Abstract
Objectives
To update the findings of a systematic review from the year 2016 on the evidence for the accuracy and potential benefits of cone beam computed tomography (CBCT) in periodontal diagnostics.
Material and methods
A systematic literature search was performed and the criteria for PICO, PRISMA and risk of bias assessment were applied. Only clinical trials (> 10 patients) conducted in humans on periodontal bone loss, i.e. vertical and/or horizontal or furcation involvement, in CBCT compared with clinical and/or conventional radiographic measures were included.
Results
From 1152 articles identified, 11 case series on furcations and eight on vertical and/or horizontal bone loss were included. The studies showed moderate risk of bias and heterogeneous study designs. The agreement between non-surgical clinical or two-dimensional radiographic assessments of horizontal, vertical or interfurcal bone loss and CBCT measurements was analysed in 11 studies and was low in six studies with comparable study designs. A high accuracy (80–84%) of CBCT measurements compared with intra-surgical findings of furcation involvement was observed in four studies. Comparing CBCT with intra-surgical measurements of vertical or horizontal bone loss, an accuracy between 58 and 93% was found in four out of six studies. Three studies were analysed and indicated benefits of CBCT in decision making and/or a reduction of treatment costs and time in teeth of interest.
Conclusions
The findings provide additional evidence for the accuracy of CBCT in assessing periodontal bone loss.
Clinical relevance
CBCT is an accurate diagnostic tool in periodontology, which needs to be carefully considered in certain situations.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In 2016, we published a systematic review on the evidence of the applicability of cone beam computed tomography (CBCT) for periodontal diagnosis and treatment planning [1]. In this work, we detected limited evidence since we were able to include seven case series with respect to furcation-involved molars and/or vertical bone defects only. However, the analysis indicated that CBCT may provide an accurate analysis of periodontal defect morphology compared with conventional clinical and two-dimensional radiographic measurements. Additionally, one study showed that CBCT may facilitate treatment decisions and improve patient-related outcome measures (PROMS), such as treatment costs and time [2, 3]. When comparing the years 2015 and 2020, the number of studies investigating the use of dental CBCT accessible in the electronic scientific database “PubMed” has dramatically increased, i.e. PubMed hits in the year 2015, 3201; in the year 2020, 7429, and an update therefore may be indicated [4].
Thus, the aim of the present systematic review was to update the best available external evidence for the diagnostic accuracy and potential benefits of dental CBCT in periodontal diagnosis and treatment planning.
Material and methods
Registration
The review protocol was registered in the PROSPERO international prospective register of systematic reviews hosted by the National Institute for Health Research (NIHR), University of York, Center for Reviews and Dissemination (applied for on July 11, 2019).
Protocol
The present systematic review was conducted according to the PRISMA (Preferred Reporting Items for Systematic Review and Meta-Analyses) criteria [5, 6] and to current guidelines of systematic review updates [7, 8] (Online Resource 1).
The PI(E)CO (Population, Intervention/Exposure, Comparison, Outcomes) method was applied to define the research questions [9]. For the purpose of this review, two terms need to be defined: “agreement” was used for the comparison between dental CBCT and non-surgical clinical and/or two-dimensional radiographic findings, and “accuracy” was used for the comparison between dental CBCT and intra-surgical clinical findings. The specific questions for this update were slightly modified and addressed as follows:
In patients suffering from periodontitis (P), which agreement, accuracy and/or benefit (O) of dental CBCT compared with findings obtained from clinical and/or conventional radiographic measurements (C) can be expected in assessing teeth with:
-
(a)
Furcation involvement (FI) (I)?
-
(b)
Vertical and/or horizontal bone loss (I)?
Outcome measures
The primary outcome measures were:
-
i.
Agreement of dental CBCT compared with non-surgical clinical and/or two-dimensional radiographic findings of FI, vertical and/or horizontal bone loss, and
-
ii.
Accuracy of dental CBCT compared with intra-surgical clinical findings (so-called gold standard of measurement accuracy) of FI, vertical and/or horizontal bone loss.
Any potential benefit of a dental CBCT use in terms of PROMS, e.g. cost benefit, reduction of treatment time and/or favourable decision making, was considered as secondary outcome parameter.
Eligibility criteria
Publications were considered eligible for inclusion in this systematic review if they presented the following parameters:
-
1.
In vivo original study, i.e. randomized controlled clinical trials, controlled clinical trials, prospective or retrospective case series,
-
2.
Study performed on humans,
-
3.
Study including at least 10 patients at follow-up,
-
4.
Use of dental CBCT,
-
5.
Comparative clinical (i.e. non-surgical or intra-surgical) and/or radiographic (i.e. two-dimensional X-ray images) measurements,
-
6.
