Abstract
Objectives
This study used cone beam computed tomography (CBCT) images to comparatively evaluate the three-dimensional microstructural features of reconstructed bone bridge based on the bone harvesting site and the presence/absence of artificial bone material, as well as the features of regenerated bone tissue after bone harvesting from mandibular symphysis in secondary alveolar bone grafting (SABG) for patients with cleft lip, with or without cleft palate.
Materials and methods
Thirty-one patients were divided into three groups in which SABG was performed by autologous bone harvesting from iliac crest (IC), mandibular symphysis (MS), or MS combined with β-TCP granules (MS+TCP). The microstructural trabecular bone parameters (TBPs) and bone structure indexes (SIs) were analyzed using datasets of CBCT images taken before and after SABG.
Results
TBPs showed differences between IC and MS groups (P < 0.05), resulting in greater values of bone volume density (P < 0.05) and inferior value of TBPf (P = 0.070) in IC group compared with MS group. Using MS+TCP or filling β-TCP granules into donor site significantly improved reconstructed or regenerated BV/TV and Tb.Th (P < 0.05) compared with group without β-TCP.
Conclusions
Microstructural characteristics of reconstructed bone bridge were dependent on the donor site of bone harvesting; using an absorbable bone conductive material improved bone quality and increased bone volume density.
Clinical relevance
Application of β-TCP granules as a partial alternative with autologous bone from mandibular symphysis could obtain comparable outcomes in the microstructure of bone bridge to SABG with autologous iliac crest.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
For patients with cleft lip with or without cleft palate, it is critical to treat the remaining alveolar cleft after primary lip and palate have been repaired. Boyne and Sands [1] were the first to advocate the use of secondary alveolar bone grafting (SABG); this approach is now widely accepted and used to achieve morphological and functional improvements, including the eruption of impacted permanent teeth into newly formed bone bridges, as well as development of dental arch and occlusion.
Regarding surgical methods for SABG, autologous grafts, especially those involving harvest of iliac crest bone, constitute the current gold standard; mandibular symphysis is used to lower morbidity at donor sites [2,3,4]. In our institution, we routinely used autologous iliac crest bone for SABG until 2005. Subsequently, we used mandibular symphyseal bone to avoid morbidity in harvesting iliac crest bone; however, the amount of bone that can be harvested from mandibular symphysis in the early mixed dentition period is limited due to the embedded permanent dentition. Therefore, application of this approach is restricted. Beta-tricalcium phosphate (β-TCP), an osteoconductive material with biodegradable kinetics, has been successfully used in bone reconstruction. After orthodontic tooth movement to the graft space, results are comparable to those achieved by using autologous iliac crest in an animal model [5], as well as in patients with alveolar defects [6]; notably, donor site morbidity and other systemic side effects are minimal, suggesting the suitability of this approach for clinical use in SABG.
Regarding bone tissue engineering, there are critical interactions among osteogenic cellular components, scaffold supports for cell proliferation and migration, and regulatory signals that induce cellular differentiation [7]. In addition, the alveolar cleft is spatially surrounded by the cortical bone wall of the proximal and distal maxillary segments and the bony defects of the labionasal and palatal wall, such that filling with β-TCP granules alone is dimensionally unstable after graft surgery [8]. Therefore, we used β-TCP in combination with autologous bone from the mandibular symphysis in unilateral cleft patients; in these patients, the grafted space was covered with the cortical bone to ensure stability of the applied mixed cancellous bone and β-TCP. Our current procedure for SABG has provided clinically favorable results comparable with those of grafts achieved by using autologous bone harvested from iliac crest; however, the specific microstructural characteristics of the formed bone bridge in the alveolar defect, including differences with those produced by conventional methods with iliac crest bone, remain unknown.
To evaluate outcomes in SABG, dental radiographs have widely been used to assess the remodeling process regarding matured bone tissue of the grafted bone or alternative materials by measuring the height of the bone bridge with various grading systems [9, 10]. However, these radiographic images are unable to perform three-dimensional evaluations, such as labial–palatal width of the bone bridge and qualitative analyses of stereoscopic structures; notably, such aspects might influence subsequent tooth migration, eruption, and long-term prognosis. Recently, three-dimensional analysis using cone beam CT (CBCT) has been developed that enabled the use of a lower dose of radiation to measure the volume and thickness in any direction; thus, analysis can be performed regarding three-dimensional parameters of trabecular bone or a variety of structural indexes of bony tissue [11, 12], and can provide greater details regarding prognosis, including the eruption of embedded teeth [13, 14].
