Abstract
Objectives
Indirect CAD/CAM restorations can be fabricated using both subtractive and additive CAD/CAM technology. This study investigated the fracture load of crowns fabricated from three particle-filled composite CAD/CAM materials and one 3D-printed composite material.
Materials and methods
Lava Ultimate, Cerasmart and Brilliant Crios were used as particle-filled composite CAD/CAM material and els-3D Harz as 3D-printed composite material. For each group, crowns with three different material thicknesses (0.5/1.0/1.5 mm) were fabricated. Control group was composed of ceramic-based CAD/CAM materials e.max CAD and Enamic. Totally, n = 180 crowns were fabricated and adhesively seated on SLA fabricated dies. Thermomechanical loading and fracture testing were performed. The data for fracture loading force were statistically analyzed by two-way ANOVA followed with multiple comparisons by post hoc Tukey’s test (α = 0.05).
Results
In contrast to ceramics, all particle-filled composite crowns with 0.5-mm thickness survived fatigue testing. Forces varied statistically significantly. Brilliant Crios showed highest maximum loading force with 1580.4 ± 521.0 N (1.5 mm). Two-way ANOVA indicated that both the material and the thickness affected the fracture load (p < 0.05).
Conclusions
Particle-filled composite resin CAD/CAM materials may have advantageous material characteristics compared to ceramic CAD/CAM materials for minimal restoration thicknesses.
Clinical relevance
Composite-based CAD/CAM materials may offer new possibilities in minimally invasive restorative treatment concepts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Both ceramic and composite resin materials are used for the fabrication of indirect CAD/CAM (computer-aided-design/computer-aided-manufacturing) restorations. While esthetic characteristics have been reported to be superior for ceramics, composite-based materials may behave advantageously in terms of intraoral reparability [1,2,3]. Up-to-date, CAD/CAM composite materials are mostly available for subtractive fabrication procedures with a CAD/CAM milling machine in the form of industrially homogenously fabricated blocks. These blocks have been shown to have superior characteristics compared to direct composite materials [4, 5]. These materials are used for permanent single restorations. Composite-based CAD/CAM materials are composed of a composite resin polymer matrix and embedded ceramic-based filler particles. The composition and percentage of the relative compartment differs for the respective CAD/CAM materials and might be the main reason for the different material characteristics [2, 6, 7]. Composite-based CAD/CAM materials are often referred to as “particle-filled composites” because of their high filler percentage which is exemplarily reported to be 79% for Lava Ultimate (3 M ESPE; St Paul, MN, USA) and 71% for Cerasmart (GC Corporation; Tokyo, Japan). Up-to-date, only few 3D-printable composite materials are available for fixed, permanent single restorations. 3D-printable composite materials are additively built up layer-by-layer with a 3D printer typically using DLP (digital light processing) technology.
Few clinical studies are available for composite-based CAD/CAM materials, and most in vitro studies in terms of fatigue and fracture behavior only address veneer restorations [8,9,10,11,12,13]. However, there are no studies available investigating the fracture load of composite-based CAD/CAM materials as a function of different material thicknesses.
The aim of this study was to evaluate the fracture load of three particle-filled composite CAD/CAM materials and one 3D-printed composite as a function of different material thicknesses. The hypothesis was that there are no statistically significant differences for the fracture load of CAD/CAM-fabricated crowns made from different materials and thicknesses.
Materials and methods
The study comprised fatigue loading and subsequent fracture loading of adhesively seated single molar CAD/CAM crowns. Four composite CAD/CAM materials were investigated: LU = Lava Ultimate (3M ESPE; St. Paul, MN, USA), GC = Cerasmart (GC Corporation; Tokyo, Japan); BC = Brilliant Crios (Coltène AG; Altstätten, Switzerland); 3D = els-3D Harz (Saremco Dental AG; Rebstein, Switzerland). Control group was composed of two ceramic-based CAD/CAM materials: EC = lithium disilicate ceramic e.max CAD (Ivoclar Vivadent AG; Schaan, Liechtenstein); VE = hybrid ceramic VITA Enamic (VITA Zahnfabrik; Bad Säckingen, Germany). For each material, three different material thicknesses were investigated (0.5 mm, 1.0 mm, and 1.5 mm). For each group, n = 10 crowns were fabricated with a CAD/CAM system (CEREC Bluecam, CEREC MCXL milling unit) (Dentsply Sirona; York, PA, USA) (groups LU, GC, BC, EC, VE) respectively a 3D printing device (Freeform Pro 2, ASIGA; Anaheim Hills, CA, USA) (group 3D). In total 180 crowns were fabricated. Groups are shown in Table 1. Estimation of total sample size for the respective study setup with six test groups based on α = 0.05 significance level was performed by means of a power analysis with statistical power analysis program G*Power v3.1 (Open Source; HHU Düsseldorf) in respect of an estimated effect size of 0.3 and an observed power of 0.85.
