Abstract
Objectives
The aim of this study was to compare the postoperative pain after root canal treatment using a carrier-based obturation system and two different sealers.
Materials and methods
In this prospective randomized clinical trial, 160 patients were selected. Patients with vital and devital teeth were randomized into four groups using a randomized block design with block sizes of 10 patients each. The groups were devital/vital teeth treated with iRoot SP sealer and devital/vital teeth treated with AH Plus sealer. Patients were prescribed ibuprofen, a 200-mg analgesic, if needed, and postoperative pain was recorded by visual analogue scale at 6, 12, 24, and 72 h after obturation. Pain score and frequency of tablet intake were recorded and statistically analyzed.
Results
Results showed that there was no significant difference between groups in the incidence of postoperative pain; however, iRoot SP sealer was associated with less analgesic intake compared to AH Plus sealer.
Conclusion
The use of different sealers did not significantly affect pain levels.
Clinical relevance
iRoot SP sealer was associated with less analgesic intake compared to AH Plus sealer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pain after root canal treatment is a common sensation, which may commence a few hours to days postoperatively. The reported prevalence varies widely, from 1.9% [1] to 82.9% [2]. Factors that may predispose patients to postoperative pain after single visit root canal treatment include pulp status, preoperative pain level, the number of root canals present, the choice of root canal sealer [3], and obturation technique [4].
Root canal obturation is a critical component of root canal therapy and provides an adequate seal for the root canal system. Several techniques have been recommended to achieve complete filling of root canals and lateral canals. The use of cold lateral condensation (LC) of gutta-percha (GP) is common among dental practitioners. However, the disadvantages of this method include inhomogeneity, increased risk of root canal fracture, and poor adaptation to the canal walls [5]. Recently, the use of thermoplasticized GP is becoming more prevalent. The use of an endodontic obturator consisting of a flexible plastic core carrier that is coated homogeneously with a layer of refined “alpha-phase” GP enables more rapid lateral and vertical compaction of the thermoplasticized GP and sealer [6]. However, rapid insertion of the thermoplasticized obturator may result in the extension of the sealer and GP beyond the working length (WL) and through the apical foramen, whereas slow insertion may cause underfilling [7]. The extrusion of filling material may cause postoperative pain, although evidence is currently lacking.
AH Plus (Dentsply, Maillefer, Ballaigues, Switzerland), a root canal sealer based on epoxy resin, is frequently used for comparison with other sealers because of its favorable physicochemical properties and adaptability to root canal walls [8]. Mineral trioxide aggregate (MTA)-like materials based on calcium silicate, such as bioceramics, have been introduced recently. iRoot SP (Innovative BioCeramix Inc., Vancouver, Canada), a radiopaque, insoluble MTA-like sealer composed of calcium silicate, calcium phosphate, calcium hydroxide, and zirconium oxide, has demonstrated excellent physical properties and biocompatibility [9]. Compared with AH Plus, iRoot SP has shown significantly greater area of dentinal tubule penetration and equivalent apical sealing [9]. However, given the risk of overextension, practitioners should be familiar with the characteristics of sealers used with carrier-based obturation techniques. Because, it was shown that iRoot SP sealer had favorable properties with respect to the biological responses of subcutaneous and bone tissues [10].
Many research studies focus on endodontic postoperative pain management [1, 2, 4, 11,12,13]. Alacam et al. [11] evaluated the incidence and type of postoperative pain in single visit endodontic therapy, when different root canal sealers were utilized. Demirci and Calıskan [12] compared pain after root canal treatments using carrier-based obturation and the cold LC technique. Graunaite et al. [13] investigated postoperative pain after root canal obturation using warm vertical condensation technique with GP point with resin-based sealer or a bioceramic-coated GP point with bioceramic sealer. To our knowledge, the effects of carrier-based obturation technique using different sealers on postoperative pain concerning filling overextension have not been examined yet. Thus, the aim of this randomized controlled clinical study was to compare the incidence, the intensity of post-obturation pain, and overextension of root canal filling following the use of two different sealers with a carrier-based obturation system in single-visit root canal treatment. The hypothesis of this study was that there would be a difference between post-obturation pain among groups.