Data on periodontal bone loss, i.e. furcation defects or vertical and/or horizontal bone loss, and
-
7.
Publication in English or German language.
Information sources and search
The electronic databases Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE via PubMed, Scopus and the grey literature (www.opengrey.eu) were searched for studies published by June 6, 2019. The search protocols within the different databases were applied and validated as identically as possible (Online Resource 2). The following search terms were applied: “periodontal diseases” OR “periodontitis” OR “periodont*” AND “furcation” OR “defect” OR “bone loss” AND “computed tomography” OR “digital volume tomography”.
Additionally, potentially relevant citations were harvested from the bibliographies of included studies and relevant reviews on the topic, and examined for inclusion eligibility. The references resulting from the searches were entered in EndNote (Version X9, Clarivate Analytics, Philadelphia, PA, USA), and duplicates were removed.
Study selection
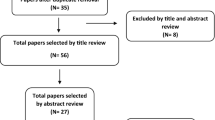
Screening of records was performed independently by three of the authors (S. M., C. A. R. and J. C. S.). A Cohen kappa score was calculated to assess interexaminer agreement [10]. Eligibility assessment was performed through title and abstract analysis and secondly through full-text analysis (Fig. 1, Online Resource 3). If necessary, authors were contacted for clarifications or unreported data. From all studies of potential relevance, full text was obtained for independent assessment by the reviewers. Any disagreement was resolved by discussion among the authors. The software system for recording decisions was Microsoft Excel (Version 16.16.14, Microsoft Corporation, Redmond, WA, USA).
Data collection process
The following data of included studies were collected in duplicate by two independent reviewers in data extraction files (Microsoft Word, Version 16.16.14, Microsoft Corporation, Redmond, WA, USA): study design and methodology, number and characteristics of participants, assessed parameters (FI, vertical and/or horizontal bone loss), methods of assessment (CBCT device and comparison, i.e. clinical and/or radiographic measures), results, i.e. agreement, accuracy and/or potential benefit of CBCT in comparison with conventional diagnostics (Tables 1, 2, 3, 4).
Summary measures and synthesis of results
The studies were grouped according to the pattern of periodontal bone loss (i.e. interfurcal (FI) or vertical and/or horizontal bone loss) and with regard to the comparison method applied (i.e. non-surgical, two-dimensional radiographic and/or intra-surgical measurements).
With respect to the primary outcomes, the percentages of concordance (CBCT = comparison method), overestimation (CBCT > comparison method) and underestimation (CBCT < comparison method) were presented for categorical parameters (e.g. furcation grade). In case of continuous variables (e.g. defect depth or width), the predominant result (concordance, overestimation or underestimation) was presented. Owing to the great heterogeneity of included studies, a pooling of data or statistical meta-analyses was not appropriate and therefore not conducted. Thus, a narrative synthesis of the primary and secondary outcomes was performed.
Quality assessment
The risk of bias of included case series was evaluated by the checklist from Moga et al. [11], including 18 items of the following topics: (a) study objective; (b) study population; (c) intervention and co-intervention; (d) outcome measure; (e) statistical analysis; and (f) results and conclusion (Online Resource 4). Considering the adequacy in the respective case series, the items were graded and the percentage of positively graded items was calculated (Online Resource 5).
Results
Study selection
A total of 1152 studies was identified by electronic and hand search (Fig. 1). After title and abstract screening (inter-examiner Cohen’s kappa score = 0.810), the full texts of 17 studies were assessed for possible inclusion (Online Resource 3). Finally, 19 case series published between 2009 and 2019 fulfilled the inclusion criteria and thus remained for analysis.
Summary of study characteristics
According to the two specific questions, the data were presented separately for either topic.
-
(a)
Furcation involvement
A total of 11 studies was included and summarized in Tables 1 and 2 [2, 3, 12,13,14,15,16,17,18,19,20].
Study design
All included case series were conducted in a single university centre. None of the studies reported funding by an industrial partner. Examiner calibration was reported in seven studies [2, 3, 12, 15,16,17, 19].
Population
The sample sizes varied from 11 to 83 patients. Three studies, analysing 12 or 14 patient records, referred in part to the same overlapping study population [2, 3, 12]. The total number of patients in the remaining studies was 224. The mean age of patients ranged from 38 to 59 years, and the age range was between 18 and 86 years. One study did not report the age of included patients [18]. Eight out of 11 studies stated the proportion of males and females, i.e. out of 198 patients, 99 were females and 99 were males.
The number of teeth was reported in nine out of 11 studies, and varied from 20 to 85 teeth. The studies investigated maxillary and/or mandibular molars. The tooth type was further specified in seven studies, comprising 70 first and 56 second maxillary molars as well as 27 first, 26 second and two third mandibular molars. All studies reported the number of furcation sites, ranging from 25 to 423 sites. Thus, a total of 1006 furcation entrances were examined. All but one study [16] stated the severity of FI: In eight studies, furcation grades II or III were predominant. In two studies, furcation grades 0 and I constituted the majority [13, 20].