In the present study, we analyzed the microstructural parameters and degree of mineralization of the formed bone bridge using CBCT images in patients who underwent SABG. These data were used to comparatively evaluate the three-dimensional microstructural features of reconstructed bone bridge according to the bone harvesting site and the presence/absence of artificial bone material, as well as the microstructural features of regenerated bone tissue in the donor site after bone harvesting from mandibular symphysis for patients who exhibited cleft lip with or without cleft palate.
Material and methods
Patients
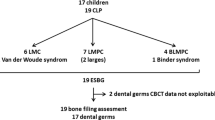
This study was based on the data obtained from a convenience sample of 31 patients with non-syndromic unilateral cleft lip and alveolus (UCLA) and cleft lip and palate (UCLP) treated at our institution between 2009 and 2013 (Fig. 1a). After providing an explanation of the study design and procedures to all parents, informed consent was obtained from them. The experimental protocol was approved by the Institutional Ethics Committee. Of the 31 patients, residual alveolar cleft was repaired with iliac crest bone in 9 (IC group), with mandibular symphysis in 8 (MS group), and with mandibular symphysis combined with micro-structured β-TCP granules in 14 (MS+TCP group, Fig. 1b). All the included patients had tooth germ of the canine, but not of the lateral incisor; the mean age at the time of SABG did not significantly differ among the groups (Fig. 1a, Table 1). Before the operation, orthodontic treatments (e.g., maxillary protraction, expansion of the maxillary arch, and alignment) were performed as necessary to ensure suitable recipient space for bone grafting. We assessed the radiographic scoring of canine root development prior to and 12 M after the surgery, and the reconstructed alveolar bone bridge resorption 12 M after surgery in all cases, using previously reported methods [15, 16].
Procedure of bone grafting
The surgical graft space preparations of the patients’ recipient sites were performed by a single experienced oral-maxillofacial surgeon, in accordance with a method published previously by Bergland et al. [10]. Briefly, the alveolar defect was exposed by an incision in the cleft margin; after preparation of the nasal lining, autologous cancellous bone was harvested from iliac crest or mandibular symphysis as a single entity for grafting. Alternatively, a mixture of materials was made comprising autologous cancellous bone from mandibular symphysis, β-TCP granules (0.5–3.0 mm; 75% microporous structured particles containing highly purified (> 99.9%) β-TCP; OSferionTM, Olympus Terumo Biomaterials, Tokyo, Japan) at a ratio of one to one were filled into the graft space. Then, the nasal lining and labial side wall were covered with cortex harvested from the mandibular symphysis. The graft space was then covered with reflected labial (and palatal) flaps; a periosteal releasing incision was used to ensure watertight closure and sufficient sliding of flaps. In some patients, β-TCP granules were used to fill the bony defect of the mandibular symphysis after bone harvesting.
Radiological examination and three-dimensional microstructure analyses of reconstructed bone
All the patients underwent CBCT before bone grafting as well as at 12 months after bone grafting. The Alphard-3030 (Asahi Roentgen, Kyoto, Japan) was used to perform CBCT scanning. CBCT images for all the included patients were obtained from infraorbital to mandible with the 10.2 × 10.2 cm field of view selection. The images were taken at 80 kVp and 4–5 mA with a scan time of 17 seconds, as well as voxel size of 0.2 × 0.2 × 0.2 mm. The datasets were exported in 16-bit DICOM file format.
