Abstract
Half of mental disorders have their first onset before adulthood when the presence of a disorder may be particularly disruptive to developmental milestones. Retrospective prevalence estimates have been shown to underestimate the burden of mental illness and scarce data are available on the incidence of disorders throughout the adolescent period, especially in developing countries. Thus, the objective was to determine the incidence of mental disorders in an 8-year period from adolescence to young adulthood, onset of service use and their predictors in a Mexican cohort. 1071 respondents from a representative two-wave panel sample participated in the Mexican Adolescent Mental Health Survey in 2005 and in the follow-up survey in 2013. Disorders were evaluated with the World Mental Health Composite International Diagnostic Interview. 37.9 % experienced the onset of a psychiatric disorder and 28.4 % sought services for the first time. Substance use disorders had the greatest incidence, followed by mood and behavior disorders, anxiety disorders and lastly eating disorders. Sex, age, school dropout, childhood adversities and prior mental disorders predicted the onset of new disorders. Being female, having more educated parents and most classes of disorder predicted first time service use. These findings contribute to a paradigm shift in conceptions of mental disorder similar to how we think of common physical afflictions as near universal experiences across the life course, but less frequent at any given moment. Adolescents are particularly vulnerable. Therefore, public health policy should focus on early universal promotion of positive mental health and structural determinants of mental health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite the evidence that at least half of all psychiatric disorders around the world emerge before age 21 [1], there are few longitudinal studies of the incidence of these disorders from adolescence to emerging adulthood. Considering the important developmental milestones and social role changes of this period, such as culminating educational attainment, entering the work force, partner selection and parenthood, a psychiatric illness at this stage can have lasting consequences into adulthood [2]. It is important to understand the incidence of psychiatric disorders during this transitional period for several reasons. The developmental timing of psychiatric disorders may shed light on the etiology of disorders. Incidence studies are more powerful than retrospective studies for establishing risk factors [3], reduce the memory bias of retrospective reports of prevalence [4] and thus are less likely to underestimate treatment needs. Therefore, incidence data are necessary to guide public health policy and services.
In developing countries like Mexico, estimating the incidence of psychiatric disorders in adolescence is particularly important because this age group is a larger proportion of the population and their problems may go undetected because of early school dropout and less access to mental health services. While longitudinal studies of psychiatric disorders throughout adolescence have been carried out in developed countries [5–8], none to our knowledge has been carried out in developing countries or in Latin America. Even of those carried out in developed countries, only a few have included a wide range of psychiatric disorders over the whole adolescent period in representative samples [5] or reported incidence rates [8].
One of the most comprehensive longitudinal surveys to evaluate the development of mental disorders over time starting in childhood and now with data that spans into early adulthood is the Great Smoky Mountains Study, a representative sample of rural areas of Southeastern United States, following 1420 children up to 11 times between the ages of 9 and 26 [9, 10]. While within any 3-month period during childhood, only 13.3 % met criteria for a DSM-IV disorder [10], by age 21, 61.1 % met criteria for a disorder and an additional 21.4 % for subclinical problems, bringing the cumulative psychiatric burden to 82 % [9]. Even in the Early Developmental Stages of Psychopathology Study which covered a more narrow age range (14–17 at baseline) over a shorter follow-up period (19.7 months), there was an incidence of 25.2 % of any disorder during that short time period and a cumulative prevalence of 50.1 % [10]. Despite these groundbreaking studies, there is a lack of documentation of incidence rates across a broad range of disorders, covering the entire adolescent period, and in diverse populations.
Despite the strikingly high cumulative prevalence and incidence estimates for mental disorders in adolescence, mental health service use is likely to be lower in adolescents than in either children or adults, as children usually have regular general medical checkups, their problems may be identified by schools and they are under parental control. Adolescents, on the other hand, cannot seek services without parental involvement (consent, paying for services), but may also reject parental insistence to seek help and generally no longer have regular medical checkups. How mental health service use, its barriers and facilitators, changes in the transition from childhood to adolescence to early adulthood is important to understand in order to reduce unmet mental health needs. Low rates of mental health counseling in adolescents persist and are even lower in young adults (mean age 21.5) [11]. Female gender, high maternal education, school attendance and routine physical examinations were found to be predictive of mental health counseling in young adults [11]. In Mexico, a large proportion of adolescents and emerging adults are no longer in school nor have routine medical checkups.