Intervention
All examinations were performed using a CBCT device. Different CBCT systems and settings with various technical parameters were used in the included studies.
Comparison
For comparison, non-surgical periodontal probing was performed in seven out of 11 studies [2, 3, 13, 14, 16, 18, 20]. In one study, periapical radiographs were additionally used for comparison [14]. Three out of 11 studies conducted intra-surgical measurements using an endodontic file [19] or Nabers and periodontal probes [12, 15]. One study performed both non-surgical and intra-surgical examinations in addition to CBCT analysis [17].
Primary outcome: Agreement of CBCT compared with non-surgical and/or radiographic measurements
In five studies, FI was classified in furcation grades [2, 13, 14, 18, 20]. In maxillary molars, 18 to 27% of the clinical findings were confirmed in the CBCT, while 29 to 58% were overestimated (FI in CBCT < FI non-surgical) and 19 to 46% revealed an underestimation (FI in CBCT > FI non-surgical) [2, 13, 18]. The clinically based furcation grade III was confirmed in 100%, while the confirmation of furcation grades I or II was between 0 and 29%. In mandibular molars, 23 to 84% of the clinical findings were confirmed in the CBCT, while 0 to 58% were overestimated (FI in CBCT < FI non-surgical) and 16 to 20% underestimated (FI in CBCT > FI non-surgical) [13, 14]. One study pooled data from maxillary and mandibular first molars and found concordance of CBCT to clinical findings in 60% [20]. Pajnigara et al. [17] measured the furcation depth as a continuous parameter and showed an underestimation of clinical findings compared with CBCT data (FI in CBCT > FI non-surgical).
Primary outcome: Accuracy of CBCT compared with intra-surgical measurements
In two studies, FI was classified in furcation grades [12, 15]. Herein, maxillary teeth were investigated, and 82 to 84% of CBCT data were confirmed by intra-surgical findings. Concordance was high in teeth with furcation grades I to III (98 to 100%) and rather low in teeth with furcation grade 0 (31%) [12]. Three studies measured the furcation depth as a continuous variable, showing concordance between CBCT and clinical findings in two studies [17, 19] and an underestimation by CBCT in one study [15]. In two studies, the furcation width and height were additionally determined [15, 19].
Secondary outcome: Potential benefits of CBCT
For the analysis of any potential benefit of CBCT in decision making, treatment recommendations based on non-surgical clinical measurements and periapical radiographs with and without supplemental CBCT imaging were compared in one study [1, 2]. The analysis indicated more than one treatment option in most maxillary molars without CBCT, while an additional CBCT analysis facilitated a clear decision for further periodontal treatment in all teeth investigated. Discrepancies between the CBCT-based and the clinical therapeutic approaches amounted between 59 and 82% [2]. In one study, a cost–benefit analysis was performed [3]. This analysis indicated the potential for relevant cost and/or time reductions when a CBCT is performed for treatment planning of a maxillary molar.
-
(b)
Vertical and/or horizontal bone loss
A total of eight studies related to this research question was included and summarized in Tables 3 and 4 [21,22,23,24,25,26,27,28].
Study design
All included case series were conducted in a single university or specialist centre. None of the studies reported funding by an industrial partner. Examiner calibration was performed in three studies [21, 22, 27].
Population
Sample sizes ranged from 11 to 44 patients, while the total number of patients was 179. The average age of the patients was between 33 and 49 years, and the age range was between 22 and 66 years. Three studies provided neither a mean age nor an age range of included patients [23,24,25]. In five out of eight studies, the proportion of males and females was declared. Overall, 71 females and 70 males were investigated in these studies.
All but two studies [21, 24] reported the number of teeth examined, ranging from 30 to 116 teeth. A total of 317 teeth were included in these studies. The tooth type was specified in six out of eight studies, comprising 52 anterior teeth and 198 posterior teeth [23, 25, 26, 28] and further 18 single-rooted and 12 multi-rooted teeth [27]. Grimard et al. [21] included two defects in incisors, 17 defects in canines or premolars, and 16 defects in molars. The number of sites was provided in all studies and ranged from 35 to 180 sites. Thus, a total of 735 sites were analysed. Of these, 254 presented vertical defects and 149 horizontal bone loss. In 332 sites, the bone loss pattern was not further specified [25, 27].
Intervention
All measurements were performed using a CBCT device. The CBCT systems and settings, i.e. technical parameters, varied considerably between studies.