For the assessment of microstructure of newly formed bone in alveolar defects and in defects of the mandibular symphysis after bone harvesting, CBCT images were reconstructed and analyzed by TRI/3D-BON software (RATOC System Engineering, Tokyo, Japan). To extract the regenerated bone tissue in alveolar clefts or the mandibular symphysis, reconstructed three-dimensional CBCT images taken prior to surgery and after surgery at different time periods were superimposed on facial bone by using landmarks in the infraorbital margin and piriform aperture for maxilla and inferior border of mandibular body and mental protuberance for mandible, respectively. The following measurement parameters were analyzed using the software in this study: bone volume fraction (BV/TV), trabecular thickness (Tb.Th), trabecular number (Tb.N), trabecular separation (Tb.Sp), trabecular bone pattern factor (TBPf), structure model index (SMI), and fractal dimension (FD). Tb.Th represents the averaged local thickness of trabecular bone, and Tb.Sp represents the local thickness of the marrow space between trabeculae. Tb.N can be evaluated as the inverse of the mean distance between the mid-axes of the trabecular bone. In this study, TBPf was used to evaluate convex or concave structure; values less than 0 indicated greater strength, similar to that of a honeycomb-like structure [17]. SMI was used to determine the plate- or rod-like geometry of trabecular structures; smaller values indicated that structures were increasingly plate-like [18]. Furthermore, FD was calculated as a slope value of the logarithm-fitted curve of inverse voxel size relative to the number of cubes needed to cover the bony structure [19].
Statistical analysis
Numeric results were expressed as means±standard error. Statistical analysis was performed using Prism (GraphPad Software, Inc., San Diego, CA). Kolmogorov-Sminov test was used to test the normality and the data followed distributions different than normal. Therefore, for all further statistical tests, nonparametric Mann-Whitney or Kruskal Wallis test were employed to compare mean values between the groups. Values of P < 0.05 were considered to be statistically significant.
Results
Table 1 summarizes the characteristics of patients in the present study. As shown, mean ages at the time of operation were similar among the IC, MS, and MS+TCP groups. In most cases, the root of the canine was developed approximately 1/2–3/4 (score 3–4) [15], with root formation progressing further after surgery. As described by Abyholm [16], radiographic outcome rating score, signifying the resorption of the reconstructed bone bridge, did not vary significantly among the groups.
Evaluation of the impact of bone harvesting site and bone substitute material on bone quality and biomechanical properties of the reconstructed bone bridge in alveolar defects
Figure 2 presents the results of IC, MS, and MS+TCP treatments. Comparisons of the microstructure of trabecular bone, according to donor bone harvesting site, demonstrated that Tb.Th and Tb.Sp showed smaller values, whereas Tb.N showed greater values in the IC group, relative to the MS group (Tb.Th: IC, 668 ± 54.4 μm, MS, 877 ± 55.4 μm, P = 0.014; Tb.Sp: IC, 596 ± 55.0 mm, MS, 1296 ± 503 mm, P = 0.001; Tb.N: IC, 0.72 ± 0.08/mm, MS, 0.15 ± 0.09/mm, P < 0.001). The results showed greater BV/TV values in the IC group than in the MS group, whereas TBPf in the IC group was inferior to that in the MS group (BV/TV: IC, 46.6 ± 6.53 mm3, MS, 30.5 ± 4.25 mm3, P = 0.046; TBPf: IC, 1.31 ± 0.52/mm, MS, 0.32 ± 0.08/mm, P = 0.070). Other structural indexes (SMI and FD) showed no significant differences between the two groups (SMI: IC, 2.11 ± 0.15, MS, 2.17 ± 0.18, P = 0.500; FD: IC, 2.08 ± 0.04, MS, 2.11 ± 0.05, P = 0.246). Conversely, in comparisons between MS and MS+TCP groups, all the trabecular bone parameters (TBPs; with the exception of Tb.Th) were improved in the MS+TCP group (Tb.Th, 1158 ± 68.8 μm, P = 0.009; Tb.Sp, 1063 ± 98.2 mm, P = 0.236; Tb.N, 0.15 ± 0.02/mm, P = 0.486); this increased BV/TV and TBPf in the MS+TCP group (BV/TV, 52.5 ± 6.04 mm3, P = 0.010; TBPf, − 0.26 ± 0.24/mm, P = 0.071), compared with those parameters in the MS group.