Prospective longitudinal studies have begun to replicate relevant risk factors for mental disorders found consistently in cross-sectional studies, providing valuable insights into the risk factors for incident mental disorders in adolescence and emerging adulthood such as socio-demographic characteristics (sex, age, socio-economic level, family constellation), childhood adversities, and prior mental disorders [6, 9, 12]. Despite the “waxing and waning” of mental disorders [8] and the high comorbidity of disorders during this life stage [13], the specificity of risk factors for specific types of incident disorder is unclear.
The objective of this study, therefore, was to determine the incidence of mental disorders in an 8-year period from adolescence to young adulthood, the utilization of services for these disorders, and the predictors of incident disorders and service use in a Mexican cohort.
Methods
Participants
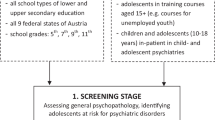
1071 young adults aged 19–26 were re-interviewed in 2013, 8 years after they were originally interviewed as adolescents when they were between 12 and 17 years of age. The period of incidence thus covers the age span of 12–26. The wave I survey was a stratified multistage area probability sample representative of the nearly two million adolescents that resided in the Mexico City Metropolitan Area at that time. 3005 participants completed the wave I interview with a 71 % response rate. Further details of the wave I sample design and procedures have been previously reported [14].
2763 (91.9 %) of the original 3005 participants provided contact information in 2005. Of those, we were able to locate 2470 (89.4 %) households. Of the households which were found, no informant had or was willing to provide information on the whereabouts of 622 (25.1 %) participants, 101 (4.1 %) moved away to another city, state or country, 12 (0.5 %) had died, 2 (0.1 %) were in jail and 5 (0.2 %) were hospitalized. Of the remaining 1728 participants eligible for interview, 128 (7.4 %) declined to participate, 517 (29.9 %) were not found at home on any of the visits, and 12 (0.7 %) had incomplete interviews. Thus, a response rate of 62.0 % of eligible participants was obtained, though this was only 35.6 % of the wave I sample.
Procedures
Face-to-face interviews were conducted in the homes of the participants by trained lay interviewers after providing a verbal and written explanation of the study and obtaining informed consent. All study participants were given a pamphlet of the study findings from wave I and contact information for institutions from which they could seek services should they wish to do so. The Internal Review Board of the National Institute of Psychiatry approved the research.
Diagnostic assessment
Mental disorders were assessed at both waves with the World Mental Health version of the WHO Composite International Diagnostic Interview 3.0 (CIDI) [15], a fully structured computer-assisted interview that generates diagnoses for DSM-IV mental disorders including mood disorders, anxiety disorders, substance use disorders, disruptive behavior disorders and eating disorders. Wave I used the adolescent version of the CIDI [16, 17] while Wave II used the adult version modified for follow-up. Follow-up modification consisted of preloading wave I diagnoses in the program such that for each disorder, those who met criteria in 2005 were asked only about symptomatology for that disorder in the years since wave I whereas those who did not meet criteria for the disorder in 2005 were asked about lifetime symptomatology for that disorder. Clinical reappraisal interviews have found generally good concordance between DSM-IV diagnoses from the CIDI and those from the Structured Clinical Interview for DSM-IV Axis I Disorders [18]. Incident cases of a disorder were defined as those that developed a disorder between waves I and II among those who never had the disorder at wave I. Incident cases of a disorder class were defined as those who developed any one of the disorders in that class (anxiety, mood, disruptive behavior, substance, eating) between waves I and II among those who never had any disorder from that class at wave I. The CIDI included retrospective reports of the age-at-onset of disorders based on a question sequence shown to improve recall accuracy [19]. Participants that did not meet disorder criteria at wave I, but at wave II reported a lifetime disorder with an age of onset three or more years before their age at wave I, were excluded as incident cases to provide more conservative estimates.
Assessment of service use
The CIDI also included information regarding service use for mental health problems. Services included treatment in the healthcare sector (mental health specialty and general health services) as well as services sought in non-healthcare settings (schools, human services such as religious advisors and complementary alternative services such as traditional healers).