Comparison
For comparison, non-surgical periodontal probing using a periodontal probe was performed in one out of eight studies [27]. In two studies, CBCT images were compared with conventional periapical radiographs [22, 26]. None of the eight studies compared CBCT with a combination of non-surgical and two-dimensional radiographic measurements. Six out of eight studies performed intra-surgical measurements using an endodontic reamer [24] or a periodontal probe [21, 23, 27, 28]. One study did not report the instrument for intra-surgical measurements [25].
Primary outcome: Agreement of CBCT compared with non-surgical or radiographic measurements
CBCT compared with non-surgical measurements: The height of the alveolar crest, i.e. cemento-enamel junction (CEJ) to alveolar crest (AC), was measured as a continuous parameter and an overestimation of clinical findings compared with CBCT was shown [27].
CBCT compared with conventional periapical radiographs: While the height of the alveolar crest (CEJ to AC) was underestimated in the periapical images, the defect depth (CEJ to BD), the defect width (AC to AC) and the defect type (vertical versus horizontal defects) corresponded between both methods [22]. The number of identified defect walls was identical in 45%, while more defect walls were detected by CBCT in 37% of defects [26].
Primary outcome: Accuracy of CBCT compared with intra-surgical measurements
Various parameters were evaluated:
-
The height of the alveolar crest (CEJ to AC), classified in categories, was evaluated in one study [25]. Herein, 93% of CBCT data corresponded to clinical findings. Four studies compared the height of the alveolar crest as a continuous variable, showing concordance [21, 23, 24] or underestimation of CBCT [27].
-
The defect depth, i.e. CEJ to bottom of the defect (BD) or AC to BD, was evaluated in four studies. Of these, two studies showed concordance [23, 24] and two studies demonstrated an underestimation of CBCT [21, 28].
-
The defect fill (CEJ to BD before versus after regenerative surgery) and the defect resolution (AC to BD before versus after regenerative surgery) were calculated in one study [21]. The results showed concordance for both parameters.
-
The defect width, i.e. AC to AC, was calculated in one study, showing concordance between both methods [28].
-
The defect type (vertical versus horizontal defects) was determined in one study [24]. Herein, 100% accuracy by CBCT was shown.
Secondary outcome: Potential benefits of CBCT
In one study, treatment recommendations for teeth with vertical bone defects based on periapical radiographs compared with CBCT images were determined [26]. The analysis showed overall concordance between CBCT-based and conventional periapical radiographs in 64% of teeth, while concordance decreased to 43% when periodontal regeneration was selected. There were no studies investigating potential benefits of CBCT in terms of PROMS, e.g. cost or treatment time benefits, in assessing vertical and/or horizontal bone loss.
Quality assessment
The assessment of risk of bias of the included case series is illustrated in Online Resource 5 and was based on the checklist from Moga et al. [11]. Percentage of positively graded items relevant for quality assessment ranged from 53 to 87% in the included studies. No study fulfilled all items for control of bias, i.e. the risk of bias could not be completely minimized in the included case series.
Discussion
The present systematic review has attempted to identify the best available external evidence for the accuracy and the additional benefit of CBCT images in periodontology. A total of 12 new case series were identified with the updated search, leading to 19 papers finally included. The studies were grouped according to the pattern of periodontal bone loss, i.e. interfurcal (FI) or vertical and/or horizontal bone loss. Eleven studies evaluated CBCT images in furcation-involved teeth, and eight studies examined vertical and/or horizontal bone defects.
A high agreement (84%) between non-surgical clinical and CBCT measurements of advanced FI was found in mandibular molars [14], whereas confirmation of non-surgical measurements by CBCT was comparatively low in maxillary molars (up to 27%) [2, 13, 18] (Table 1).
When assessing horizontal bone loss (CEJ to AC) and/or the number of defect walls in vertical bony defects, discrepancies between non-surgical and/or conventional X-ray images and CBCT data were reported [22, 26, 27] (Table 3). There was a high level of accordance between periapical radiographs and CBCT in detecting defect type, defect width in the mesio-distal direction and defect depth [22].
The comparison between CBCT and intra-surgical measurements demonstrated a high diagnostic accuracy of CBCT in assessing FI [12, 15, 17, 19], as well as vertical and/or horizontal bone defects [21, 23,24,25] (Tables 2, 3, 4). However, an under- or overestimation of bone loss was seen in the studies included; in order to decrease such risks, the diagnostic measures available should be reasonably combined in order to state the most accurate diagnosis and to perform a reasonable treatment planning. In addition, data from five studies showed that CBCT images provided information on the residual attachment, root proximities and fusions, periapical lesions, combined periodontal-endodontic lesions, fenestrations, length of root trunk and/or the assessment of the second mesiobuccal root canal [2, 13,14,15, 18]. These parameters may influence tooth prognosis and treatment planning [2].