All crowns were adhesively seated to methacrylate dies (n = 180) fabricated with stereolithography (SLA) technology (Viper Si2, 3D Systems; Rock Hill, SC, USA). Dies were designed with special CAD Software (Pro Engineer Wildfire 4.0, PTC; Needham, MA, USA). There were three different designs for each 0.5 mm, 1.0 mm, and 1.5 mm groups. Design for the dies was in accordance with the preparation guidelines for full-ceramic restorations. Z-axis solution was 100 μm for the base of the die and 50 μm for the body of the die. Material characteristics for the die material (inCoris SLS, infiniDent; Darmstadt, Germany) were as follows: E-Modulus 2.5 GPa, fracture strength 110–130 MPa, shore hardness 80–84 Shore D.
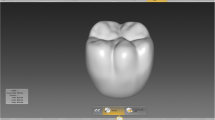
CAD design of single molar crowns for each group was done using CEREC software v.4.0 (Dentsply Sirona; York, PA, USA). CAD software tools “cursor details” and “show minimum thickness” were applied to ensure the respective thickness of the restoration for each group. Restoration for group 0.5 mm was designed manually. CAD design mode “biocopy” was used to transfer and adapt this design for groups 1.0 and 1.5 mm. For these means, a 0.5-mm crown was scanned with the intraoral scanning device CEREC Bluecam (Dentsply Sirona; York, PA, USA) after dusting with scanspray (VITA Powder Scan Spray, VITA Zahnfabrik; Bad Säckingen, Germany). For all restorations, the spacer parameter was set to 80 μm whereas all other parameters were set to 0 μm. CAM fabrication was performed with the 3 + 1 axis milling unit CEREC MCXL (Dentsply Sirona; York, PA, USA) equipped with cylinder pointed bur 12 S and step bur 12. Milling mode was set to “standard.” Milling instrument was renewed after milling one group respectively, i.e., after ten milling cycles to prevent damage of the restorations by used instruments. Printing of crowns for group 3D was performed with the DLP-based 3D printer Freeform Pro 2 (ASIGA; Anaheim Hills, CA, USA) after STL data file import into the software. Parameters were set to slice thickness 50 μm, exposure time 0.6 s, minimum/maximum light intensity 13.14 mW/cm2, z compensation 0 μm, xy compensation 0 μm. Crowns underwent different post-processing procedures after fabrication. Crowns of group EC were crystallized according to manufacturer’s recommendations (Programat CS, Ivoclar Vivadent AG; Schaan, Liechtenstein). Crowns of group 3D were first cleaned and washed in isopropanol 98% for 2 × 3 min using ultrasonic and then light cured with 4000 lighting exposures using Otoflash G171 device under nitrogen oxide gas atmosphere. No further manipulation was done to crowns of groups LU, BC, CE, VE. Die and restoration for thickness 0.5 mm is exemplarily shown in Fig. 1. Different cross-sections of restorations for 0.5 mm, 1.0 mm, and 1.5 mm restorations are shown in Fig. 2.