Assessment of socio-demographic predictors
The CIDI assessed general socio-demographics. We included the following information from wave I: sex, age, family constellation, educational and employment status of the participant, and the educational attainment and income of their parents. Family constellation was categorized as living with both parents (or not) in 2005. Participants were considered students if enrolled as a student in 2005 (or dropouts if not). Adolescents were asked whether they worked during the school year, whether they were ever married and whether they had children. The participants were asked about the educational attainment of each of their parents and that of the parent with the highest level. Parental household income was categorized into tertiles. The number of childhood adversities was the sum of having experienced the following 12 events as measured by the CIDI (physical abuse, neglect, sexual abuse, parent with a mental illness, parent with a substance use problem, parent with criminal behavior, witnessing domestic violence, death of a parent, parental divorce, other parental loss, serious physical illness, and economic adversity).
Weights
To assess possible study attrition bias, χ 2 tests were performed which tested differences in socio-demographic and mental health characteristics of those participants that were re-interviewed versus those that were not. The variables that showed bias were used to calculate weights using the WTADJUST procedures in SUDAAN software to ensure that wave II participants represented the initial wave I sample.
Analysis
Cross-tabulations were used to estimate 8-year incidence of psychiatric disorders and service use. To estimate prospective associations of risk factors with incident disorder and service use, risk ratios (RR) were calculated as functions of average marginal predictions from fitted logistic regression models [20]. Average marginal predictions allow comparisons of predictive outcomes (risk) between groups of people in the population, after controlling for differences in covariate distributions between the groups. We preferred to estimate the RR directly instead of using odds ratios (OR), which is now feasible with standard software [21] and to evaluate the same 8-year period for all instead of a classical time-to-event analysis which requires exact knowledge of the time of event occurrence. We used the SUDAAN 11.0.1 software package to obtain point estimates, standard errors, confidence intervals, and p values for the parameters and contrasts of interest using the Taylor series method [22]. Multivariate significance was evaluated using Wald χ 2 tests and 0.05 as the probability level. Sensitivity analyses of the logistic regression models were performed without weighting, which resulted in RRs in the same direction and of similar magnitude.
Results
Attrition
Table 1 shows un-weighted wave I socio-demographic and mental health characteristics of those re-interviewed in wave II versus those that were not re-interviewed. Females, those who lived with both parents, and students at wave I were more likely to be followed up whereas age, parental education, and parental income showed no attrition bias. Most importantly, there were no differences for type or any lifetime mental disorder between those who were and were not re-interviewed. Thus, in subsequent analyses, the sample of participants was weighted for sex, living with both parents and being a student at wave I.
Wave II socio-demographic characteristics of the follow-up sample are presented on Table 2. Between the ages of 19 and 26, almost half continued to live with both parents (48.1 %), a third were students (32.5 %) and a fifth had some college education (21.2 %). Slightly more than a third were married and 36.2 % already had children.
Incidence of psychiatric disorders and service use
The 8-year incidence of psychiatric disorders and service use for the total sample and by sex is shown on Table 3. During the adolescent years into emerging adulthood, 37.9 % experienced the onset of a new psychiatric disorder. With regard to type of disorders, the greatest incidence was of substance use disorders (24.5 %), followed by mood and disruptive behavior disorders (14.0 and 14.2 % respectively), anxiety disorders (7.0 %) and lastly eating disorders (3.7 %). With regard to individual disorders, the greatest incidence was found for alcohol abuse (18.3 %), major depression (12.9 %), and intermittent explosive disorder (10.4 %). Females had greater incidence than males of specific phobia, social phobia, posttraumatic stress disorder, major depression and bulimia. Males had greater incidence than females of alcohol abuse, alcohol dependence, drug abuse and drug dependence. Of those who had not previously sought treatment for mental health problems, 28.6 % utilized services with greater incident service use for females than males.