Biomechanical properties of a reconstructed bone bridge in an alveolar defect at 12 months post-operation. Comparative analyses of the microstructural characteristics of reconstructed alveolar bone bridges among the IC, MS, and MS+TCP groups related to volumetric bone mineral density (BV/TV, a), trabecular bone properties including Tb.Th (b), Tb.N (c), Tb.Sp (d), TBPf (e), and structural indexes, including SMI (f) and FD (g). All parameters are shown as mean ± standard error. Mann-Whitney test was used to evaluate statistical significance (*P < 0.05, IC vs MS, **P < 0.05, MS vs MS+TCP)
Comparative evaluation of bone quality and microstructural parameters of reconstructive bone bridge between patients with CLA and those with CLP
Next, we examined the differences in the structural parameters between the cleft lip and alveolus (CLA) and cleft lip and palate (CLP) groups. As shown in Fig. 3, there were no significant differences in any of the study parameters between the groups, upon treatment with autologous mandibular symphysis (MS) bone (Tb.Th: CLA group, 895 ± 99.2 μm, CLP group, MS, 858 ± 65.4 μm, P = 0.443 ; Tb.Sp: CLA group, 1398 ± 320 μm, CLP group, 1194 ± 195 μm, P = 0.441; TBPf: CLA group, 0.36 ± 0.13 /mm, CLP group, 0.27 ± 0.09/mm, P = 0.443). BV/TV and other structural parameters were also comparable between CLA and CLP groups (BV/TV: CLA group, 30.0 ± 8.81%, CLP group, 31.1 ± 2.52%, P = 0.343; TBPf: CLA group, 0.36 ± 0.13 /mm, CLP group, 0.27 ± 0.09/mm, P = 0.443; SMI: CLA group, 2.26 ± 0.30, CLP group, 1.93 ± 0.10, P = 0.486). Although not statistically significant, additional application of β-TCP granules as a partial alternative with mandibular symphysis (MS+TCP) showed trend to improve the mean values of Tb.Th, Tb.Sp, and TBPf in the CLA group, compared with the CLP group (Tb.Th: CLA group, 1249 ± 82.1 μm; CLP group, 1067 ± 105 μm, P = 0.083; Tb.Sp: CLA group, 970 ± 119 μm; CLP group, 1324 ± 215 μm, P = 0.191; TBPf: CLA group, − 0.66 ± 0.36 /mm; CLP group, 0.14 ± 0.24/mm, P = 0.083). Consistent with these findings, BV/TV and SMI also improved in the CLA group, compared to the CLP group (BV/TV: CLA group, 61.8 ± 9.16%; CLP group, 43.1 ± 6.71%, P = 0.083; SMI: CLA group, 1.58 ± 0.30; CLP group, 2.41 ± 0.24, P = 0.036).
Biomechanical characteristics of reconstructive bone bridge between patients with CLA and CLP. a–g MS and MS+TCP patients were subdivided into the CLA and CLP groups, and then, we evaluated the differences between MS and MS+TCP for each group with respect to the microstructural features assessed in Fig. 1. Mann-Whitney test was used to evaluate the statistical significance. All parameters are shown as mean ± standard error. *P < 0.05
Evaluation of the usefulness of β-TCP in the repair of mandibular symphysis donor sites
Figure 4 a shows a representative example of the radiographic healing process of donor and cleft sites, with or without augmentation synthetic bone materials (β-TCP), after bone harvesting from mandibular symphysis (TCP and non-TCP groups). As shown, use of β-TCP to fill the symphyseal defect area resulted in an esthetically pleasing lateral profile and facilitated bone regeneration at 12 months after the operation. The ratio of postsurgical values of labiolingual distance at the level of mental protuberance to the corresponding presurgical values showed favorable recovery upon filling with β-TCP (Fig. 4b). In addition, microstructural analyzes of regenerated bone in the harvested region revealed the superiority of both TBPs and bone structural indexes in the TCP group, compared with the non-TCP group (Table 2); this was consistent with the radiographic findings.
Evaluation of radiographic healing process with or without β-TCP augmentation in a donor site. a Representative radiographic images of healing process before and after SABG using autologous bone from mandibular symphysis with or without β-TCP. Each panel shows two-dimensional images by axial plane for cleft site and sagittal plane for donor site of cone beam computed tomography data, respectively. b The ratio of labiolingual distance on the repaired donor site in mandibular symphysis. Scores were measured as values relative to the baseline. All data are shown as mean ± standard error (n = 8) and were analyzed by Mann-Whitney test. *P < 0.001
Discussion
The spatial distribution of cortical and trabecular bone, including bone mineral density, is related to bone strength; it is clinically important to evaluate the ability to resist fracture in patients with osteoporosis [20, 21]. Non-invasive analysis techniques using three-dimensional imaging have been developed; these can provide information regarding skeletal fragility and bone quality, and may be useful for clinical management [20, 21].
