reduction to predict ≥20 and ≥50 % reduction, respectively, at week 6, showed the highest accuracy (accuracy = 83.3, 84.8 %) and the greatest AUC (AUC = 0.92, 0.91). Except for the ER3 of 38.7 % to predict ≥50 % reduction, all other optimal cut-off points for ER2 and ER3 to predict a percentage response at week 6 were around 20 % (19.8–23 %). This was also true for remission, where ROC curves showed optimal cut-off points of 16 % reduction in BPRS-C total score at week 2 and 20 % at week 3 to best predict remission at week 6.
Predictors of ultimate response and remission
The logistic regression analysis showed that predictors of response (defined as ≥40 % reduction in BPRS-C total score) were ER2 (p = 0.0001), ER3 (p < 0.0001), a lower baseline AIMS total score (0.041–0.044), a higher baseline SAS total score (p = 0.047), male gender (p = 0.0075) and a higher baseline BPRS-C withdrawal score (p = 0.026) (Table 5). Predictors of remission were ER2 (p = 0.0044), ER3 (p = 0.0003) and a lower baseline CGI-Severity score (p = 0.0007–0.0013) (Table 5).
Adverse effect outcomes
There were no differences in adverse effect outcomes between ER2/ER3 patients and ENR2/ENR3 patients, except for ER3 patients having a greater improvement in EPS assessed by the Simpson–Angus Scale compared to ENR3 patients (p = 0.008) (Table 6). Both ER and ENR patients gained body weight over the 6 weeks of treatment and increased mean blood cholesterol, triglycerides and fasting glucose from baseline to endpoint. Moreover, around 45 % of the patients gained ≥7 % of body weight (Table 6).
Discussion
Main findings from this post hoc analysis of a 6-week randomized, double-blind, placebo-controlled trial of olanzapine vs. placebo for adolescents suffering from schizophrenia include: (1) most of the symptomatic improvement with olanzapine was achieved by weeks 1 and 2; (2) ER and ENR patients did not differ significantly with regards to baseline demographic, illness and treatment variables; (3) ER2 and even more so ER3 significantly predicted UR and remission; (4) a threshold for ER of ≥20 % BPRS-C reduction was confirmed as having the best predictive validity for UR; (5) patients with ER had better efficacy than NER patients on almost all other efficacy outcomes that were independent of the BPRS-C, which was used to define ER, while adverse effects did not differ significantly between ER and NER patients; (6) ER2 and ER3 remained significant predictors of UR in multivariable regression analyses that only identified one or two additional clinical predictors.
Our finding that patients achieved most of the symptomatic response early in treatment (51 % by week 1, 73 % by week 2 and 86 % by week 3) is consistent with studies in adults with schizophrenia where the improvement up to week 2 was significantly larger than the additional improvement up to week 4 [6, 36] or where the 4-week improvement was larger than symptom reductions over the next 11 months [16, 36]. Similarly, our findings are also consistent with emerging data in adolescents with schizophrenia [25] or youth with schizophrenia spectrum disorders [26], in whom most of the symptomatic improvement also occurred in the first 2–4 weeks of a new treatment trial. Nevertheless, the relative symptomatic improvement at week 1 was double than that seen in a 6-week double-blind randomized trial with aripiprazole, in which at week 1 and 2 about 25 % of the overall PANSS total score reduction was seen [25]. This difference may be due to more sedating effects of olanzapine, potentially leading to a reduction in general psychopathology, variations in the titration speed until therapeutic dose levels were reached, or in the overall PANSS score reduction from baseline (which was larger in the aripiprazole arms (−31 points) [37] than in the olanzapine arm (−21 points) [28], with parallel differences in the placebo response (−21 and −9 points, respectively)).