Predictors of psychiatric disorder incidence
Table 4 shows the results of five separate multiple logistic regression equations, one for the prediction of each of the following classes of disorder: any incident anxiety disorder, mood disorder, disruptive behavior disorder, substance use disorder and eating disorder. With regard to socio-demographic predictors, females had greater risk of an incident anxiety (RR 1.75, 95 % CI 1.28–2.41) and mood disorder (RR 1.33, 95 % CI 1.03–1.72) and less risk for developing a substance use disorder (RR 0.42, 95 % CI 0.33–0.53). The oldest adolescents (aged 16–17 at wave 1) had less risk of developing any anxiety (RR 0.65, 95 % CI 0.47–0.88) and mood disorder (RR 0.72, 95 % CI 0.54–0.97). High parental income increased risk for disruptive disorders (RR 1.39, 95 % CI 1.01–1.92). Dropping out of school predicted any incident disruptive (RR 1.37, 95 % CI 1.04–1.83) and substance use disorder (RR 1.45, 95 % CI 1.15–1.82).
With regard to prior psychiatric disorders, having a prior anxiety disorder predicted a subsequent mood (RR 1.43, 95 % CI 1.07–1.92), disruptive (RR 1.35, 95 % CI 1.05–1.73) and substance use disorder (RR 1.25, 95 % CI 1.02–1.52). Having a prior mood disorder predicted only a subsequent anxiety disorder (RR 1.53, 95 % CI 1.09–2.13), though the relative risk ratios for all classes of incident disorders were above one, but not statistically significant. Having a prior disruptive disorder increased the risk for developing an anxiety (RR 1.47, 95 % CI 1.03–2.11), mood (RR 1.57, 95 % CI 1.14–2.17) and substance disorder (RR 1.62, 95 % CI 1.22–2.15). Neither prior substance nor eating disorders increased risk for other disorders.
Finally, having experienced three or more childhood adversities increased the risk for any incident anxiety (RR 1.71, 95 % CI 1.13–2.58) and disruptive disorder (RR 1.81, 95 % CI 1.30–2.51).
Predictors of service use incidence
Table 5 presents the results of a multiple logistic regression equation for the prediction of any incident service use. Incident service use was predicted by female gender (RR 1.31, 95 % CI 1.08–1.60), greater parental education (RR 1.26, 95 % CI 1.07–1.48 for high school versus primary education and RR 1.91, 95 % CI 1.55–2.36 for university versus primary education) and all lifetime disorders except eating disorders (RRs ranging from 1.22 for disruptive behavior disorders to 1.70 for mood disorders). Age, family constellation, dropping out of school and parental income did not predict incident service use.
Discussion
Study limitations
These findings should be considered within the context of the study’s limitations. The validity of estimates from prospective surveys may be adversely affected by sample attrition [23, 24], which we corrected here with post-stratification weights. The suggestion that attrition rate does not affect estimates of associations between variables, even for attrition rates as high as 70 % [25], gives us further confidence in our findings. However, we cannot be certain that some factor that we did not evaluate in our attrition analysis may have biased our follow-up sample in some relevant way. Fortunately, we found no attrition bias for mental disorders.
Having only two waves, 8 years apart and no measurements in between, may contribute to recall bias. On the one hand, caseness at baseline is likely to have been underestimated due to lifetime recall (thus overestimating first incidence at follow-up). On the other hand, incident disorders that emerged and remitted between the waves may have been forgotten thus underestimating incidence. These opposing effects may cancel each other out, if of similar magnitude.
The wide age span from 12 to 17 years of age at first assessment may be considered a limitation in terms of the heterogeneity of the developmental stage of the participants. On the other hand, it permitted us to cover the entire adolescent through early adulthood period which would have required a much longer follow-up period if the initial sample were of the same age.
A further limitation is that despite the high incidence of mental disorders found in this sample, the incidence of any particular disorder (except alcohol abuse) is low, such that risk factors for individual disorders could not be evaluated with the desirable precision. Thus, we chose to evaluate risk factors for classes of disorders, assuming that disorders within the same class share common risks. Even as a class, incidence for eating disorders and anxiety disorders was low such that lack of significant results, particularly for eating disorders, may be due to lack of statistical power.