Materials and methods
This in vivo study was a prospective, single-center, single-blind, parallel, randomized clinical trial. The Human Ethics Committee of Cukurova University, Adana, Turkey, approved the study protocol (no. 2015-44-18).
Patient selection and pre-treatment assessment
Study participants (n = 160) were adults (age 18–65 years) undergoing root canal treatment at Endodontic Department of Cukurova University Faculty of Dentistry between July 2015 and January 2016. Exclusion criteria were systemic and/or periodontal disease; allergy to local anesthetic agents and/or history of intolerance to non-steroidal anti-inflammatory drugs; requirement for antibiotic prophylaxis; previous endodontic therapy; periodontal bone loss (visualized radiographically) and/or open tooth apex; pregnancy or breastfeeding status; pacemaker use; and use of an analgesic, anti-inflammatory medication, or antibiotic in the 7 days prior to the beginning of treatment. Patients were fully informed about the treatment, postoperative care, follow-up examinations, possible complications, and treatment options before participating in the study. All study participants provided oral and written informed consent.
This study is a randomized block design study with two treatment factors at 2 levels both. With an effect size of 0.25 for factors and an effect size of 0.5 for interaction (analyzed from preliminary experiment, along with the data of preoperative pain in both groups) and at a 5% significance level with 80% power, 33 participants for each of 4 treatment combinations are needed. Finally, 40 participants in each group were selected for this study, allowing for lost to follow-up.
One tooth per patient (mandibular premolar or molar) was included in the study. All patients received endodontic treatment in single visits. Prior to treatment, the practitioner recorded the tooth type, pulp status (vital/devital), patient gender (female/male) and age, and preoperative pain intensity. Pulp vitality was assessed using an electric pulp tester (Analytic Technology Corp., Redmond, WA, USA) and verified by the presence or absence of root canal bleeding during endodontic access preparation. Patients received instruction in the use of the Huskisson [14] 10 cm visual analogue scale (VAS) to rate pain preoperatively (before local anesthesia administration) and postoperatively.
Randomization
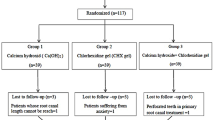
Patients were allocated to sealer groups (iRoot SP; Innovative BioCeramix Inc., AH Plus; Dentsply Maillefer, Ballaigues, Switzerland) using a randomized block design with blocks of 10 patients each. Allocation was concealed with a prespecified computer-generated randomization list. Number tables were prepared separately for vital and devital pulp. In each sealer group, 39 vital and devital teeth were included. The study groups consisted of devital teeth treated with iRoot SP sealer (ISP-D), vital teeth treated with iRoot SP sealer (ISP-V), devital teeth treated with AH Plus sealer (AHPlus-D), and vital teeth treated with AH Plus sealer (AHPlus-V). Table 1 shows demographic and clinical features of the population and the distribution of treated teeth according to sealer group. There were no partially vital teeth (in multirooted teeth) and 44 teeth had periapical lesion (21 ISP-D, 23 AHPlus-D).
Root canal procedures
An inferior alveolar nerve block was administered, and buccal infiltration with 2-mL articaine hydrochloride containing 1:200,000 adrenaline (Maxicaine; VEM Ilac, Istanbul, Turkey) was performed. None of the patients required further anesthetic use. The affected tooth was then isolated with a rubber dam. Endodontic access preparation was performed using sterile round diamond burs (Plus, Shenzen Dian Fong Abrasives Co. Ltd., Shenzhen, China). A dental operating microscope (Moller Spectra 500, Moller-Wedel GmbH, Wedel, Germany) was then used to locate the visible canal, and the WL was established with a #10 K file (VDW GmbH, Munich, Germany) and an electronic apex locator (Raypex 6; VDW GmbH). The WL was accepted when the apex locator displayed three green bars. WL was also determined radiographically, but the apex locator value was selected in cases of disagreement between values.