In line with studies in adults [7–12, 38, 39] and emerging pediatric data [25, 26], we confirmed that early responders at week 2 or 3 had significantly better outcomes across a variety of efficacy measures. Exceptions were the isolated lack of a difference in the psychosocial summary score of the CHQ-PF50 between ER2/NER2 at week 6, as functional improvement may take longer than 6 weeks, and in adverse effects in this short-term study. Moreover, in a 6-week, placebo-controlled study of adolescents with schizophrenia treated with aripiprazole [25], early response/non-response status at week 3 was more predictive of ultimate outcome than early response/non-response status at week 2.
Similar to prior work in adults [9, 13] and the common practice in the literature on ER in schizophrenia, we found with the exception of a single outlier (ER3 of 38.7 % to predict UR50) that thresholds of around 20 % (16–23 %) reduction of BPRS-C total score at week 2 or 3 were the optimal cut-off point for ER to predict UR and remission. Using equipercentile linking, the ≥20 % reduction in PANSS (or Brief Psychiatric Rating Scale) scores was found to be comparable to “minimal improvement” on the CGI-I scale [40]. Since the CGI-I can easily be utilized in busy clinical settings, it should be considered in clinical care, as lack of at least minimal improvement on the CGI-I at week 4 was shown to predict UNR at week 12, defined as much or very much improved on the CGI-I in youth with schizophrenia spectrum disorders [26].
Using this 20 % improvement threshold in BPRS-C total score at week 2 or 3 to define ER or ENR, 65 % of the olanzapine-treated adolescents with early-onset schizophrenia were categorized as ER. This two-third figure for ER status is higher than that found in a study of adolescents with early-onset schizophrenia randomized to aripiprazole, where ER2 and ER3 was achieved by 33 and 49 %, respectively [25]. However, the early response frequency of about 65 % is also higher than that reported in adult studies, where frequencies were 43–47 % in first-episode schizophrenia [18, 38] and 22–30 % in chronic schizophrenia also treated with olanzapine [10–12]. Reasons for this difference in the proportion of early responders are unclear, but could possibly relate to differences in pre-baseline exposure to antipsychotics and degree of required washout, which each will affect pre-baseline response status and baseline severity of psychopathology. Another possibility is that olanzapine and aripiprazole have differing levels and/or time course of efficacy, yet these findings should be followed up in future studies, ideally comparing different antipsychotics head-to-head.
Further, our results suggest that prediction of UR may be more accurate in adolescents with schizophrenia than prediction of UNR, at least when treated with olanzapine. From a clinical point of view, however, NPV and specificity for prediction of ultimate non-response are the most important variables, since an accurate and early identification of non-responders provides an opportunity of changing treatment to more effective options without exposure of patients to ultimately ineffective or suboptimal treatments. For UR40 and UR50, the specificity was between 86 and 100 %. Thus, most or all of the patients who were ultimate non-responders at week 6 were already early non-responders at week 2 or 3. Nevertheless, while PPV was high (91–100 %), sensitivity (51–74 %) and NPV (46–66 %) were only moderate, indicating that 2 or 3 weeks may not suffice to reliably identify youth with schizophrenia who will not have sufficient benefit from longer treatment with the same antipsychotic. These results are somewhat in line with data from adults with first-episode schizophrenia [18, 19] in whom also a longer time until ultimate treatment response was observed than reported in studies with more chronic patients, even though this difference was not significant in a recent meta-analysis comparing the predictive validity of early response/non-response in first-episode and chronic samples [13]. However, these data contrast with the findings from the study of adolescents with schizophrenia treated with aripiprazole where ER at week 2 and 3 had very favorable NPVs for UR40 of 81.7 and 93.6 % [25]. Although these discrepant findings could also be influenced by different response rates in the two populations, these varying results underscore the need to identify additional clinical and biomarkers of response to antipsychotics in patients with schizophrenia. Moreover, recent work has extended the early antipsychotic response paradigm that dichotomizes the early illness course and uses this to predict UR and remission to examining different trajectories of symptomatic change from baseline to endpoint [41–44]. Other approaches have included trying to identify a smaller number of most predictive individual PANSS items that comprise the early response, rather than using a cut-off across ratings of all 30 PANSS items [45]. It remains to be seen how this work can inform individualized clinical decision making in the future.