Study strengths and noteworthy findings
Despite these limitations, this study has important strengths such as covering the complete adolescent period into emerging adulthood, a more comprehensive range of mental disorders than previous studies, and a population of youth from a developing country in Latin America for which scarce epidemiologic information is available. We found several noteworthy findings. First, over a third of youth experienced the first onset of a mental disorder during the adolescent years into emerging adulthood, substance use disorders having, by far, the greatest incidence during this stage. Sex, age, school dropout, childhood adversities and prior mental disorders predicted the onset of new disorders. Of the total sample, 28 % had incident service use, principally in the health sector, which was predicted by being female, greater parental education and having any class of disorder (except eating disorders).
Incidence of mental disorders
While we expected a high incidence rate given that prior studies in Mexico and across the globe suggest that half of all lifetime mental disorders have their first onset by age 21 [1, 26], our estimates surpassed the lifetime prevalence estimate of 26.1 % for a nationally representative sample of adults in Mexico and reached the projected estimate of lifetime prevalence by age 65 of 36 % [26]. One plausible explanation is that this generation of youth is more affected than earlier generations. There is contradictory evidence in the international literature regarding whether younger cohorts are more affected than earlier generations [1, 27–29]. Even if true, it is not likely to explain the full magnitude of these differences. Another likely explanation is that the aforementioned lifetime prevalence estimate is greatly underestimated due to the recall bias of retrospective reports as adults may forget earlier episodes. This explanation is supported by the findings of Moffitt and colleagues that the prevalence estimates of lifetime mental disorders to age 32 were doubled in prospective as compared to retrospective data [30]. In fact our incidence rates are consistent with the incidence rate of 25 % reported for a German adolescent sample in a 19.7-month period [8], the 61 % cumulative prevalence up to age 21 in a Southern US sample [5], and the lifetime prevalence at age 19 of 45 % in a Dutch sample [31].
It is not surprising that substance use disorders have the greatest incidence among disorders given the social context of substance use in this age group and structural factors in Mexico City which make substances readily available to youth. Convenience stores sell alcohol 24 h a day, businesses sell alcohol in close proximity to schools and target students [32], and there is lax enforcement of laws against selling alcohol to minors [33]. The low incidence of anxiety disorders during adolescence and the reduced risk ratios of the oldest adolescents for anxiety disorders may be due to the age of peak incidence having passed, as retrospective ages of onset of anxiety disorders are typically in childhood [1].
Risk factors for incident disorders
With regard to socio-demographic predictors and similar to what has been reported in other studies, females were more likely to develop an anxiety and mood disorder and less likely to develop a substance use disorder compared to males [34]. Age was inversely related to incident anxiety and mood disorders suggesting that new anxiety and mood disorder onset levels off in early adulthood and that the period of greater vulnerability is early to mid adolescence. Dropping out of school increased risk for the onset of disruptive behavior and substance use disorders, but not for internalizing disorders which helped elucidate the temporal order of the associations between school dropout and mental disorders found in cross-sectional studies [35, 36].
With regard to predictive trajectories of disorders, prior anxiety and disruptive behavior disorders predicted subsequent internalizing and externalizing disorders, whereas mood disorders predicted only subsequent anxiety disorders and substance use and eating disorders did not predict future disorders. Previous research on trajectories from childhood to adolescence to adulthood have generally found that anxiety and mood disorders predict each other while behavioral disorders predict mood and anxiety disorders, but not vice versa [9, 37].
Finally, the number of prior childhood adversities was associated to the onset of anxiety and disruptive disorders, but not to other disorder classes whereas prior retrospective reports have found associations with all classes of disorders [38].
Incidence and risk factors for service use
Universal health coverage was implemented in Mexico a decade ago, enrolling over 41 million Mexicans previously uninsured, which might account for these higher than expected rates of first service use. Although we cannot discount that these are a result of having received information on mental health service resources at wave I. Our finding of female gender promoting service utilization is consistent with other studies of adolescent and emerging adult populations in other countries [11, 39]. Similar to the findings of Amone-P´lak and collegues [40], service use was predicted by parental education rather than parental income, suggesting that higher SES associated to service use may be due to more educated parents having more information regarding mental health and mental health resources and thus more able to detect attention needs in their children, rather than fewer economic barriers. Therefore, strategies to promote mental health literacy in less educated families might increase mental health service utilization.