CBCT applies a higher radiation dose than conventional X-ray images, including periapical and panoramic radiographs [29]. Therefore, each time CBCT is used, the potential harm must be carefully weighed against the potential benefit according to the ALARA principles (as low as reasonably achievable) in each case [30, 31]. Three case series evaluated potential benefits of CBCT in terms of PROMS and/or treatment recommendations (Tables 1, 2, 3). Walter et al. [2] showed that treatment decisions for maxillary molars based on clinical and conventional radiographic examinations differed from those obtained from additional CBCT analyses. In addition, discrepancies in treatment decisions based on conventional radiographs instead of CBCT images were observed for teeth with vertical bone defects, in particular when periodontal regeneration was considered [26]. A reduction of costs and treatment time was reported by Walter et al. [3] when using CBCT for treatment planning of furcation-involved maxillary molars. However, no evidence is currently available with regard to data on PROMS, e.g. cost and treatment time benefits, and CBCT application in assessing vertical and/or horizontal bone defects.
Thus, the data from this systematic review have shown an increased evidence for the accuracy of detecting periodontal bone loss and potential benefits of CBCT imaging in terms of clinically relevant, tooth-specific information. Thus, the results update, confirm and complement the results of our previous systematic review [1]. However, some aspects of the included studies need to be discussed:
-
1.
The study populations differed with respect to the severity of periodontal bone loss. For example, two studies included primarily (i.e. 79% and 84%, respectively) furcation lesions classified as grade 0 or I [13, 20]. The clinical relevance of additional three-dimensional imaging is limited compared with more severe FI.
Similarly, the severity of vertical and horizontal bone defects varied, with mean values ranging from 3.14 to 8.90 mm for the defect depth and from 2.6 to 7.62 mm for the alveolar crest height. In the studies included, discrepancies between intra-surgical measurements and CBCT findings seemed to be more common in more advanced defects [27, 28].
-
2.
Different tooth types, e.g. maxillary and/or mandibular molars, and different tooth sites were investigated in the studies included. For example, Marinescu et al. [14] investigated exclusively buccal furcation sites in mandibular molars, while six studies examined buccal and oral furcations sites in maxillary molars [2, 12, 15, 16, 18, 20].
The value of additional information obtained from CBCT depends on the examined tooth type. In mandibular molars, information of the FI may already be obtained by two-dimensional imaging methods. In addition, the accuracy of intra-surgical measurements may depend on tooth- and site-specific parameters, such as root morphology, diameter of furcation entrance and root proximities. As oral sites may have reduced clinical accessibility, differences may exist between CBCT and periodontal probing. In this way, differences in agreement between different furcation sites, e.g. buccal versus mesiopalatal sites in maxillary molars, may be explained [12]. In addition, measuring buccal sites in mandibular molars may show stronger agreement between clinical and CBCT measurements compared with mesiopalatal and distopalatal sites in maxillary molars.
-
3.
The studies used different systems to describe the severity of interfurcal bone loss, i.e. classification systems [2, 12,13,14,15, 18, 20], measurements [15, 17, 19] or dichotomous assessment models [16]. Thus, a direct comparison between the studies is limited. This marked heterogeneity of the studies with regard to the measurement methods for periodontal bone loss and the outcome parameters makes a statistical meta-analysis impossible. The percentages of concordance, overestimation and underestimation were presented for each study. However, recently, a meta-analysis on CBCT and periodontal diagnostics was published [32]. Currently, there is no scientific consensus on the feasibility of a meta-analysis. Some authors and journal editors accept great heterogeneity among the studies and provide or just ask for a statistical analysis for heterogeneity (I2) [33]. In contrast, other authors do not accept a great heterogeneity and argue with respect to differences between biology/medicine and statistics/mathematics [34, 35]. In addition, there is no agreement regarding the number of studies necessary for a useful meta-analysis. Recently, a systematic review with a meta-analysis was published. The analysis included two studies [36]. However, in some cases, a synopsis of studies might be useful. A simple approach was recently suggested [37], i.e. vote counting or recently the more advanced weighted vote counting [37,38,39]. The latter one provides a proxy of the impact for each study within the analysis.
In contrast, studies assessing vertical bone defects preferred continuous variables measuring exact values. Herein, linear measurements between reference points such as the CEJ and the alveolar bone crest were common. However, the periodontal probe is limited as a measurement tool as values as small as 0.5 mm are measured whereas CBCT is capable of measuring values to the nearest 0.01 mm. In three studies, clinical recording was performed with a digital Vernier calliper with an accuracy of up to 0.2 mm which may be comparable the accuracy of CBCT measurement [19, 23, 24]. The different accuracy of CBCT and clinical measurements by a periodontal probe may explain discrepancies between both methods. For example, furcation height and depth, measured as continuous parameters, were underestimated by CBCT relative to the respective intra-surgical findings in one study [15]. However, the discrepancy was lower than the 0.5-mm minimum accuracy of periodontal probing and seems to be acceptable with regard to the clinical relevance.