Finally, using multivariable regression analyses, we confirmed that ER2 and ER3 remained robust and significant predictors of UR and remission, even when entering baseline variables as potential moderators and change in the severity of symptom severity in EOS subjects as potential mediators. In addition, higher BPRS-C withdrawal and baseline SAS scores, lower baseline AIMS scores and male sex predicted response, whereas lower baseline CGI-S score predicted remission. Studies in adults found next to early response higher baseline psychopathology scores to be predictive of UR, whereas lower baseline psychopathology scores predicted remission at endpoint [46–48]. In our study, only higher baseline BPRS-C withdrawal scores were associated with greater response, but we also found that patients with less CGI severity, i.e., those closer to remission, were more likely to achieve remission during the 6-week study. The finding that higher baseline SAS scores were associated with a higher likelihood of UR may relate to a change from antipsychotics with higher EPS potential that can interfere with full therapeutic benefits in youth [26] and adults [49]. Similarly, higher baseline, but not 4-week akathisia ratings were found in subsequently non-remitting first-episode schizophrenia subjects [17]. The finding that lower AIMS baseline scores were associated with achieving UR is consistent with findings in adults with chronic schizophrenia indicating that patients with tardive dyskinesia respond more poorly to antipsychotics [50], possibly indicating greater disruption of physiological dopamine transmission. Finally, although male sex has traditionally been associated with poorer antipsychotic response, recent findings have been more heterogeneous, which may have to do with the time frame of observation. Interestingly, male sex no longer predicted poor treatment outcome in the majority of recent studies that focused on the early post-acute period, whereas studies that confirmed a poorer outcome in males with a first-episode of schizophrenia reported mostly on time frames of at least one year [2].
Strengths and limitations
Results from this study must be interpreted within its limitations. First, the study was a post hoc analysis and since the study was a randomized controlled trial, its generalizability to everyday clinical samples may be reduced. Second, we were only able to evaluate early improvement and its predictive validity within the first 6 treatment weeks, whereas prediction of longer-term outcome is also very important. Third, our outcome variables did not extend to subjective wellbeing or daily functioning at school, work or interpersonally. On the other hand, strengths of this study include the use of standardized assessment instruments, double-blind treatment assignment and symptom ratings, relatively low dropout rate, use of a single antipsychotic and reasonable large sample size of adolescents with early-onset schizophrenia.
Conclusions
Adolescents with schizophrenia treated with olanzapine achieved the majority of symptomatic improvement during the first 1–2 weeks of treatment. Early response at 2 and 3 weeks predicted ultimate response and remission at week 6, with ER3 having the best predictive power. ER patients were more likely to maintain their improvements through the study endpoint, while ENR did not have similarly high predictive power for UNR. A 20 % improvement threshold for defining ER was confirmed as a robust measure. ER and ENR should be assessed and considered as valuable information for clinical decision making in youth with early-onset schizophrenia. Additional research is needed to enable more individualized antipsychotics treatment and determination of the best time and circumstance for either continuing an antipsychotic trial in a patient with still insufficient response or discontinuing the trial and switching to another agent.