Conclusion
These findings coupled with the estimates for cumulative prevalence in other longitudinal studies confirm the recent assertions of various psychiatric epidemiologists that mental disorders are not only common, but nearly universal over the life course, similar to common physical disorders such as colds, the flu, injuries, etc. [5, 30, 31]. This suggests an important paradigm shift from viewing psychiatric disorders as rare phenomenon, severely affecting the unlucky few (an abnormality which engenders stigma) to a view more similar to how we think of common physical afflictions as a near universal experience, varying in severity, persistence and chronicity, and infrequent at any given moment.
These findings have important public health policy and service implications. The underestimation of retrospective reports needs to be complimented with data from prospective studies for a more accurate estimation of the burden of mental disorders. The near ubiquity of mental disorders across the life course raises questions regarding the feasibility and need for treating all cases. The greater magnitude of incident and lifetime prevalence estimates to point prevalence estimates in the literature suggests that many remit without treatment. This indicates the need for refining our understanding of the longitudinal course of disorders to determine which cases remit without treatment, if those remitted cases recover their functioning to predisorder levels or maintain disability in some areas, which cases have significant long-term disability, and which cases will benefit most from treatment. Because of the limited viability of treating all cases, it is particularly important to strengthen early promotion of positive mental health in universal settings such as schools, target structural determinants of mental health rather than individual determinants [41], and redistribute mental health attention to primary care rather than secondary or tertiary care. While the latter has been an objective of the World Health Organization, in Mexico 80 % of the budget for mental health services is for tertiary psychiatric hospitals [42]. Furthermore, a public awareness of this mental health paradigm shift from rare to common disorders might help address issues of stigma.
References
Kessler RC, Angermeyer M, Anthony JC et al (2007) Lifetime prevalence and age of onset distributions of mental disorders in the World Health Organization’s World Mental Health Surveys. World Psychiatry 6:168–176
Fergusson DM, Woodward LJ (2002) Mental health, educational and social role outcomes of adolescents with depression. Arch Gen Psychiatry 59:225–231. doi:10.1001/archpsyc.59.3.225
de Graaf R, ten Have M, Tuithof M, van Dorsselaer S (2013) First-incidence of DSM-IV mood, anxiety and substance use disorders and its determinants: results from the Netherlands Mental Health Survey and Incidence Study-2. J Affect Disord 149:100–107. doi:10.1016/j.jad.2013.01.009
Simon GE, VonKorff M (1995) Recall of psychiatric history in cross-sectional surveys: implications for epidemiologic research. Epidemiol Rev 17:211–227
Copeland WE, Shanahan L, Costello EJ, Angold A (2011) Cumulative prevalence of psychiatric disorders by young adulthood: a prospective cohort analysis from the Great Smoky Mountain Study. J Am Acad Child Adolesc Psychiatry 50:252–261. doi:10.1016/j.jaac.2010.12.014
Fergusson DM, Woodward LJ (2001) The christchurch health and development study: a review of findings on child and adolescent mental health. Aust N Z J Psychiatry 35:287–296
Patton GC, Coffey C, Romaniuk H, Mackinnon A, Carlin JB, Degenhardt L, Olsson CO, Moran P (2014) The prognosis of common mental disorders in adolescents; a 14-year prospective cohort study. Lancet 383:1404–1411. doi:10.1016/S0140-6736(13)62116-9
Wittchen HU, Lieb R, Pfister H, Schuster P (2000) The waxing and waning of mental disorders: evaluating the stability of syndromes of mental disorders in the population. Compr Psychiatry 41:122–132. doi:10.1016/S0010-440X(00)80018-8
Copeland WE, Shanahan L, Costello EJ, Angold A (2009) Which childhood and adolescent psychiatric disorders predictor which young adult disorders? Arch Gen Psychiatry 66:764–772. doi:10.1001/archgenpsychiatry.2009.85
Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A (2003) Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry 60:837–844. doi:10.1001/archpsyc.60.8.837
Yu JW, Adams SH, Burns J, Brindis CD, Irwin CE (2008) Use of mental health counseling as adolescents become young adults. J Adolesc Health 43:268–276. doi:10.1016/j.jadohealth.2008.01.009
Oldehinkel AJ, Ormel J (2014) A longitudinal perspective on childhood adversities and onset risk of various psychiatric disorders. Eur Child Adolesc Psychiatry. doi:10.1007/s00787-014-0540-0
Kessler RC, Avenevoli S, McLaughlin KA, Greif Green J, Lakoma MD, Petukhova M, Pine DS, Sampson NA, Zaslavsky AM, Merikangas KR (2012) Lifetime comorbidity of DSM-IV disorders in the NCS-R Adolescent Supplement (NCS-A). Psychol Med 42:1997–2010. doi:10.1017/S0033291712000025
Benjet C, Borges G, Medina-Mora ME, Zambrano J, Aguilar-Gaxiola S (2009) Youth mental health in a populous city of the developing world: results from the Mexican Adolescent Mental Health Survey. J Child Psychol Psychiatry 50:386–395. doi:10.1111/j.1469-7610.2008.01962.x
Kessler RC, Üstün TB (2004) The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). Int J Methods Psychiatr Res 13:93–121. doi:10.1002/mpr.168
Kessler RC, Avenevoli S, Green J, Gruber MJ, Guyer M, He Y, Jin R, Kaufman J, Sampson NA, Zaslavsky AM (2009) National comorbidity survey replication adolescent supplement: III. Concordance of DSM.IV/CIDI diagnoses with clinical reassessments. J Am Acad Child Adolesc Psychiatry 48:386–399. doi:10.1097/CHI.0b013e31819a1cbc
Merikangas KR, Avenevolli S, Costello EJ, Koretz D, Kessler RC (2009) National comorbidity survey replication adolescent supplement: I. Background and measures. J Am Acad Child Adolesc Psychiatry 48:367–379. doi:10.1097/CHI.0b013e31819996f1
Haro JM, Arbabzadeh-Bouchez S, Brugha TS, de Girolamo G, Guyer ME, Jin R, Lepine JP, Mazzi F, Reneses B, Vilagut G, Sampson NA, Kessler RC (2006) Concordance of the composite international diagnostic interview version 3.0 (CIDI 3.0) with standardized clinical assessments in the WHO World Mental Health surveys. Int J Methods Psychiatr Res 15:167–180
Knauper B, Cannell CF, Schwarz N, Bruce ML, Kessler RC (1999) Improving the accuracy of major depression age of onset reports in the US National Comorbidity Survey. Int J Methods Psychiatr Res 8:39–48
Graubard BI, Korn EL (1999) Predictive margins with survey data. Biometrics 55:652–659
Bieler GS, Brown GG, Williams RL, Brogan DJ (2010) Estimating model-adjusted risks, risk differences, and risk ratios from complex survey data. Am J Epidemiol 171:618–623
Wolter K (1985) Introduction to variance estimation. Springer, New York
Eaton WW, Anthony JC, Tepper S, Dryman A (1992) Psychopathology and attrition in the epidemiologic catchment area surveys. Am J Epidemiol 135:1051–1059
de Graaf R, Bijl RV, Smit F, Ravelli A, Vollebergh WA (2000) Psychiatric and sociodemographic predictors of attrition in a longitudinal study: the Netherlands Mental Health Survey and Incidence Study (NEMESIS). Am J Epidemiol 52:1039–1047
Gustavson K, von Soestm R, Karevold E, Roysamb E (2012) Attrition and generalizability in longitudinal studies: findings from a 15-year population-based study and Monte Carlo simulation study. BMC Public Health 12:918. doi:10.1186/1471-2458-12-918
Medina-Mora ME, Borges G, Benjet C, Lara C, Berglund P (2007) Psychiatric disorders in Mexico: lifetime prevalence and risk factors in a nationally representative sample. Br J Psychiatry 190:521–528
Collishaw S, Maughan B, Goodman R, Pickles A (2004) Time trends in adolescent mental health. J Child Psychol Psychiatry 45:1350–1362
Costello EJ, Erkanli A, Angold A (2006) Is there an epidemic of child and adolescent depression? J Child Psychol Psychiatry 47:1263–1271
Sourander A, Koskelainen M, Niemelä S, Rihko M, Ristkari R, Lindroos J (2012) Changes in adolescents mental health and use of alcohol and tobacco: a 10-year time-trend study of Finnish adolescents. Eur Child Adolesc Psychiatry 21:665–671. doi:10.1007/s00787-012-0303-8