-
4.
Different levels of expertise among the examiners could have influenced the outcomes. Some studies did not report whether the examiners were radiologists and/or examiners who performed clinical measurements were periodontists. However, precise detection of FI is a challenge even for experienced clinicians. In addition, examiners should be calibrated to measurements. In ten studies, calibration of examiners was reported [2, 3, 12, 15,16,17, 19, 21, 22, 27].
-
5.
Several studies excluded teeth with metal and amalgam restorations or metal crowns, and/or teeth with endodontic fillings [15, 17,18,19, 22, 25, 27, 28]. Metallic artefacts reduce image quality by beam-hardening artefacts, scatter effects and/or streak artefacts, and thus affect visibility and applicability of CBCT images for diagnosis and treatment planning [40].
-
6.
Within each study, the same CBCT unit and the same exposure parameters were used. However, CBCT units and the protocols for image acquisition, i.e. exposure parameters such as the field of view, voxel size, exposure time, mA and kV settings, rotation, slice distance and/or number of images per scan, differed between the 19 included studies. Different CBCT machines may have an impact on accuracy [41]. In addition, the exposure parameters may influence image quality to a varying extent, and thus may explain differences between studies. Some CBCT parameters may lead to higher or lower spatial resolution. Further research needs to address these issues with particular attention to measures for reduction of doses of radiation.
Conclusion
This updated review provides clearly an increased evidence for CBCT imaging in detecting interfurcal, vertical and horizontal bone loss. With respect to the teeth and sites analysed, the benefit of CBCT imaging varies and is particularly pronounced in maxillary molars. However, further clinical trials are still needed to determine the benefit of CBCT imaging for diagnosis and treatment planning in periodontology and to establish criteria that will help define the specific indications for the use of three-dimensional imaging in periodontology [1].
References
Walter C, Schmidt JC, Dula K, Sculean A (2016) Cone beam computed tomography (CBCT) for diagnosis and treatment planning in periodontology: a systematic review. Quintessence Int 47:25–37. https://doi.org/10.3290/j.qi.a34724
Walter C, Kaner D, Berndt DC, Weiger R, Zitzmann NU (2009) Three-dimensional imaging as a pre-operative tool in decision making for furcation surgery. J Clin Periodontol 36:250–257. https://doi.org/10.1111/j.1600-051X.2008.01367.x
Walter C, Weiger R, Dietrich T, Lang NP, Zitzmann NU (2012) Does three-dimensional imaging offer a financial benefit for treating maxillary molars with furcation involvement? A pilot clinical case series. Clin Oral Implants Res 23:351–358. https://doi.org/10.1111/j.1600-0501.2011.02330.x
https://www.ncbi.nlm.nih.gov/pubmed/ Accessed 24 January 2020
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, Group P-P (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4:1. https://doi.org/10.1186/2046-4053-4-1
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097. https://doi.org/10.1371/journal.pmed.1000097
Cumpston M, Chandler J (2019) Chapter IV: updating a review. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane handbook for systematic reviews of interventions version 6.0 (updated August 2019). Cochrane
Garner P, Hopewell S, Chandler J, MacLehose H, Akl EA, Beyene J, Chang S, Churchill R, Dearness K, Guyatt G, Lefebvre C, Liles B, Marshall R, Martínez García L, Mavergames C, Nasser M, Qaseem A, Sampson M, Soares-Weiser K, Takwoingi Y, Thabane L, Trivella M, Tugwell P, Welsh E, Wilson EC, Schünemann HJ (2016) When and how to update systematic review: consensus and checklist. BMJ 35:i3507
Miller SA, Forrest JL (2001) Enhancing your practice through evidence-based decision making: PICO, learning how to ask good questions. J Evid Based Dent Pract 1:136–141
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Moga C, Guo B, Schopflocher D, Harstall C (2012) Development of a quality appraisal tool for case series studies using a modified Delphi technique. http://www.ihe.ca/documents/Case%20series%20studies%20using%20a%20modified%20Delphi%20technique.pdf (accessed in august, 2019)