All crowns were adhesively seated to SLA-fabricated dies in accordance with a standardized protocol with a dual-polymerizing composite resin system (Variolink II high viscosity, Ivoclar Vivadent AG; Schaan, Liechtenstein). Application of an oxygen layer inhibitor material (Oxyguard, Kuraray Noritake; Tokyo, Japan) was performed. Polymerization of the luting composite resin was done with a polymerization lamp (Satelec MiniLED, KaVo Dental; Biberach, Germany) using 1600 mW/cm2 from the occlusal, mesial, distal, buccal, and lingual aspects for 60 s each. Preparations of dies and restorations prior to luting were carefully ensured following a standardized protocol. Dies were airborne-particle abraded with Si-coated aluminum oxide (Cojet, 3M ESPE; St. Paul, MN, USA) (diameter ≤ 50 μm, 200 kPa). Silanization of the dies was done with a silane for at least 60 s (Monobond Plus, Ivoclar Vivadent AG; Schaan, Liechtenstein). Bonding agent Heliobond (Ivoclar Vivadent AG; Schaan, Liechtenstein) was applied without light-curing. Restorations were cleaned with ultrasonic and degreased with ethanol. Restoration’s preparation for adhesive luting was in accordance with the respective manufacturer’s recommendations. Five percent HF acid etching was applied in group VE (60 s) and group EC (20 s). Restorations of groups LU, CE, BC, and 3D were airborne-particle abraded with aluminum oxide (diameter ≤ 50 μm, 200 kPa). Silanization with a silane (Monobond Plus; Ivoclar Vivadent AG; Schaan, Liechtenstein) for at least 60 s and application of a bonding agent (Heliobond; Ivoclar Vivadent AG; Schaan, Liechtenstein) was performed for all restorations.
After adhesive seating, crowns were prepared for fatigue testing and fracture loading. Restorations were centrally fixated in test blocks with a methacrylate (Paladur; Heraeus Kulzer; Hanau, Germany). Storage of crowns was done in distilled water at 37° in a heating cabinet. Thermomechanical loading was performed in respect to standardized protocol in a specially designed mastication device (1.2 million cycles, 1.7 Hz, invariable occlusal load 49 N ± 0.7 N, thermal cycling 5–55 degrees, dwell time 120 s, 12,000 cycles, water change time 10 s) [14]. The antagonist was the cusp of a natural molar. Load was applied to the central fissure. Examination of restorations for cracks was performed with a stereomicroscope at × 14 magnification with transmitted light after thermomechanical loading (Wild Leitz/M1B, Walter Products; Windsor, ON, Canada). If restorations showed failures such as cracks or chipping fractures, they were eliminated for further investigation. Surviving specimens were loaded until fracture in a universal testing machine (Allround Line z010; Zwick; Ulm, Germany) using a standardized protocol (crosshead speed 1 mm/min, ball diameter 5 mm). The maximum loading force to fracture values (N) were recorded automatically. The data for maximum loading force were statistically analyzed by two-way ANOVA followed with multiple comparisons by post hoc Tukey’s test (α = 0.05).
Results
Results for survival after fatigue testing and values for fracture loading are shown in Table 2. The maximum fracture loading forces significantly varied among the groups tested. There was a statistically significant two-way interaction between material and thickness F(8, 141) = 3.075, p = 0.003. Detailed statistical results after two-way ANOVA followed with multiple comparisons by post hoc Tukey’s test (α = 0.05) are shown in Table 3.
Compared to ceramic materials, all particle-filled composite crowns with 0.5-mm thickness survived fatigue testing. None of the crowns for group VITA Enamic (VE) and one crown for group e.max CAD (EC) with 0.5-mm thickness survived fatigue testing. One crown with thickness 1.0 mm in group CE, BC, and LU showed cracks after fatigue loading. For particle-filled composite materials group, Brilliant Crios (BC) showed highest mean loading force until fracture with a mean of 1580.4 N for group 1.5 mm. Mean loading force for Lava Ultimate (LU) restorations was highest with a mean of 1516.2 N for group 1.5 mm. Mean loading force for Cerasmart (CE) restorations was highest with a mean of 1251.1 N for group 1.5 mm. Mean loading force for 3D-printed materials els-3D Harz (3D) was highest with a mean of 1478.7 N for group 1.5 mm. No statistically significant differences were found among all four particle-filled composite resin CAD/CAM materials for all material thicknesses. VITA Enamic (VE) showed lowest mean loading force for ceramic-based materials with 729.1 N for group 1.0 mm.
Discussion
In this study, the fracture load of three particle-filled composite CAD/CAM materials (Lava Ultimate, Cerasmart, Brilliant Crios) and one 3D-printed composite (els-3D Harz) was investigated as a function of three different material thicknesses (0.5/1.0/1.5 mm). The control group was composed of two ceramic-based CAD/CAM materials (e.max CAD, Enamic). Molar crowns were fabricated either with a subtractive CAD/CAM system for groups LU, CE, BC, VE, and EC or an additive 3D printing system for group 3D. Crowns were adhesively luted to SLA-fabricated methacrylate dies. Thermomechanical loading and fracture testing were performed.