The glide path to the WL was created using G1 and G2 files (Micro-Mega, Besançon, France), and the root canal was then prepared using the One Shape system (Micro-Mega, Besançon, France) and VDW Silver motor (VDW GmbH) at a speed of 400 rpm and 2.5 N torque. For canals that passively accommodated a size-15 file, a One Shape ISO 25 tip and 6% taper file were used to complete root canal shaping. For larger canals, no. 30 and no. 37 (.06) files were used. During instrumentation, irrigation was performed with 10 mL 2.5% NaOCl using side-vented needles (NaviTips, 30 gauge; Ultradent Products, Inc., South Jordan, UT, USA). Final irrigation was performed with 5 mL 2.5% NaOCl, 5 mL 17% EDTA (EdiTac, Kemiger Nano Technologies, Ankara, Turkey), and 5 mL sterile saline. After the root canal had been dried, a verifier (Micro-Mega, Besançon, France) was placed into the canal in accordance with final file, and a radiograph was taken to control the adaptability. Teeth were obturated using the Herofill™ Soft-Core obturators (Micro-Mega, Besançon, France) with calibration of the carrier and adjustment of the obturator’s rubber stopper. The root canal was then coated with sealer (AH Plus or iRoot SP) up to the middle third using a suitable paper point. A second paper point was used to distribute the sealer, and a third was used to remove excess sealer, as described by Castelo et al. [15]. After heating for 35 s in an oven (HEROfill® Oven, Micro-Mega, Besancon, France), the operator inserted the obturator to the WL using firm apical pressure without rotation, while stabilizing the handle of the device with the index finger. The coronal GP was condensed around the carrier using a plugger until it hardened. After cooling, with a small round bur (Thermacut; Dentsply, Maillefer), the obturator handle and excess material were removed. The quality of root canal obturation was confirmed radiographically, and composite resin was then used for coronal restoration. Patients were given instructions on postoperative care and prescribed 200 mg ibuprofen (Advil, Catalent France Beinheim SA, France) when needed. One investigator was assigned to perform all of the clinical procedures (Ayfer Atav Ates).
Preoperative and postoperative pain rating
At the end of the treatment visit, patients were given a Huskisson VAS form to take home and requested to rate their pain at 6, 12, 24, and 72 h. Upon the return of completed forms, preoperative and postoperative pain scores (range 0–10) were recorded. Patients were also asked to record the quantity and timing (by hour) of ibuprofen use and to submit this information after 72 h.
Radiographic examination of root canal Obturation
Two experienced endodontists, who were blinded to the sealer used, individually examined root canal filling radiographs. The radiographs were prepared as a PowerPoint presentation (Microsoft® Corporation, Redmond, WA) and analyzed on a computer screen in a darkened room. In the evaluation of filling overextension, the GP and sealer could not be differentiated on the radiographs. Thus, the evaluators recorded only the presence or absence and extent of root canal filling overextension (0, no sealer or GP at the foramen; 1, sealer/GP at the foramen only; 2, sealer/GP extending beyond the foramen). For multirooted teeth, the number of overextruded root canals (1, one canal; 2, more than one canal) was recorded. In cases of examiner disagreement, a third experienced examiner was consulted.
Statistical analysis
All analyses were performed using IBM SPSS Statistics software (version 20.0; IBMCorp., Armonk, NY, USA). Categorical variables were expressed as numbers and percentages, and continuous variables were expressed as means with standard deviations or as medians with ranges. Categorical variables were compared among groups using the chi-squared test. Multiple group comparisons were performed using one-way analysis of variance (ANOVA) with the Bonferroni test. Repeated-measures ANOVA was used to evaluate changes in pain scores over time. For all tests, p < 0.05 was considered to be significant.
