Abstract
Objective
The study evaluated the longevity, effectiveness, safety, and impact on the oral health-related quality of life of in-office dental bleaching using low-concentration hydrogen peroxides.
Materials and methods
Randomized, parallel, and double-blinded clinical trial was performed with 54 participants using 6% or 15% hydrogen peroxide (HP) in-office bleaching activated via hybrid LED/laser light. Tooth color was evaluated at baseline (T1), 1 week of bleaching (T2), 2 weeks of bleaching (T3) and 1 week (T4) and 6 months (T5) after finishing the bleaching using the Classical Vita™ scale and spectrophotometer. Tooth sensitivity and gingival irritation were measured with Visual Numeric Scale and Modified Gingival Index. The impact on quality of life was evaluated using the Oral Impact on Daily Performance. The data were analyzed using the Friedman, Mann-Whitney, and McNemar tests (p < 0.05).
Results
The group HP15% presented significant color change (ΔE) from T1 to T4 (p = 0.002) and T1 to T5 (p < 0.001). Parameters L, a*, and b* differed significantly at T3, T4, and T5 compared T1 for both groups. At 6-month follow-up, 57.1% of HP6 and 43.7% of HP15% participants migrated from B1 to a darker color. No significant differences were observed between the groups in tooth sensitivity, gingival irritation, or impact on quality of life.
Conclusions
Both agents showed bleaching effectiveness, but HP15% presented greater color stability than HP6%, at 6-month follow-up. The agents showed low levels of tooth sensitivity, gingival irritation, and did not affect the oral health-related quality of life of the participants.
Clinical relevance
Despite the greater presence of sensitivity during treatment compared with 6% hydrogen peroxide, 15% hydrogen peroxide demonstrated better bleaching effectiveness, and greater color stability at the end of bleaching and at 6-month follow-up. The use of 15% hydrogen peroxide presents more suitable results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bleaching techniques are effective but the results vary by dental staining, patient age, the concentration of the active agent and the time and frequency of treatment [1]. In-office bleaching has traditionally been performed with high concentrations of hydrogen peroxide (HP), usually varying from 35 to 40% [2, 3]. However, the American Dental Association (ADA) [1] considers products with concentrations of up to 3.5% hydrogen peroxide as safe to use, whereas the Scientific Committee on Consumer Products (SCCP) [4] of the European Union approves of products with up to 6.0% hydrogen peroxide. Higher concentrations of peroxides result in more adverse effects, such as sensitivity and gingival irritation [5].
The amount and concentration of peroxide applied during in-office bleaching can alter the potential for harm [1]. Dental sensitivity during and after bleaching has been associated with microscopic surface defects and enamel pores that allow rapid entry of the bleaching agent into the pulp, resulting in sensitivity [6,7,8]. Hydrogen peroxide has irritant and cytotoxic potential [9,10,11]. Clinical studies have reported a higher prevalence of gingival irritation in patients who used bleaching materials with higher concentrations of peroxide [1, 12]. Hydrogen peroxide concentrations of 10% or more are potentially corrosive to the mucous membranes and skin [4].
To improve the safety of bleaching, some manufacturers have released low- concentration bleaching gels (6–20%) for in-office use; although these gels minimize tooth sensitivity, unfortunately, they do not achieve the same bleaching efficacy as high-concentration agents [13]. The TiO_N semiconductor agent (nanoparticles of titanium dioxide doped with nitrogen) was combined with the products of low concentrations (3.5–15%) of hydrogen peroxide to increase the safety and efficacy of bleaching compared with conventional formulations [14]. Although these agents increased the effectiveness of bleaching, they did not reach the same levels as the high-concentration (35 e 38%) agents did [14,15,16]. The biocompatibility and safety of low-concentration agents should be considered compared with those of conventional agents when choosing a bleaching agent that could have adverse effects on patients’ lives [14].
Previous studies have compared effectiveness and safety of low-concentration agents (6–15%) with those of conventional bleaching agents (35–38%) [14,15,16,17,18,19,20]. Considering the indications of the ADA [1] and the SCCP [4] regarding the use of products with hydrogen peroxide concentrations of up to 6%, few studies have compared low-concentration bleaching agents in terms of their effectiveness, safety or effects on oral health-related quality of life (OHRQL). The objective of this study was to evaluate the longevity, effectiveness, safety, and impact on the OHRQL of patients given in-office dental bleaching with concentrations of 6% and 15% hydrogen peroxide catalyzed with titanium dioxide nanoparticles and activated via hybrid light. This randomized clinical trial tested the null hypotheses that there are no differences between in-office dental bleaching using 6% and 15% hydrogen peroxide catalyzed with titanium dioxide nanoparticles and activated via hybrid light, considering the outcomes: longevity, effectiveness, safety, and impact on the OHRQL.