Statistically significant differences were found for the fracture loading force depending on the respective material used. Both the material and the thickness affected the fracture load (p < 0.05). None of the 0.5 mm ceramic crowns survived fatigue testing whereas all resin-based crowns survived. High fracture loading forces were found for the resin-based material Brilliant Crios (BC) showing the highest loading force with 1580.4 N (1.5 mm). Based on the results found in this study, the hypothesis that there are no statistically significant differences for the fracture load of CAD/CAM-fabricated crowns made from different materials and thicknesses has to be rejected. Results of this study must be discussed under various aspects.
It is important to emphasize the fact that when evaluating the fracture behavior of CAD/CAM materials, the whole study setup system comprised of the test material characteristics, the abutment design and its material characteristic, and the parameters for fatigue loading and fracture loading have to be considered [14,15,16,17]. The cement thickness has also been shown to influence the values for maximum occlusal loading of crowns [18]. Additionally, the material strengthening effect of adhesive bonding procedures has to be considered in due consideration of its varying effects on resin-based and ceramic-based CAD/CAM materials [19, 20]. Different study setup settings will result in different values found for the fracture force of CAD/CAM materials. In literature, there is the unanimity that the crown material and thickness are of primary importance when evaluating the relative contribution of the variables previously mentioned [21]. However, the E-Modulus of the supporting structure has been also shown to play an important role in flexural fracture [1]. The fracture load of all-ceramic crowns has been shown to be increased with the increase of the E-Modulus of the supporting material [22].
In this study, the E-Modulus of the die fabricated with SLA technology was 2.5 GPa and the E-Modulus of the luting resin was 8.3 GPa. The E-Modulus of human dentine is reported to be between 7 and 13 GPa [23]. The study setup thus represents a worst-case scenario for the respective CAD/CAM material and might undervalue the actual clinical material properties. Because of the high E-Modulus of the SLA fabricated abutment, the study setup represents a scenario that may tend to favor composite materials. It is thus important to emphasize that results found in this study cannot be transferred directly to in vivo conditions with a far more complex parameter setting. Human teeth or materials with a comparable E-Modulus might be preferable for in vitro fracture tests. Several studies have shown that fatigue loading simulating the wear mechanism and temperature changes within the oral environment are important when evaluating the fracture loading of dental materials [14, 24]. There are studies, questioning the clinical validity of in vitro tests due to the fact that clinical failure mechanisms can differ from the behavior observed in in vitro tests [25, 26]. However, in vitro test such as this study represents a first viable and valuable approach when considering the respective limitations of the study setup.
The choice of group’s material thickness has to be discussed as it is below the manufacturers’ recommendations for groups 0.5 and 1.0 mm. The reduction of restoration’s minimum thickness to 0.5 mm and 1.0 mm was performed to simulate clinical situations such as occlusal veneers or minimal-invasive crown preparations. Occlusal veneers represent a viable treatment approach for clinical cases of severe abrasion and erosion [27]. As tissue loss in severe erosion cases often includes all surfaces of the abutment teeth, minimal-invasive crowns instead of only occlusal covering restorations were chosen for the study setup. Minimally invasive restorations are clinically preferable as the conservation of tooth substance helps to preserve tooth vitality and to reduce postoperative sensitivity. Approximately 63 and 72% of coronal tooth structure has to be removed when teeth are prepared for all-ceramic and metal-ceramic crowns [28, 29]. Literature has shown that 2 mm or more of remaining dentine is a crucial threshold after preparation [30]. CAD/CAM materials that might persevere unnecessary tooth structure removal might be favorable for clinical application. Results of this study show that CAD/CAM materials might be suitable to fulfill these requirements. In this study, all composite-based restorations with thickness 0.5 mm have survived fatigue loading. Particle-filled composite CAD/CAM materials showed maximum loadings fracture values that are above the normal occlusal loading force for the posterior region.