Results
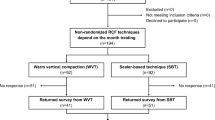
One patient was excluded from the study due to not attending to the recall visit and could not be reached. Three patients experienced flare-up and slight swelling, and they did not return the VAS forms. Thus, data from a total of 156 patients (89 women, 67 men) were included in the analyses (Fig. 1). Patient age differed significantly among groups (p = 0.002), but gender did not.
Pain intensity-analgesic intake
Table 2 shows the number of patients reporting pain at each time point according to group and intensity. In total, 53 patients obturated with AH Plus sealer (68%), 46 patients obturated with iRoot SP sealer (59%) perceived pain at 0–6 h period and decreased significantly over time in all groups (p < 0.001). Mean pain scores did not differ among groups at any time point (p > 0.05 for all; Table 3). However, when the groups were split AH Plus or iRoot SP and premolar or molar, there was a statistically significant difference between groups at 6–12-h interval. In this time period, premolars in iRoot SP group showed statistically less pain intensity than premolars in AH plus (p = 0.042). In this period, analgesic intake was not statistically different (iRoot SP group 8%-in AH Plus group 21%) in premolar teeth. In molar teeth, there was no statistically significant difference in pain intensity between sealer groups at any time period. But in molar teeth, analgesic intake was statistically higher at 6–12-h interval in AH Plus group than iRoot SP group (p = 0.014). Figure 2 shows mean plot of pain over time for groups.
Table 4 shows analgesic intake after root canal obturation at each time point. Seventy-two analgesics were used by 54 patients during the 72-h study period (6 h, 27.5%; 12 h, 14.1%; 24 h, 3.8%; 72 h, 0.6%). Completion of 72 h study period, 102 patients did not take analgesics (p = 0.011). Analgesic intake was significantly higher for patients with the vital teeth treated with AH Plus group compared to the other groups at 0–6 and 6–12 h periods (p < 0.05 for both). The risk of analgesic intake was 2.5-fold higher in the AH Plus groups than that of in the iRoot SP groups (OR = 2.5 and 95% CI 1.3–5.1).
Extrusion of root canal filling material
After obturation, 84 (54%) root canals showed slight extrusion of the filling into the apical or periapical area. Thirty-five (45%) root canals in the iRoot SP groups and 49 (63%) root canals in the AH Plus groups showed extrusion. The extrusion rate was highest in the AHPlus-D group, followed by the AHPlus-V, ISP-D, and ISP-V groups, but this difference was not statistically significant (Fig. 3). Furthermore, the extrusion rate did not differ between premolars and molars. There was no correlation between extrusion of root canal material-pain intensity and analgesic intake.
Discussion
Postoperative pain in endodontics reflects activation of the local inflammatory response in the periapical tissues [16], which is known to be associated with sealer composition and root canal obturation methods. In this study, the use of AH Plus or iRoot SP sealers did not significantly affect pain levels. In addition, Granuaite et al. [13] compared the same sealers with warm vertical condensation technique in patients with asymptomatic apical periodontitis and found no difference in the occurrence of postoperative pain. However, both premolar and molar teeth with vital and necrotic pulp were included in this study similar to some previous studies [17, 18] in order to reflect typical clinical conditions. In previous studies [17, 19], the incidence of post-endodontic treatment pain was higher in teeth with three or more canals, possibly due to the increased presence of potential periapical pain foci. In this study, when molar teeth were evaluated independently, there was not any difference in postoperative pain at any time period. The present study included teeth with vital and devital pulps, which were treated in single-visit root canal treatment, to see the possible effects of the presence of infected necrotic on postoperative pain. However, the incidence of postoperative pain during the 72-h study period did not differ among vital/devital groups and no correlation had been found between pulp status and postoperative pain. In accordance with our study, Ali et al. [20] reported that there was no correlation between the pulpal status and the postoperative pain when root canal treatment was performed in a single visit. Single-visit root canal treatment was preferred because this procedure was less time-consuming for the patients and the clinicians, which also avoids inter-appointment infection. Besides that, Wang et al. [21] demonstrated that post-filling pain levels did not differ between patients undergoing root canal treatments in single and multiple visits.