In young healthy cleft patients, the repair of remaining alveolar defect with autologous bone frequently resulted in better bone bridging with eruption of an embedded permanent incisor; this was independent of the donor site. Remodeling parameters of static cortical bone are considerably different in the mandible and iliac crest [22]; moreover, little is known regarding whether those parameters can be altered in recipient sites after bone grafting. However, these trends suggest that autologous bone harvested from different sites can provide bone quality needed for SABG [2,3,4].
The present study demonstrated the following characteristics of remodeled autologous bone morphological microstructure, upon grafting into alveolar cleft: (1) microstructural characteristics of grafted bone differ between iliac crest bone and mandibular symphysis; (2) β-TCP, an osteoconductive calcium phosphate scaffold, could increase trabecular bone size when combined with autologous bone harvested from mandibular symphysis, relative to grafting with mandibular symphyseal bone alone; (3) use of β-TCP granules to fill the harvesting defects in the mandibular symphysis could facilitate bone regeneration with superior bone quality, compared to defects filled without resorbable calcium phosphate.
In our study, bone volume density, represented by BV/TV, was greater in the IC group than in the MS group; this suggested that SABG with iliac crest bone results in a greater increase in the spatial density of formed trabecular bone. A previous study investigated differences in static bone remodeling parameters in mandible and iliac crest bone; the relative number of osteons was much smaller, while osteonal diameter was larger in the mandible than in the iliac crest [22]. These characteristics were related to reduced cortical porosity and reduced activation frequency in the mandible, consistent with previous findings [22, 23].
In accordance with previous findings regarding site specificity of remodeling at different anatomic locations [22, 24], the present study showed increased trabecular thickness but reduced trabecular number and separation in the MS group compared with the IC group. These trends resulted in reduced bone volume density and lowered TBPf, which indicated improved formation of trabecular bone with a concave microstructure in the MS group. Interestingly, bone augmentation—using a highly porous β-TCP with transplantation of autologous bone from mandibular symphysis—significantly improved most parameters; trabecular thickness was increased and trabecular separation was reduced, which led to increased bone volume density, comparable to that observed in the IC group. Moreover, TBPf was lowered, indicating favorable trabecular bone quality. These results suggest that β-TCP could be a potent candidate for augmentation of bone substitute, producing functionally adequate bone volume in the graft space (comparable to that achieved by single autologous bone graft), as well as for improvement of bone volume density by increased trabecular bone quality.
In this study, we also investigated differences in microstructural features of the synthesized bone bridge according to the cleft type comprising the alveolar defect. In patients treated with mandibular symphysis bone, TBPs and structural indexes did not show significant differences between CLA and CLP groups. Although not statistically significant, the MS+TCP treatment resulted in greater improvement of bone quality and structural indexes in the CLA group relative to the CLP group. These differences might have been due to morphological differences in alveolar defects between CLA and CLP. Graft space in CLP has only bony wall on the lateral sides; moreover, the use of β-TCP is dimensionally unstable for condensing materials because of the free motion of the granules [8], although they are filled with mixtures that include autologous cancellous bone. To prevent potential morphological instability of β-TCP, a blend of carboxymethyl cellulose in glycerol has been used as a suitable binder formation, which allowed optimal surgical handling [25]. Although highly porous biomaterial particles may exhibit fragility due to excess pressure during application into bony defects [26], our results support the addition of dense filling components into the graft space to improve better bone quality after remodeling.
Autologous bone harvesting from the mandibular symphysis enables avoidance of surgical damage in the extraoral region, including visible cutaneous scarring [27]. Although local morbidity has been reported (e.g., tooth injury or dental pulp necrosis [28], as well as sensory disturbance of the mental nerve [29]), most of our patients showed no donor site morbidity; this finding was consistent with that of a previous report [30]. Notably, a residual defect after bone harvest is a distinct complication; a previous study showed that the curved shape of the symphysis cannot be morphologically restored to the preoperative level during the natural course of wound healing [31]. To avoid the deformity of the harvesting site in the mandibular symphysis, a recent report described the excellent regeneration properties of resorbable calcium phosphate ceramic for repairing chin bone harvesting defects in SABG [31]. In that study, regenerated symphysis at 12 months post-surgery was histologically healed with bone tissue resembling natural bone structure; most implanted materials were absorbed, except small remnants embedded within the bone [31]. The present study also showed better regeneration of the contoured shape of the symphysis by using β-TCP to fill the bony defect of the harvesting site. In addition, microstructural analysis of regenerated bone revealed improvement in TBPs, such that bone volume density, was improved in the β-TCP group, compared with that in the non-β-TCP group. These results also support the use of β-TCP as bone augmentation material in the regeneration of bone tissue, consistent with previous findings [8, 31].