Materials and methods
This randomized, parallel, and double-blinded clinical trial evaluated the longevity, effectiveness, tooth sensitivity, and gingival irritation associated with low-concentration hydrogen peroxides in-office bleaching as well as its impact on OHRQL. This study followed the ethical principles established in the Helsinki Declaration of 1964, and was approved by the University Ethics Committee (Process no. 1.269.466). The study was registered as clinical trial (NCT02816593-https://clinicaltrials.gov/ct2/results?term=NCT02816593&Search=Pesquisa) and reported in accordance with the CONSORT Statement (Consolidated Standards of Reporting Trials) [21].
The examiners and the participants were blind to the concentrations of the bleaching agents. Individuals were invited to participate and those who agreed signed an informed consent document. The participants received tooth bleaching on upper and lower dental arches from the right second premolar to the left second premolar. The evaluation times were defined as follows: baseline (T1), 1 week after the beginning of bleaching (T2), 2 weeks after the beginning of bleaching (T3) and 1 week (T4) and 6 months (T5) after finishing the bleaching. The participants were assessed for color change from T1 to T5, tooth sensitivity and gingival irritation from T1 to T4. The impact of tooth bleaching on the individual daily lives was measured using the Oral Impact on Daily Performance (OIDP) instrument for both groups at T1 and T4.
Sample size
Two sample calculations were performed for the major dependent variables: bleaching effectiveness and oral health-related quality of life. Considering the clinically relevant difference between the bleaching techniques effectiveness (ΔE = 3.1), standard deviation of 3.71 [16] 95% confidence level and 80% power, a sample estimation was performed. Using oral health-related quality of life as the dependent variable, the calculation considered 41.76% bleaching effect ratio [22], 95% confidence level, 80% power, and 14.5% expected effect ratio. The minimum sample size required in both calculations was 22 participants per group. To offset possible losses, 20% was added to the sample, resulting in a total of 27 participants per group and 54 participants in total.
Recruitment
Sixty-nine individuals who were interested in participating in the research as advertised through posters on the university campus were recruited. All evaluations and procedures were conducted at the dentistry faculty clinics. We included 54 men and women between 18 and 40 years of age. The inclusion criteria were as follows: good general health status and an absence of systemic diseases; dental color ranging from A1 to darker assessed by the Classical Vita™ Scale; teeth without blemishes or restorations in the region of bleaching; and no previous bleaching treatment. Individuals with severe dental crowding, severe tooth sensitivity, pregnant, and smokers were not included.
Randomization and blinding
Individuals who met the eligibility criteria were selected and allocated into two groups. Randomization was performed using 54 sealed envelopes that were sequentially numbered, such that 27 envelopes had the 6% hydrogen peroxide (HP6%) and 27 had the 15% hydrogen peroxide (HP15%).
During the experiment, a blinded investigator in one room evaluated the patients with regard to color, tooth sensitivity, and gingival irritation and administered the questionnaire to assess the oral health-related quality of life. An operator in a second room independently performed the bleaching procedures without showing the concentration of bleaching agent to the participants.
Bleaching protocol
A gingival barrier (Lase protect, DMC Equipment, São Carlos, SP, Brazil) was applied and light cured (10 s). Three applications (10 min each) of bleaching agents per consultation were made, for a total of three consultations, with 7-day intervals among them [23]. Group HP6% used 6% hydrogen peroxide gel (Lase Peroxide Lite DMC Equipment, São Carlos, SP, Brazil), whereas Group HP15% used 15% hydrogen peroxide (Lase Peroxide Lite DMC Equipment, São Carlos, SP, Brazil). The bleaching agents were activated via hybrid LED/laser light (Whitening Laser II DMC Equipment, São Carlos, SP, Brazil) consisting of 6 LED (470 nm/blue light; Power = 1800 mW), and 3 low-intensity lasers (808 nm/infrared light; Power = 600 mW) with total area of irradiation = 8.5 cm2 and power density = 300 mW/cm2. In each bleaching session, the gel was irradiated with 5 cycles of 1 min per arch, alternating in both arches for 10 min.