In this study, post-obturation pain was compared with baseline pain and pain at several time points during a 72-h period after a single-visit root canal treatment. Preoperative pain intensity did not differ among groups; however, the incidence and intensity of post-obturation pain decreased gradually over the study period in all groups.
The Huskisson VAS [14] was applied in this study because it is easier to use a numeric rating scale than to rate pain more broadly using categories such as “mild,” “moderate,” and “severe” by patients. The Huskisson VAS may take the form of a 5-, 10-, 15-, or 20-cm-long bounded line ranging from “no pain” to “maximum pain.” This scale has been found to be valid, reliable, and has been widely used in previous endodontic researches [22, 23]. Revill et al. [24] found that measurement error was related inversely to line length. We used a 10-cm scale in this study because it is significantly more accurate than a 5-cm scale. And also to avoid conflation of postoperative pain assessment, only one tooth per patient was treated in patients.
A carrier-based obturation system was used in this study to achieve increased GP density in the apical region, better flow into lateral canals, and fewer voids [25]. However, this technique has been associated with an increased risk of GP and sealer extrusion (25–100%) from the apical foramen in in vitro studies [12, 26, 27]. In the present study, extrusion rates ranged from 43 to 69%; they were thus lower than the rate reported by Tennert et al. [27] (80%) and higher than that reported by Demirci and Calıskan [12] (34%). In this study, more extrusion was detected in teeth treated with the AH Plus sealer but it was not statistically significantly more than iRoot SP sealer. This difference may be attributed to a difference in sealer flow. Qu et al. [28] recently demonstrated that warm vertical compaction decreased the flow rate of iRoot SP sealer. In this study, there was no correlation between extrusion, tooth type, and pulp status.
A laboratory study demonstrated that the likelihood of overfilling was associated with the canal tapering [29] and over instrumentation, which may cause post-treatment pain due to the extrusion of debris, sealer, or GP. In this study, root canal instrumentation was performed using the One Shape rotary system, because rotary instrumentation has been associated with significantly less debris extrusion than occurs with hand instrumentation and the use of reciprocating systems [30]. Great care was taken to determine the WL, a verifier of Herofill system that was placed into the canal before obturation and radiographs were taken to control adaptability.
The clinical implications of overfilling might induce undesirable pain and possible pooling of sealer in the apical portion of the canal. Riccuci et al. [31] showed that in cases of slight extrusion, the treatment outcome was not significantly affected by the type of sealer, and no correlation between sealer extrusion and postoperative pain was observed [32]. Similar to these findings, there was no correlation between extrusion and postoperative pain in our study.
Ibuprofen 200 mg was prescribed for postoperative pain, since higher dose may obscure the outcome especially with the low pain levels caused by endodontic treatment protocol in general [33]. Analgesic intake was higher at 0–24 h interval, which might be attributed to injection of local anesthetics, pressure from a rubber dam clamp, or discomfort due to prolonged mouth opening. iRoot SP groups took 2.5 times less analgesics than those in the AH Plus groups. The categories (being female, mandibular molar teeth, selection of AH Plus sealer) had a higher incidence of analgesic intake in this research (P < .05). When only molar teeth were evaluated, 46% of AH Plus group took analgesics, which was 25% in iRoot SP groups. Preoperative pain, pulpal status, and age did not affect analgesic intake. Females had taken 2.3 times more analgesic than males.
The differences in analgesic intake may be attributed to the greater biocompatibility and reduced cytotoxicity of bioceramic sealer compared with resin-based sealers [34]. The observed cytotoxicity of the sealers implied that their contact with the periapical tissues could provoke postoperative pain. There is an interference that the AH Plus group must have experienced more pain to have taken more analgesics and that the analgesics masked the perceived pain on the scale. It is the limitation of postoperative pain studies.
Postoperative pain associated with root canal treatment is a poor indicator of long-term success; however, the occurrence and the control of pain are of clinical interest. Future studies should be designed to determine the outcome of endodontic treatment with different sealers in the overfilled cases.