References
Young CM, Findling RL (2004) Pharmacologic treatment of adolescent and child schizophrenia. Expert Rev Neurother 4(1):53–60
Carbon M, Correll CU (2014) Clinical predictors of therapeutic response to antipsychotics in schizophrenia. Dialogues Clin Neurosci 16(4):505–524
Buckley PF, Correll CU, Miller AL (2007) First-episode psychosis: a window of opportunity for best practices. CNS Spectr S12(15):1–12 discussion 13-4; quiz 15-6
Lieberman JA, Perkins DO, Jarskog LF (2007) Neuroprotection : a therappeutic strategy prevent deterioration associated with schizophrenia. CNS Spectr 12(S4):1–13
Harrison G et al (2001) Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry 178:506–517
Agid O et al (2003) Delayed-onset hypothesis of antipsychotic action: a hypothesis tested and rejected. Arch Gen Psychiatry 60(12):1228–1235
Correll CU et al (2003) Early prediction of antipsychotic response in schizophrenia. Am J Psychiatry 160(11):2063–2065
Leucht S et al (2007) Early prediction of antipsychotic nonresponse among patients with schizophrenia. J Clin Psychiatry 68(3):352–360
Leucht S et al (2008) Predicting antipsychotic drug response—replication and extension to six weeks in an international olanzapine study. Schizophr Res 101(1–3):312–319
Kinon BJ et al (2008) Predicting response to atypical antipsychotics based on early response in the treatment of schizophrenia. Schizophr Res 102(1–3):230–240
Kinon BJ et al (2010) Early response to antipsychotic drug therapy as a clinical marker of subsequent response in the treatment of schizophrenia. Neuropsychopharmacology 35(2):581–590
Ascher-Svanum H et al (2008) Clinical, functional, and economic ramifications of early nonresponse to antipsychotics in the naturalistic treatment of schizophrenia. Schizophr Bull 34(6):1163–1171
Samara MT, Leucht C, Leeflang MM, Anghelescu IG, Chung YC, Crespo-Facorro B, Elkis H, Hatta K, Giegling I, Kane JM, Kayo M, Lambert M, Lin CH, Möller HJ, Pelayo-Teran JM, Riedel M, Serretti M, Zhao JJ, Correll CU, Leucht S (2015) Early improvement predicts later response to antipsychotics in schizophrenia: a diagnostic test review. Am J Psychiatry (in press)
Overall JE, Pfefferbaum B (1982) The brief psychiatric rating scale for children. Psychopharmacol Bull 18:10–16
Kay SR, Fiszbein A, Opler LA (1987) The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 13(2):261–276
Leucht S et al (2005) Early-onset hypothesis of antipsychotic drug action: a hypothesis tested, confirmed and extended. Biol Psychiatry 57(12):1543–1549
Derks EM et al (2010) Antipsychotic drug treatment in first-episode psychosis: should patients be switched to a different antipsychotic drug after 2, 4, or 6 weeks of nonresponse? J Clin Psychopharmacol 30(2):176–180
Emsley R, Rabinowitz J, Medori R (2006) Time course for antipsychotic treatment response in first-episode schizophrenia. Am J Psychiatry 163(4):743–745
Gallego JA et al (2011) Time to treatment response in first-episode schizophrenia: should acute treatment trials last several months? J Clin Psychiatry 72(12):1691–1696
Chang YC et al (2006) Optimizing early prediction for antipsychotic response in schizophrenia. J Clin Psychopharmacol 26(6):554–559
Schennach-Wolff R et al (2010) An early improvement threshold to predict response and remission in first-episode schizophrenia. Br J Psychiatry 196(6):460–466
Liu-Seifert H, Adams DH, Kinon BJ (2005) Discontinuation of treatment of schizophrenic patients is driven by poor symptom response: a pooled post hoc analysis of four atypical antipsychotic drugs. BMC Med 3:21
Sikich L et al (2008) Double-blind comparison of first- and second-generation antipsychotics in early-onset schizophrenia and schizo-affective disorder: findings from the treatment of early-onset schizophrenia spectrum disorders (TEOSS) study. Am J Psychiatry 165(11):1420–1431
Clemmensen L, Vernal DL, Steinhausen HC (2012) A systematic review of the long-term outcome of early onset schizophrenia. BMC Psychiatry 12:150