Walter C, Weiger R, Zitzmann NU (2010) Accuracy of three-dimensional imaging in assessing maxillary molar furcation involvement. J Clin Periodontol 37:436–441. https://doi.org/10.1111/j.1600-051X.2010.01556.x
Darby I, Sanelli M, Shan S, Silver J, Singh A, Soedjono M, Ngo L (2014) Comparison of clinical and cone beam computed tomography measurements to diagnose furcation involvement. Int J Dent Hyg 13:241–245. https://doi.org/10.1111/idh.12116
Marinescu AG, Boariu M, Rusu D, Stratul SI, Ogodescu A (2014) Reliability of CBCT as an assessment tool for mandibular molars furcation defects. Proc SPIE 8925, Fifth International Conference on Lasers in Medicine: Biotechnologies Integrated in Daily Medicine, 89250J (14 January 2014); https://doi.org/10.1117/122045782
Qiao J, Wang S, Duan J, Zhang Y, Qiu Y, Sun C, Liu D (2014) The accuracy of cone-beam computed tomography in assessing maxillary molar furcation involvement. J Clin Periodontol 41:269–274. https://doi.org/10.1111/jcpe.12150
Cimbaljevic MM, Spin-Neto RR, Miletic VJ, Jankovic SM, Aleksic Z, Nikolic-Jakoba NS (2015) Clinical and CBCT-based diagnosis of furcation involvement in patients with severe periodontitis. Quintessence Int 46:863–870. https://doi.org/10.3290/j.qi.a34702
Pajnigara N, Kolte A, Kolte R, Pajnigara N, Lathiya V (2016) Diagnostic accuracy of cone beam computed tomography in identification and postoperative evaluation of furcation defects. J Indian Soc Periodontol 20:386–390. https://doi.org/10.4103/0972-124X.192307
Zhu J, Ouyang XY (2016) Assessing maxillary molar furcation involvement by cone beam computed tomography. Chin J Dent Res 19:145–151. https://doi.org/10.3290/j.cjdr.a36679
Padmanabhan S, Dommy A, Guru SR, Joseph A (2017) Comparative evaluation of cone-beam computed tomography versus direct surgical measurements in the diagnosis of mandibular molar furcation involvement. Contemp Clin Dent 8:439–445. https://doi.org/10.4103/ccd.ccd_515_17
Zhang W, Foss K, Wang BY (2018) A retrospective study on molar furcation assessment via clinical detection, intraoral radiography and cone beam computed tomography. BMC Oral Health 18:75. https://doi.org/10.1186/s12903-018-0544-0
Grimard BA, Hoidal MJ, Mills MP, Mellonig JT, Nummikoski PV, Mealey BL (2009) Comparison of clinical, periapical radiograph, and cone-beam volume tomography measurement techniques for assessing bone level changes following regenerative periodontal therapy. J Periodontol 80:48–55. https://doi.org/10.1902/jop.2009.080289
de Faria Vasconcelos K, Evangelista KM, Rodrigues CD, Estrela C, de Sousa TO, Silva MA (2012) Detection of periodontal bone loss using cone beam CT and intraoral radiography. Dentomaxillofac Radiol 41:64–69. https://doi.org/10.1259/dmfr/13676777
Haghgoo JM, Shokri A, Khodadoustan A, Khoshhal M, Rabienejad N, Farhadian M (2014) Comparison the accuracy of the cone-beam computed tomography with digital direct intraoral radiography, in assessment of periodontal osseous lesions. Avicenna J Dent Res 6:e21952
Banodkar AB, Gaikwad RP, Gunjikar TU, Lobo TA (2015) Evaluation of accuracy of cone beam computed tomography for measurement of periodontal defects: a clinical study. J Indian Soc Periodontol 19:285–289. https://doi.org/10.4103/0972-124X.154176
Goodarzi Pour D, Romoozi E, Soleimani Shayesteh Y (2015) Accuracy of cone beam computed tomography for detection of bone loss. J Dent (Tehran) 12:513–523
Suphanantachat S, Tantikul K, Tamsailom S, Kosalagood P, Nisapakultorn K, Tavedhikul K (2017) Comparison of clinical values between cone beam computed tomography and conventional intraoral radiography in periodontal and infrabony defect assessment. Dentomaxillofac Radiol 46:20160461. https://doi.org/10.1259/dmfr.20160461
Yang J, Li X, Duan D, Bai L, Zhao L, Xu Y (2019) Cone-beam computed tomography performance in measuring periodontal bone loss. J Oral Sci 61:61–66. https://doi.org/10.2334/josnusd.17-0332
Li F, Jia PY, Ouyang XY (2015) Comparison of measurements on cone beam computed tomography for periodontal intrabony defect with intra-surgical measurements. Chin J Dent Res 18:171–176
Dula K, Benic G, Bornstein M, Walter C, Dagassan-Berndt D, Filippi A, Hicklin S, Jeger F, Luebbers H-T, Sculean A, Sequeira-Byron P, Zehnder M (2015) SADMFR guidelines for the use of cone-beam computed tomography / digital volume tomography. A consensus workshop organized by the Swiss Association of Dentomaxillofacial Radiology. Part II: Endodontics, Periodontology, Reconstructive Dentistry, pediatric dentistry. Swiss Dent J 125:945–953