Conclusion
Although the use of different sealers did not significantly affect pain levels following root canal obturation, the iRoot SP sealer was associated with less analgesic intake than was the AH Plus sealer.
References
ElMubarak AHH, Abu-bakr NH, Ibrahim YE (2010) Postoperative pain in multiple-visit and single-visit root canal treatment. J Endod 36(1):36–39
Glassman G, Krasner P, Morse DR, Rankow H, Lang J, Furst ML (1989) A prospective randomized double-blind trial on efficacy of dexamethasone for endodontic interappointment pain in teeth with asymptomatic inflamed pulps. Oral Surg Oral Med Oral Pathol 67(1):96–100
Thakur S, Emil J, Paulaian B (2013) Evaluation of mineral trioxide aggregate as root canal sealer: a clinical study. J Conserv Dent 16:494–498
Alonso-Ezpeleta LO, Gasco-Garcia C, Castellanos-Cosano L, Martín-González J, López-Frías FJ, Segura-Egea JJ (2012) Postoperative pain after one-visit root-canal treatment on teeth with vital pulps: comparison of three different obturation technique. Med Oral Patol Oral Cir Bucal 17(4):721
Hale R, Gatti R, Glickman GN, Opperman LA (2012) Comparative analysis of carrier-based obturation and lateral compaction: a retrospective clinical outcomes study. Int J Dentistry 2012(3):954675
Goldberg F, Artaza LP, De Silvio A (2001) Effectiveness of different obturation techniques in the filling of simulated lateral canals. J Endod 27(5):362–364
Levitan ME, Himel VT, Luckey JB (2003) The effect of insertion rates on fill length and adaptation of a thermoplasticized gutta-percha technique. J Endod 29(8):505–508
Marin-Bauza GA, Rached-Junior FJA, Souza-Gabriel AE, Sousa-Neto MD, Miranda CES, Silva-Sousa YTC (2010) Physicochemical properties of methacrylate resin–based root canal sealers. J Endod 36(9):1531–1536
Zhang W, Li Z, Peng B (2009) Assessment of a new root canal sealer’s apical sealing ability. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 107(6):79–82
Zhang BP (2015) Tissue reactions after subcutaneous and intraosseous implantation of iRoot SP, MTA and AH Plus. Dent Mater J 34:774–780
Alacam T (1985) Incidence of postoperative pain following the use of different sealers in immediate root canal filling. J Endod 11(3):135–137
Demirci GK, Calıskan MK (2016) A prospective randomized comparative study of cold lateral condensation versus core/gutta-percha in teeth with periapical lesions. J Endod 42(2):206–210
Graunaite I, Skucaite N, Lodine G, Agentiene I, Machiulskiene V (2018) Effect of resin-based and bioceramic root canal sealers on postoperative pain: a split-mouth randomized controlled trial. J Endod 44(5):689–693
Huskisson E (1974) Measurement of pain. Lancet 304(7889):1127–1131
Castelo-Baz P, Martin-Biedma B, Lopes MM, Pires-Lopes L, Silveira J, López-Rosales E, Varela-Patino P (2013) Ultramicroscopic study of the interface and sealing ability of four root canal obturation methods: Resilon versus gutta-percha. Australian Endod J 39(3):159–163
Omoigui S (2007) The biochemical origin of pain: the origin of all pain is inflammation and the inflammatory response. Part 2 of 3—inflammatory profile of pain syndromes. Med Hypotheses 69:1169–1178
Arias A, la Macorra J, Hidalgo J, Azabal M (2013) Predictive models of pain following root canal treatment: a prospective clinical study. Int Endod J 46(8):784–793
Ince B, Ercan E, Dalli M, Dulgergil CT, Zorba YO, Colak H (2009) Incidence of postoperative pain after single-and multi-visit endodontic treatment in teeth with vital and non-vital pulp. European J Dent 3(4):273
Genet J, Hart A, Wesselink P, Thoden van Velzen S (1987) Preoperative and operative factors associated with pain after the first endodontic visit. Int Endod J 20(2):53–64