The present study used CBCT to evaluate the microstructural parameters of regenerated bone in donor and recipient sites after alveolar bone grafting. Notably, regenerated trabecular bone microstructure showed different features based on the site of bone harvesting; application of β-TCP as augmentation material, with or without autologous bone, significantly enhanced bone volume density by improving TBPs. Moreover, it improved reconstruction of the shape of the mandibular symphysis after bone harvesting. Further investigation of long-term outcomes of macro- and microstructural features of grafted or synthesized bone after remodeling is necessary to understand the dimensional stability related to subsequent orthodontic tooth movement.
References
Boyne PJ, Sands NR (1972) Secondary bone grafting of residual alveolar and palatal clefts. J Oral Surg 30:87–92
Mikoya T, Inoue N, Matsuzawa Y, Totsuka Y, Kajii TS, Hirosawa T (2010) Monocortical mandibular bone grafting for reconstruction of alveolar cleft. Cleft Palate Craniofac J 47:454–468
Enemark H, Jensen J, Bosch C (2001) Mandibular bone graft material for reconstruction of alveolar cleft defects: long-term results. Cleft Palate Craniofac J 38:155–163
Koole R, Bosker H, van der Dussen FN (1989) Late secondary autogenous bone grafting in cleft patients comparing mandibular (ectomesenchymal) and iliac crest (mesenchymal) grafts. J Craniomaxillofac Surg 17(suppl 1):28–30
de Ruiter A, Meijer G, Dormaar T et al (2010) Beta-TCP versus autologous bone for repair of alveolar clefts in a goat model. Cleft Palate Craniofac J 48:654–662
de Ruiter A, Janssen N, van Es R, Frank M, Meijer G, Koole R, Rosenberg T (2015) Micro-structured beta-tricalcium phosphate for repair of the alveolar cleft in cleft lip and palate patients: pilot study. Cleft Palate Craniofac J 52(3):336–340
Murphy CM, O’Brien FJ, Little DG, Schindeler A (2013) Cell-scaffold interactions in the bone tissue engineering triad. Eur Cell Mater 26:120–132
Janssen NG, de Ruiter AP, van Hout WMMT, van Miegem V, Gawlitta D, Groot FB, Meijer GJ, Rosenberg AJWP, Koole R (2017) Microstructured β-tricalcium phosphate putty versus autologous bone for repair of alveolar clefts in a goat model. Cleft Palate Craniofac J 54(6):699–706
Kindelan JD, Nashed RR, Bromige MR (1997) Radiographic assessment of secondary autogenous alveolar bone grafting in cleft lip and palate patients. Cleft Palate Craniofac J 34(3):195–198
Bergland O, Semb G, Abyholm FE (1986) Elimination of the residual alveolar cleft by secondary bone grafting and subsequent orthodontic treatment. Cleft Palate J 23:175–205
Ibrahim N, Parsa A, Hassan B, van der Stelt P, Aartman IH, Wismeijer D (2014) Accuracy of trabecular bone microstructural measurement at planned dental implant sites using cone-beam CT datasets. Clinical oral implants research 25(8):941–945
Hsu JT, Wang SP, Huang HL, Chen YJ, Wu J, Tsai MT (2013) The assessment of trabecular bone parameters and cortical bone strength: a comparison of micro-CT and dental cone-beam CT. Journal of biomechanics 46(15):2611–2618
Oh TS, Park JS, Choi JW, Kwon SM, Koh KS (2016) Risk factor analysis of bone resorption following secondary alveolar bone grafting using three-dimensional computed tomography. J Plast Reconstr Aesthet Surg 69(4):487–492
Ozawa T, Omura S, Fukuyama E, Matsui Y, Torikai K, Fujita K (2007) Factors influencing secondary alveolar bone grafting in cleft lip and palate patients: Prospective analysis using CT image analyzer. Cleft Palate Craniofac J 44:286–291
El Deeb M, Messer LB, Lehnert MW, Hebda TW, Waite DE (1982) Canine eruption into grafted bone in maxillary alveolar cleft defects. Cleft Palate J 19(1):9–16