Correll CU et al (2013) Early antipsychotic response to aripiprazole in adolescents with schizophrenia: predictive value for clinical outcomes. J Am Acad Child Adolesc Psychiatry 52(7):689–698.e3
Stentebjerg-Olesen M et al (2013) Early nonresponse determined by the clinical global impressions scale predicts poorer outcomes in youth with schizophrenia spectrum disorders naturalistically treated with second-generation antipsychotics. J Child Adolesc Psychopharmacol 23(10):665–675
Guy W (1976) Clinical global impression ECDEU assessment manual for psychopharmacology, revised. National Institute of Mental Health, Rockville
Kryzhanovskaya L et al (2009) Olanzapine versus placebo in adolescents with schizophrenia: a 6-week, randomized, double-blind, placebo-controlled trial. J Am Acad Child Adolesc Psychiatry 48(1):60–70
Kaufman J et al (1997) Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 36(7):980–988
Yudofsky SC et al (1986) The Overt Aggression Scale for the objective rating of verbal and physical aggression. Am J Psychiatry 143(1):35–39
Landgraf JM, Abetz N (1996) Measuring health outcomes in pediatric populations; issues in psychometrics and application. Qual Life Pharmacoeco Clin Trials 2:793–802
Simpson GM, Angus JW (1970) A rating scale for extrapyramidal side effects. Acta Psychiatr Scand Suppl 212:11–19
Barnes TR (1989) A rating scale for drug-induced akathisia. Br J Psychiatry 154:672–676
Schooler NR, Kane JM (1982) Research diagnoses for tardive dyskinesia. Arch Gen Psychiatry 39(4):486–487
Andreasen NC et al (2005) Remission in schizophrenia: proposed criteria and rationale for consensus. Am J Psychiatry 162(3):441–449
Agid O, Seeman P, Kapur S (2006) The “delayed onset” of antipsychotic action—an idea whose time has come and gone. J Psychiatry Neurosci 31(2):93–100
Findling RL et al (2008) A multiple-center, randomized, double-blind, placebo-controlled study of oral aripiprazole for treatment of adolescents with schizophrenia. Am J Psychiatry 165(11):1432–1441
Stauffer VL et al (2011) Early response to antipsychotic therapy as a clinical marker of subsequent response in the treatment of patients with first-episode psychosis. Psychiatry Res 187(1–2):42–48
Hatta K et al (2011) Difference in early prediction of antipsychotic non-response between risperidone and olanzapine in the treatment of acute-phase schizophrenia. Schizophr Res 128(1–3):127–135
Leucht S et al (2005) Clinical implications of brief psychiatric rating scale scores. Br J Psychiatry 187:366–371
Levine SZ, Leucht S (2010) Elaboration on the early-onset hypothesis of antipsychotic drug action: treatment response trajectories. Biol Psychiatry 68(1):86–92
Schennach R et al (2012) Response trajectories in “real-world” naturalistically treated schizophrenia patients. Schizophr Res 139(1–3):218–224
Nordon C et al (2014) Trajectories of antipsychotic response in drug-naive schizophrenia patients: results from the 6-month ESPASS follow-up study. Acta Psychiatr Scand 129(2):116–125
Pelayo-Terán JM et al (2014) Trajectories of symptom dimensions in short-term response to antipsychotic treatment in patients with a first episode of non-affective psychosis. Psychol Med 44(1):37–50
Ruberg SJ et al (2011) Identification of early changes in specific symptoms that predict longer-term response to atypical antipsychotics in the treatment of patients with schizophrenia. BMC Psychiatry 11:23
Schennach-Wolff R et al (2011) Predictors of response and remission in the acute treatment of first-episode schizophrenia patients–is it all about early response? Eur Neuropsychopharmacol 21(5):370–378
Crespo-Facorro B et al (2007) Predictors of acute treatment response in patients with a first episode of non-affective psychosis: sociodemographics, premorbid and clinical variables. J Psychiatr Res 41(8):659–666
Emsley R et al (2006) Remission in first-episode psychosis: predictor variables and symptom improvement patterns. J Clin Psychiatry 67(11):1707–1712