In this study, three different abutment geometries have been fabricated from SLA material for 0.5 mm, 1.0 mm, and 1.5 mm CAD/CAM restorations. It is important to understand that geometries for the abutment dies were specifically designed by downsizing respectively by using specific CAD design tools to ensure a homogenous material thickness of the crowns. Parameters such as the cement layer thickness were also standardized by applying identical CAD design tools such as “set cement layer thickness” and the use of identical machining tools during the CAM process. All standardization methods applied for this study setup tended to homogenize results within one material group. However, it has to be mentioned that for the interpretation of results between different material groups, such as composite and ceramic, the consideration of the complex abutment-adhesive layer-restoration material is predominantly important as it will be discussed later on.
The choice of the CAD/CAM materials for the control groups has to be discussed. VITA Enamic represents a hybrid ceramic CAD/CAM material with a ceramic network infiltrated with a polymer matrix, and e.max CAD represents a lithium disilicate material. Both materials require HF acid etching prior to adhesive bonding and their indication range covers the same spectrum than for the particle-filled composite resin CAD/CAM materials. With an average flexural strength of 370 MPa for e.max CAD, the material is on the upper threshold of glass ceramic CAD/CAM materials currently available on the market [6].
Interpretation of results of this study has to be based on very specific knowledge on the material characteristics of the respective CAD/CAM materials. The microstructural composition of composite CAD/CAM materials is less favorable to risks of fractures that have been reported especially for ceramics. In literature, the typical ceramic risk factors have been identified as pores, side wall grinding damage, microstructural flaws, and inclusions [31]. Composite CAD/CAM materials have higher margin stability than ceramic materials [32]. Ceramic-based materials often show marginal chipping when not milled properly [33]. The edge chipping resistance of composite-based CAD/CAM materials has been found to be superior to ceramic-based materials [34, 35]. Composite-based CAD/CAM restorations might thus be favorable when milling thin margins and could be used also for non-prep clinical situations without the risk of marginal chipping during the fabrication procedure.
The effect of adhesive bonding on the fracture loading force of CAD/CAM restorations has to be discussed. Adhesive bonding of restorations has been shown to increase the fracture load values when compared to conventional luting [36,37,38]. For composite-based materials, the combination of bonding strength and resilient material characteristics has to be taken additionally into account. There are recent studies that have investigated the effect of elasticity on the stress distribution in dental crowns of ceramics and composite resin-based materials using finite element (FE) analysis [39]. Other studies are available, which demonstrate that the higher the E-Modulus of the restoration material, the lower the equivalent stress that occurred in the composite luting cement [40]. These findings suggest that restorations made of stiff materials are less prone to debonding than those made of composite resin [40]. There are also finite element analysis studies previously published, which support the thesis of high stress concentration as a possible factor for debonding [41]. Several studies are available investigating the bonding strength of composite-based CAD/CAM materials [42, 43]. Studies assessing the pretreatment method of restorations prior to adhesive luting suggest that the conditioning is predominantly important for composite-based CAD/CAM materials [44,45,46]. Strict observance of manufacturer’s recommendations for bonding procedure is thus highly mandatory when using composite-based CAD/CAM materials.