Ali A, Olivieri JG, Duran-Sindreu F, Abella F, Roig M, Garcia-Font M (2016) Influence of preoperative pain intensity on postoperative pain after root canal treatment: a prospective clinical study. J Dent 45:39–42
Wang C, Xu P, Ren L, Dong G, Ye L (2010) Comparison of post-obturation pain experience following one-visit and two-visit root canal treatment on teeth with vital pulps: a randomized controlled trial. Int Endod J 43(8):692–697
De Andrade Risso P, da Cunha AJ, de Araujo MC, Luiz RR (2009) Postoperative pain and associated factors in adolescent patients undergoing two-visit root canal therapy. Aust Endod J 35(2):89–92
Segura-Egea JJ, Cisneros-Cabello R, Llamas-Carreras JM, Velasco-Ortega E (2009) Pain associated with root canal treatment. Int Endod J 42(7):614–620
Revill S, Robinson J, Rosen M, Hogg M (1976) The reliability of a linear analogue for evaluating pain. Anaesthesia 31(9):1191–1198
Clinton K, Himel VT (2001) Comparison of a warm gutta-percha obturation technique and lateral condensation. J Endod 27(11):692–695
Da Silva D, Endal U, Reynaud A, Portenier I, Orstavik D, Haapasalo M (2002) A comparative study of lateral condensation, heat-softened gutta-percha, and a modified master cone heat-softened backfilling technique. Int Endod J 35:1005–1011
Tennert C, Jungbäck IL, Wrbas K-T (2013) Comparison between two thermoplastic root canal obturation techniques regarding extrusion of root canal filling—a retrospective in vivo study. Clin Oral Investig 17(2):449–454
Qu W, Bai W, Liang Y-H, Gao X-J (2016) Influence of warm vertical compaction technique on physical properties of root canal sealers. J Endod 42(12):1829–1833
Heeren TJ, Levitan ME (2012) Effect of canal preparation on fill length in straight root canals obturated with RealSeal 1 and Thermafil plus. J Endod 38(10):1380–1382
Kucukyilmaz E, Savas S, Saygili G, Uysal B (2015) Assessment of apically extruded debris and irrigant produced by different nickel-titanium instrument systems. Braz Oral Research 29(1):1–6
Ricucci D, Rocas IN, Alves FR, Loghin S, Siqueira JF Jr (2016) Apically extruded sealers: fate and influence on treatment outcome. J Endod 42:243–249
Sadaf D, Ahmad M (2014) Factors associated with postoperative pain in endodontic therapy. Int J Biomed Sci 10:243–247
Wells LK, Drum M, Nusstein J, Reader A, Beck M (2011) Efficacy of ibuprofen and ibuprofen/acetaminophen on postoperative pain in symptomatic patients with a pulpal diagnosis of necrosis. J Endod 37:1608–1612
Al-Haddad A, Che Ab Aziz ZA (2016) Bioceramic-based root canal sealers: a review. Int J Biomater 9753210
Acknowledgements
This Project was registered at www.clinicaltrial.gov (ClinicalTrials.gov Identifier: NCT03029520).
Authorship Declaration
We hereby certify that this study has been composed by us and is based on our own work, unless stated otherwise. No other person’s work has been used without due acknowledgement in this study. All references and verbatim extracts have been quoted, and all sources of information, including graphs and data sets, have been specifically acknowledged.
Funding
The work was supported by Scientific Research Projects Coordination Center of Cukurova University (Project no. TDH-2015-4949), Adana, Turkey.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Atav Ates, A., Dumani, A., Yoldas, O. et al. Post-obturation pain following the use of carrier-based system with AH Plus or iRoot SP sealers: a randomized controlled clinical trial. Clin Oral Invest 23, 3053–3061 (2019). https://doi.org/10.1007/s00784-018-2721-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-018-2721-6