Schennach-Wolff R et al (2011) Influencing factors and predictors of early improvement in the acute treatment of schizophrenia and schizophrenia spectrum disorder. J Psychiatr Res 45(12):1639–1647
Ascher-Svanum H et al (2008) Tardive dyskinesia and the 3-year course of schizophrenia: results from a large, prospective, naturalistic study. J Clin Psychiatry 69(10):1580–1588
Acknowledgments
The original randomized controlled trial was funded and conducted by Eli Lilly and Company. However, the study sponsor had no further role in the design of the current study, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
Conflicts of interest
Drs. Stentebjerg-Olesen and Jeppesen report no conflicts of interest. Dr. Ganocy has received salary support from AstraZeneca and Eli Lilly. Dr. Chang is an unpaid consultant for GlaxoSmithKline, Merck, Bristol-Myers Squibb; has received research funding from GlaxoSmithKline and Merck and is on the DSMB for Sunovion. Dr. DelBello reports the following: Research Support from Eli Lilly Otsuka GlaxoSmithKline Merck Martek Novartis Lundbeck Shire Purdue Amylin Sunovion Pfizer, lecture bureau membership for Otsuka, Bristol-Myers Squibb, and consulting/Advisory Board/Honoraria/Travel with Pfizer, Dey, Lundbeck, Sunovian, Otsuka, Supernus, Dr. Findling receives or has received research support, acted as a consultant and/or served on a speaker’s bureau for Alexza Pharmaceuticals, American Academy of Child & Adolescent Psychiatry, American Physician Institute, American Psychiatric Press, AstraZeneca, Bracket, Bristol-Myers Squibb, Clinsys, CogCubed, Cognition Group, Coronado Biosciences, Dana Foundation, Forest, GlaxoSmithKline, Guilford Press, Johns Hopkins University Press, Johnson & Johnson, KemPharm, Lilly, Lundbeck, Merck, NIH, Novartis, Noven, Otsuka, Oxford University Press, Pfizer, Physicians Postgraduate Press, Rhodes Pharmaceuticals, Roche, Sage, Seaside Pharmaceuticals, Shire, Stanley Medical Research Institute, Sunovion, Supernus Pharmaceuticals, Transcept Pharmaceuticals, Validus, and WebMD. Dr. Kane has been a consultant and/or received honoraria from Amgen, Alkermes, Bristol-Myers Squibb, Eli Lilly, Forrest Labs, Genentech, IntraCellular Therapies. Janssen, Johnson and Johnson, Lundbeck, MedAvante, Novartis, Otsuka, Roche, Reviva, Sunovion,. He is a shareholder of MedAvante. Dr. Tohen was an Eli Lilly full time employee when the study was conducted (until 2008) and has received honoraria or consulted for AstraZeneca, Bristol-Myers Squibb, Glaxo-SmithKline, Forest, Eli Lilly, Johnson & Johnson, Merck, Otsuka, Sepracor, Sunovion, Lundbeck and Wyeth Corporations; his spouse was a fully time employee at Eli Lilly (until 2013). Dr. Correll has been a consultant and/or advisor to or has received honoraria from: AbbVie, Actavis, Alkermes, Bristol-Myers Squibb, Eli Lilly, Genentech, Gerson Lehrman Group, IntraCellular Therapies, Janssen/J&J, Lundbeck, MedAvante, Medscape, Otsuka, Pfizer, ProPhase, Roche, Sunovion, Supernus, and Takeda. He has received grant support from the American Academy of Child and Adolescent Psychiatry BMS, Janssen/J&J, National Institute of Mental Health (NIMH), Novo Nordisk A/S, Otsuka, Takeda and the Thrasher Foundation.
Ethical standards
The study has been approved by the appropriate ethics committee and has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All persons gave their informed consent prior to their inclusion in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stentebjerg-Olesen, M., Ganocy, S.J., Findling, R.L. et al. Early response or nonresponse at week 2 and week 3 predict ultimate response or nonresponse in adolescents with schizophrenia treated with olanzapine: results from a 6-week randomized, placebo-controlled trial. Eur Child Adolesc Psychiatry 24, 1485–1496 (2015). https://doi.org/10.1007/s00787-015-0725-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-015-0725-1