In this study, debonding events did not occur during the fatigue loading of CAD/CAM-fabricated composite crowns. In recent literature, a high number of clinical debonding events have been reported for one of the CAD/CAM composite materials tested in this study (LU) [47]. Fractographical analysis of specimens that had been adhesively luted to zirconia implant abutments revealed that debonding events might have been the reason for premature fractures of the restorations [48]. It is thus obvious that special attention has to be drawn to the complex abutment-adhesive layer-restoration material when discussing CAD/CAM materials in general and results of this study specifically. Even if CAD/CAM composite materials might appear advantageously in terms of reduced material thicknesses as demonstrated in this study, special attention has to be drawn to their adhesive bonding efficacy in terms of long-term clinical survival. Specific material characteristics of CAD/CAM composite materials such as elastic constants and flexural strength have been recently evaluated in detail emphasizing the specific damping effect of CAD/CAM composites [49, 50]. For CAD/CAM composite materials, crack propagation has been described to propagate through the resin matrix and matrix-particle interface with strengthening mechanisms as a result of crack deflection and the effect of bridging [51]. Effects of chemical and mechanical degradation have been recently analyzed for CAD/CAM composite materials revealing adverse characteristics compared to ceramics [52, 53]. The fact that CAD/CAM composite materials show both a higher resiliency, a higher water-up-take, and a higher thermal expansion compared to ceramic CAD/CAM materials is one essential point of the studies previously mentioned that might negatively influence the adhesive bonding efficiency of CAD/CAM composite materials and must be considered when evaluating results of this study. However, the role of the abutment material characteristics might be especially crucial for the evaluation of CAD/CAM composite materials. When the abutment complex shows hardly any resiliency, most of the deformation might occur within the CAD/CAM composite restoration because of its relatively low E-Modulus. The deformation might be thus transferred directly to the adhesive layer and might result in a higher number of debonding events. This observation might explain the high number of debonding events observed in the study of Schepke et al. with CAD/CAM composite restorations adhesively bonded to zirconia implant abutments [47]. In our study, a relatively low E-Modulus was chosen for the abutment material with only 2.5 GPa. It might be thus concluded that because of the resilient material characteristics of the abutment, the effect of debonding events might be underestimated as a result of lower stress exhibition on the adhesive layer interface during the fatigue loading. On the other hand, the high resiliency of the abutment might also explain the fact that brittle ceramics with only low flexural strength did not survive fatigue testing for ultrathin restorations in contrast to resilient CAD/CAM composite materials. When critically discussing results found in this study with focus on the respective study setup, it might be thus concluded that on the one hand, results found for CAD/CAM composites might be underestimated in terms of debonding events and overestimated in terms of fracture load force, and that on the other hand, results found for CAD/CAM ceramics might be underestimated in terms of fracture load force. Further studies are necessary to elucidate the specific role of the complex abutment-adhesive layer-restoration material more in detail.
Conclusion
Particle-filled composite resin CAD/CAM materials may have advantageous material characteristics for minimally invasive restorations allowing a more conservative approach in patient therapy.
References
Thompson VP, Rekow DE (2004) Dental ceramics and the molar crown testing ground. J Appl Oral Sci 12(spec):26–36
Ruse ND, Sadoun MJ (2014) Resin-composite blocks for dental CAD/CAM applications. J Dent Res 93:1232–1234
Spitznagel FA, Horvath SD, Guess PC, Blatz MB (2014) Resin bond to indirect composite and new ceramic/polymer materials: a review of the literature. J Esthet Restor Dent 26:382–393
Alharbi A, Ardu S, Bortolotto T, Krejci I (2017) Stain susceptibility of composite and ceramic CAD/CAM blocks versus direct resin composites with different resinous matrices. Odontology 105:162–169
Kamonwanon P, Hirose N, Yamaguchi S, Sasaki JI, Kitagawa H, Kitagawa R, Thaweboon S, Srikhirin T, Imazato S (2017) SiO2-nanocomposite film coating of CAD/CAM composite resin blocks improves surface hardness and reduces susceptibility to bacterial adhesion. Dent Mater J 36:88–94
Zimmermann M, Mehl A, Reich S (2013) New CAD/CAM materials and blocks for chairside procedures. Int J Comput Dent 16:173–181