Moffitt TE, Caspi A, Taylor A, Kokaua J, Milne BJ, Polanczyk G, Poulton R (2010) How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychol Med 40:899–909. doi:10.1017/S0033291709991036
Ormel J, Raven D, van Oort F, Hartman CA, Reijneveld SA, Veenstra R, Vollebergh WAM, Buitelaar J, Verhulst FC, Oldehinkel AJ (2014) Mental health in Dutch adolescents: a TRAILS report on prevalence, severity, age of onset, continuity and co-morbidity of DSM disorders. Psychol Med 45:260–345
Reidl Martinez LM, Gonzlez-Gonzalez A (2012) El contexto como la oferta de alcohol dirigía a jóvenes. In: Medina-Mora ME (ed) Alcohol y políticas públicas [Alcohol and Public Policy]. El Colegio Nacional, Mexico City, pp 101–140
Lange JE, Voas RB (2000) Youth escaping limits on drinking: binging in Mexico. Addiction 95:521–528
Seedat S, Scott KM, Angermeyer MC et al (2009) Cross-national associations between gender and mental disorders in the World Health Organization World Mental Health Surveys. Arch Gen Psychiatry 66:785–795. doi:10.1001/archgenpsychiatry.2009.36
Benjet C, Hernández-Montoya D, Borges G, Méndez E, Medina-Mora ME, Aguilar-Gaxiola S (2012) Youth who neither study nor work: mental health, education and employment. Salud Pública Mex 54:410–417
Breslau J, Miller E, Joanie Chung WJ, Schweitzer JB (2011) Childhood and adolescent onset psychiatric disorders, substance use, and failure to graduate high school on time. J Psychiatry Res 45:295–301. doi:10.1016/j.jpsychires.2010.06.014
Costello EJ, Copeland W, Angold A (2011) Trends in psychopathology across the adolescent years: what changes when children become adolescents and when adolescents become adults? J Child Psychol Psychiatry 52:1015–1025. doi:10.1111/j.1469-7610.2011.02446.x
Kessler RC, McLaughlin KA, Green JG et al (2010) Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. British J Psychiatry 197:378–385. doi:10.1192/bjp.bp.110.080499
Alexandre P (2008) Mental health care for youth: predictors of use are not always the same as predictors of volume. Soc Sci J 45:619–632. doi:10.1016/j.soscij.2008.09.004
Amone-P´Olak K, Ormel J, Oldehinkel AJ, Reijneveld SA, Verhulst FC, Buger H (2010) Socioeconomic position predicts specialty mental health service use independent of clinical severity: The TRAILS study. J Am Acad Child Adolesc Psychiatry 49:647–655
Clark J (2014) Medicalization of global health 2: the medicalization of global mental health. Global Health Action 7:24000. doi:10.3402/gha.v7.24000
IESM-OMS informe sobre el sistema de salud mental en México [IESM-WHO report on the mental Health system in Mexico] (2011). http://www.who.int/mental_health/who_aims_country_reports/who_aims_report_mexico_es.pdf. Accessed 19 January 2015
Acknowledgments
Wave I of the Mexican Adolescent Mental Health Survey was supported by the National Council on Science and Technology and Ministry of Education (Grant CONACYT-SEP-SSEDF-2003-CO1-22). Wave II was supported by the National Council on Science and Technology (Grant CB-2010-01-155221) with supplementary support from Fundación Azteca. The survey was carried out in conjunction with the World Health Organization World Mental Health (WMH) Survey Initiative. We thank the WMH staff for assistance with instrumentation, fieldwork, and data analysis.
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical Standards
This study was approved by the ethics committee of the National Institute of Psychiatry Ramón de la Fuente and therefore has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. At wave I, all participants were minors and thus gave their assent while their parents or legal guardians gave informed consent prior to their inclusion in the study. At wave II, all participants gave their informed consent.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Benjet, C., Borges, G., Méndez, E. et al. Eight-year incidence of psychiatric disorders and service use from adolescence to early adulthood: longitudinal follow-up of the Mexican Adolescent Mental Health Survey. Eur Child Adolesc Psychiatry 25, 163–173 (2016). https://doi.org/10.1007/s00787-015-0721-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-015-0721-5