Abyholm FE, Bergland O, Semb G (1981) Secondary bone grafting of alveolar clefts. A surgical/orthodontic treatment enabling a non-prosthodontic rehabilitation in cleft lip and palate patients. Scand J Plast Reconstr Surg 15(2):127–140
Hahn M, Vogel M, Pompesius-Kempa M, Delling G (1992) Trabecular bone pattern factor- a new parameter for simple quantification of bone microarchitecture. Bone 13(4):327–330
Laib A, Kumer JL, Majumdar S, Lane NE (2001) The temporal changes of trabecular architecture in ovariectomized rats assessed by MicroCT. Osteoporos Int 12(11):936–941
Hua Y, Nackaerts O, Duyck J, Maes F, Jacobs R (2009) Bone quality assessment based on cone beam computed tomography imaging. Clin Oral Implants Res 20(8):767–771
Bouxsein ML, Seeman E (2009) Quantifying the material and structural determinants of bone strength. Best Pract Res Clin Rheumatol 23(6):741–753
Bouxsein ML (2008) Technology insight: noninvasive assessment of bone strength in osteoporosis. Nat Clin Pract Rheumatol 4(6):310–318
Verna C, Melsen B, Melsen F (1999) Differences in static cortical bone remodeling parameters in human mandible and iliac crest. Bone 25(5):577–583
von Wowern N, Melsen F (1979) Comparative bone morphometric analysis of mandibles and iliac crests. Scand J Dent Res 87:351–357
Podenphant J, Engel U (1987) Regional variations in histomorphometric bone dynamics from the skeleton of an osteoporotic woman. Calcif Tissue Int 40:184–188
Davison N, Yuan H, de Bruijn JD, Barrere-de Groot F (2012) In vivo performance of microstructured calcium phosphate formulated in novel water-free carriers. Acta Biomater 8:2759–2769
Jensen SS, Bornstein MM, Dard M, Bosshardt DD, Buser D (2009) Comparative study of biphasic calcium phosphates with different HA/TCP ratios in mandibular bone defects. A long-term histomorphometric study in minipigs. J Biomed Mater Res B Appl Biomater 90(1):171–181
Weibull L, Widmark G, Ivanoff CJ, Borg E, Rasmusson L (2009) Morbidity after chin bone harvesting—a retrospective long-term follow-up study. Clin Implant Dent Relat Res 11(2):149e157
Booij A, Raghoebar GM, Jansma J, Kalk WW, Vissink A (2005) Morbidity of chin bone transplants used for reconstructing alveolar defects in cleft patients. Cleft Palate Craniofac J 42:533e538
Raghoebar GM, Meijer GJ, Smeele LE (2007) Reconstruction of defects in the oral and maxillofacial region. A review of the various options for treatment. Ned Tijdschr Tandheelkd 114(1):47–53
Al-Ani O, Nambiar P, Ha KO, Ngeow WC (2013) Safe zone for bone harvesting from the interforaminal region of the mandible. Clin Oral Implants Res 100:115–121
de Ruiter A, Dik E, van Es R, van der Bilt A, Janssen N, Meijer G, Koole R, Rosenberg A (2014) Micro-structured calcium phosphate ceramic for donor site repair after harvesting chin bone for grafting alveolar clefts in children. J Craniomaxillofac Surg 42(5):460–468
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Approval from the Institutional Review Board of the Osaka University Dental Hospital, Osaka University Graduate School of Dentistry, was obtained for this study (H26-E47). All procedures performed in studies involving human participants were in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from parents of all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Miyagawa, K., Tanaka, S., Hiroishi, S. et al. Comparative evaluation of bone microstructure in alveolar cleft repair by cone beam CT: influence of different autologous donor sites and additional application of β-tricalcium phosphate. Clin Oral Invest 24, 2789–2797 (2020). https://doi.org/10.1007/s00784-019-03142-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-03142-1