Goujat A, Abouelleil H, Colon P, Jeannin C, Pradelle N, Seux D, Grosgogeat B (2018) Mechanical properties and internal fit of 4 CAD-CAM block materials. J Prosthet Dent 119:384–389
Zimmerman M, Koller C, Reymus M, Mehl A, Hickel R (2017) Clinical evaluation of indirect particle-filled composite resin CAD/CAM partial crowns after 24 months. J Prosthodont 27:694–699. https://doi.org/10.1111/jopr.12582
Shembish FA, Tong H, Kaizer M, Janal MN, Thompson VP, Opdam NJ, Zhang Y (2016) Fatigue resistance of CAD/CAM resin composite molar crowns. Dent Mater 32:499–509
Schlichting LH, Maia HP, Baratieri LN, Magne P (2011) Novel-design ultra-thin CAD/CAM composite resin and ceramic occlusal veneers for the treatment of severe dental erosion. J Prosthet Dent 105:217–226
Magne P, Schlichting LH, Maia HP, Barattieri LN (2010) In vitro fatigue resistance of CAD/CAM composite resin and ceramic posterior occlusal veneers. J Prosthet Dent 104:149–157
Magne P, Stanley K, Schlichting LH (2012) Modeling of ultrathin occlusal veneers. Dent Mater 28:777–782
El-Damanhoury HM, Haj-Ali RN, Platt JA (2015) Fracture resistance and microleakage of endocrowns utilizing three CAD-CAM blocks. Oper Dent 40:201–210
Krejci I, Reich T, Lutz F, Albertoni M (1990) An in vitro test procedure for evaluating dental restoration systems. 1. A computer-controlled mastication simulator. Schweiz Monatsschr Zahnmed 100:953–960
Scherrer SS, de Rijk WG (1992) The effect of crown length on the fracture resistance of posterior porcelain and glass-ceramic crowns. Int J Prosthodont 5:550–557
Rosentritt M, Plein T, Kolbeck C, Behr M, Handel G (2000) In vitro fracture force and marginal adaptation of ceramic crowns fixed on natural and artificial teeth. Int J Prosthodont 13:387–391
Guess PC, Schultheis S, Wolkewitz M, Zhang Y, Strub JR (2013) Influence of preparation design and ceramic thicknesses on fracture resistance and failure modes of premolar partial coverage restorations. J Prosthet Dent 110:264–273
May LG, Kelly JR, Bottino MA, Hill T (2012) Effects of cement thickness and bonding on the failure loads of CAD/CAM ceramic crowns: multi-physics FEA modeling and monotonic testing. Dent Mater 28:99–109
Sarabi N, Ghavamnasiri M, Forooghbakhsh A (2009) The influence of adhesive luting systems on bond strength and failure mode of an indirect micro ceramic resin-based composite veneer. J Contemp Dent Pract 10:33–40
D'Arcangelo C, De Angelis F, D’Amario M, Zazzeroni S, Ciampoli C, Caputi S (2009) The influence of luting systems on the microtensile bond strength of dentin to indirect resin-based composite and ceramic restorations. Oper Dent 34:328–336
Rekow ED, Harsono M, Janal M, Thompson VP, Zhang G (2006) Factorial analysis of variables influencing stress in all-ceramic crowns. Dent Mater 22:125–132
Scherrer SS, de Rijk WG (1993) The fracture resistance of all-ceramic crowns on supporting structures with different elastic moduli. Int J Prosthodont 6:462–467
Kinney JH, Marshall SJ, Marshall GW (2003) The mechanical properties of human dentin: a critical review and re-evaluation of the dental literature. Crit Rev Oral Biol Med 14:13–29
Yang R, Arola D, Han Z, Zhang X (2014) A comparison of the fracture resistance of three machinable ceramics after thermal and mechanical fatigue. J Prosthet Dent 112:878–885
Kelly JR (1995) Perspectives on strength. Dent Mater 11:103–110
Kelly JR (1999) Clinically relevant approach to failure testing of all-ceramic restorations. J Prosthet Dent 81:652–661
Al-Akhali M, Chaar MS, Elsayed A, Samran A, Kern M (2017) Fracture resistance of ceramic and polymer-based occlusal veneer restorations. J Mech Behav Biomed Mater 74:245–250
Edelhoff D, Sorensen JA (2002) Tooth structure removal associated with various preparation designs for anterior teeth. J Prosthet Dent 87:503–509
Edelhoff D, Sorensen JA (2002) Tooth structure removal associated with various preparation designs for posterior teeth. Int J Periodontics Restorative Dent 22:241–249
Davis GR, Tayeb RA, Seymour KG, Cherukara GP (2012) Quantification of residual dentine thickness following crown preparation. J Dent 40:571–576
Quinn GD, Hoffman K, Quinn JB (2012) Strength and fracture origins of a feldspathic porcelain. Dent Mater 28:502–511
Mörmann WH, Stawarczyk B, Ender A, Sener B, Attin T, Mehl A (2013) Wear characteristics of current aesthetic dental restorative CAD/CAM materials: two-body wear, gloss retention, roughness and martens hardness. J Mech Behav Biomed Mater 20:113–125