Farman AG (2005) ALARA still applies. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 100:395–397. https://doi.org/10.1016/j.tripleo.2005.05.055
Sowby FD (1978) International Commission on Radiological Protection: 1978 Stockholm meeting. Radiology 129:533–535. https://doi.org/10.1148/129.2.533
Yusof NA, Noor E, Yusof MY (2020) The accuracy of linear measurements in cone beam computed tomography for assessing intrabony and furcation defects: a systematic review and meta-analysis. J Oral Res 8:527–539. https://doi.org/10.17126/joralres.2019.077
Herrera D, Matesanz P, Martin C, Oud V, Feres M, Teughels W (2020) Adjunctive effect of locally delivered antimicrobials in periodontitis therapy. A systematic review and meta-analysis. J Clin Periodontol. https://doi.org/10.1111/JCPE.13230
Schmidt JC, Sahrmann P, Weiger R, Schmidlin PR, Walter C (2013) Biologic width dimensions – a systematic review. J Clin Periodontol 40:493–504. https://doi.org/10.1111/jcpe.12078
Schmidt JC, Walter C, Amato M, Weiger R (2014) Treatment of periodontal-endodontic lesions – a systematic review. J Clin Periodontol 41:779–790. https://doi.org/10.1111/jcpe.12265
Salvi GE, Stähli A, Schmidt JC, Ramseier CA, Sculean A, Walter C (2020) Adjunctive laser or antimicrobial photodynamic therapy to non-surgical mechanical instrumentation in patients with untreated periodontitis. A systematic review and meta-analysis. J Clin Periodontol. https://doi.org/10.1111/jcpe.13236
Eggmann F, Connert T, Bühler J, Dagassan-Berndt D, Weiger R, Walter C (2017) Do periapical and periodontal pathologies affect Schneiderian membrane appearance? Systematic review of studies using cone-beam computed tomography. Clin Oral Investig 21:1611–1630. https://doi.org/10.1007/s00784-016-1944-7
Buset SL, Zitzmann NU, Weiger R, Walter C (2015) Non-surgical periodontal therapy supplemented with systemically administered azithromycin: a systematic review of RCTs. Clin Oral Investig 19:1763–1775. https://doi.org/10.1007/s00784-015-1499-z
Buset SL, Walter C, Friedmann A, Weiger R, Borgnakke WS, Zitzmann NU (2016) Are periodontal diseases really silent? A systematic review of their effect on quality of life. J Clin Periodontol 43:333–344. https://doi.org/10.1111/jcpe.12517
Schulze R, Heil U, Gross D, Bruellmann DD, Dranischnikow E, Schwanecke U, Schoemer E (2011) Artefacts in CBCT: a review. Dentomaxillofac Radiol 40:265–273. https://doi.org/10.1259/dmfr/30642039
Pauwels R, Faruangsaeng T, Charoenkarn T, Ngonphloy N, Panmekiate S (2015) Effect of exposure parameters and voxel size on bone structure analysis in CBCT. Dentomaxillofac Radiol 44:20150078. https://doi.org/10.1259/dmfr.20150078
Stovold E, Beecher D, Foxlee R, Noel-Storr A (2014) Study flow diagrams in Cochrane systematic review updates: an adapted PRISMA flow diagram. Syst Rev 3:54. https://doi.org/10.1186/2046-4053-3-54
Hamp SE, Nyman S, Lindhe J (1975) Periodontal treatment of multirooted teeth. Results after 5 years. J Clin Periodontol 2:126–135. https://doi.org/10.1111/j.1600-051x1975.tb01734.x
Funding
The study was self-funded by the authors and their institutions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Online Resource 1
PRISMA checklist. (DOC 65 kb)
Online Resource 2
Electronic search strategy for the databases PubMed, Scopus and The Cochrane Library. (DOCX 15 kb)
Online Resource 3
Studies excluded based on full-text analysis, and reasons for exclusion. (DOCX 16 kb)
Online Resource 4
Criteria for assessing the methodological and reporting quality of case series studies according to Moga et al. [11]. (DOCX 16 kb)
Online Resource 5
Quality assessment of included studies on accuracy of CBCT in FI (a) and in detecting vertical and horizontal bone loss (b) according to Moga et al. [11]. (DOCX 31 kb)
Rights and permissions
About this article
Cite this article
Walter, C., Schmidt, J.C., Rinne, C.A. et al. Cone beam computed tomography (CBCT) for diagnosis and treatment planning in periodontology: systematic review update. Clin Oral Invest 24, 2943–2958 (2020). https://doi.org/10.1007/s00784-020-03326-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-020-03326-0