Kirsch C, Ender A, Attin T, Mehl A (2017) Trueness of four different milling procedures used in dental CAD/CAM systems. Clin Oral Investig 21(2):551–558
Argyrou R, Thompson GA, Cho SH, Berzins DW (2016) Edge chipping resistance and flexural strength of polymer infiltrated ceramic network and resin nanoceramic restorative materials. J Prosthet Dent 116:397–403
Quinn GD, Giuseppetti AA, Hoffman KH (2014) Chipping fracture resistance of dental CAD/CAM restorative materials: part I—procedures and results. Dent Mater 30:99–111
Mörmann WH, Bindl A, Lüthy H, Rathke A (1998) Effects of preparation and luting system on all-ceramic computer-generated crowns. Int J Prosthodont 11:333–339
Scherrer SS, de Rijk WG, Belser UC, Meyer JM (1994) Effect of cement film thickness on the fracture resistance of a machinable glass-ceramic. Dent Mater 10:172–177
Bindl A, Luthy H, Mörmann WH (2006) Strength and fracture pattern of monolithic CAD/CAM-generated posterior crowns. Dent Mater 22:29–36
Duan Y, Griggs JA (2015) Effect of elasticity on stress distribution in CAD/CAM dental crowns: glass ceramic vs. polymer-matrix composite. J Dent 43:742–749
Dejak B, Mlotkowski A, Langot C (2012) Three-dimensional finite element analysis of molars with thin-walled prosthetic crowns made of various materials. Dent Mater 28:433–441
Krejci I, Daher R (2017) Stress distribution difference between lava ultimate full crowns and IPS e.max CAD full crowns on a natural tooth and on tooth-shaped implant abutments. Odontology 105:254–256
Gilbert S, Keul C, Roos M, Edelhoff D, Stawarczyk B (2016) Bonding between CAD/CAM resin and resin composite cements dependent on bonding agents: three different in vitro test methods. Clin Oral Investig 20:227–236
Bähr N, Keul C, Edelhoff D, Eichberger M, Roos M, Gernet W, Stawarczyk B (2013) Effect of different adhesives combined with two resin composite cements on shear bond strength to polymeric CAD/CAM materials. Dent Mater J 32:492–501
Stawarczyk B, Krawczuk A, Ilie N (2015) Tensile bond strength of resin composite repair in vitro using different surface preparation conditionings to an aged CAD/CAM resin nanoceramic. Clin Oral Investig 19:299–308
Nobuaki A, Keiichi Y, Takashi S (2015) Effects of air abrasion with alumina or glass beads on surface characteristics of CAD/CAM composite materials and the bond strength of resin cements. J Appl Oral Sci 23:629–636
Lise DP, Van Ende A, De Munck J, Vieira L, Baratieri LN, Van Meerbeck B (2017) Microtensile bond strength of composite cement to novel CAD/CAM materials as a function of surface treatment and aging. Oper Dent 42:73–81
Schepke U, Meijer HJ, Vermeulen KM, Raghoebar CMS (2016) Clinical bonding of resin nano ceramic restorations to zirconia abutments: a case series within a randomized clinical trial. Clin Implant Dent Relat Res 18:984–992
Lohbauer U, Belli R, Cune MS, Schepke U (2017) Fractography of clinically fractured, implant-supported dental computer-aided design and computer-aided manufacturing crowns. SAGE Open Med Case Rep 5:2050313x17741015
Belli R, Wendler M, de Ligny D, Cicconi MR, Petschelt A, Peterlik H, Lohbauer U (2017) Chairside CAD/CAM materials. Part 1: measurement of elastic constants and microstructural characterization. Dent Mater 33:84–98
Wendler M, Belli R, Petschelt A, Mevec D, Harrer W, Lube T, Danzer R, Lohbauer U (2017) Chairside CAD/CAM materials. Part 2: flexural strength testing. Dent Mater 33:99–109
Shah MB, Ferracane JL, Kruzic JJ (2009) R-curve behavior and micromechanisms of fracture in resin based dental restorative composites. J Mech Behav Biomed Mater 2:502–511
Wendler M, Belli R, Valladares D, Petschelt A, Lohbauer U (2018) Chairside CAD/CAM materials. Part 3: cyclic fatigue parameters and lifetime predictions. Dent Mater 34:910–921
Blackburn C, Rask H, Awada A (2018) Mechanical properties of resin-ceramic CAD-CAM materials after accelerated aging. J Prosthet Dent 119:954–958
Funding
The work was supported by the Division of Computerized Restorative Dentistry, Center of Dental Medicine, University of Zurich.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Zimmermann, M., Ender, A., Egli, G. et al. Fracture load of CAD/CAM-fabricated and 3D-printed composite crowns as a function of material thickness. Clin Oral Invest 23, 2777–2784 (2019). https://doi.org/10.1007/s00784-018-2717-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-018-2717-2