Color evaluation
Tooth color was evaluated before, during, and after bleaching using the Classical Vita™ Scale (Vita-Zahnfabrik, Bad Säckingen, Baden-Württemberg, Germany) and Vita™ Easy Shade spectrophotometer (Easy Shade Advance™ Wilcos, Petrópolis, RJ, Brazil).
Subjective evaluation
A trained examiner calibrated and certified by the Toothguide Trainer Web (870 points of the 1000 evaluated) performed the visual evaluation using the Classical Vita™ Scale (Vita-Zahnfabrik, Bad Säckingen, Baden-Württemberg, Germany) positioned on the middle third of the teeth. The subjective color evaluations were made on upper and lower dental arches from the right second premolar to the left second premolar. Color evaluations were made under the same conditions of artificial light obtained with the Rite-Lite 2 light standardizer (Rite-Lite 2®, Addent, Danbury, CT, USA). The 16-color guide tabs were arranged from highest (B1) to lowest (C4) value, and each tab was given an ordered number from 1 to 16. The total color was the most frequent color of the evaluated teeth, and the worst situation was chosen in the case of a tie.
Objective evaluation
The objective color evaluations were made on the upper right central incisor. A silicone guide was prepared to standardize the color measurement using the spectrophotometer (Vita Easy Shade Advance™, Wilcos, Petrópolis, RJ, Brazil). The device tip was placed in the hole made in the middle third of the vestibular surface of the guide, and the color was evaluated 3 times for the tooth 11. The final result was the mean of the 3 values for L *, a *, and b *.
Color change values (ΔE) were calculated considering L *, a *, and b *parameters measured at baseline (before bleaching) and 1 week after beginning the bleaching (ΔE at T2), 2 weeks after beginning (ΔE at T3), 1 week after finishing the beaching (ΔE at T4), and 6 months after finishing the bleaching (ΔE at T5). All color changes (ΔE) were calculated with respect to the L *, a *, and b * baseline values, using the following formula:
Tooth sensitivity and gingival irritation evaluation
Participants were asked about the presence and intensity of tooth sensitivity or pain from T1 to T4. The degree of tooth sensitivity reported was recorded using a Visual Numeric Scale (VNS), using the following categories: none, mild, moderate, and severe.
Gingival irritation was assessed by a calibrated examiner (intra-examiner kappa = 0.79) using the Modified Gingival Index (MIG) [24]. The marginal and interproximal tissues were scored separately as follows: 0–no inflammation; 1–mild inflammation, a slight change in color and texture in part of the gingiva; 2–mild inflammation involving the entire gingival margin; 3–moderate inflammation, shiny surface, and edema; and 4–severe inflammation, spontaneous bleeding, and marked edema. The total MGI per individual was obtained by adding the values of tooth sites and dividing by the number of teeth analyzed.
Oral health-related quality of life
The Brazilian version of the OIDP scale [25] was administered as an interview at baseline (T1) and 1 month after the beginning of treatment (T4) to evaluate the perception of changes in oral health after bleaching. Each individual was asked whether, in the last month, he had experienced any problem with his oral health that caused difficulties with the following activities: eating or enjoying food, speaking and pronouncing words clearly, cleaning teeth, sleeping, smiling, smiling while showing your teeth without embarrassment, maintaining an emotional state without becoming bored, performing work or studies, and enjoying contact with other people. The possible answers were: yes or no. When the participants reported effect on their daily performance, they were asked about their major symptoms (e.g., pain, discomfort, limitations at work, dissatisfaction with one’s appearance, or others) and the main oral conditions that caused the difficulty. The frequency and severity of the effects on each oral condition was recorded. The OIDP scale for each domain was obtained by multiplying the frequency by severity. The total effect on quality of life was the sum of the all scores for each condition reported by the patient.
Statistical analysis
A blind researcher performed the statistical analyses using the Statistical Package for Social Sciences (SPSS for Windows, version 24.0, SPSS Inc., Chicago, IL, USA). Linear associations, chi-square, and McNemar tests compared, respectively, the bleaching groups with regard to categorical variables, OIDP domains and total OIDP. The Mann-Whitney and Wilcoxon tests compared respectively the evaluation times and color parameters. The Man-Whitney and Friedman tests were used in the comparisons of evaluation times and sensibility and gingival irritation. Inter-groups and intra-groups comparisons of evaluation times and OIDP parameters were made using chi-square and McNemar tests respectively.
Results
Of the 54 participants, 33 were women, 16 were in the HP6% group, and 17 were in HP15% group. The mean age was 26.38 years, and 66.7% of participants in the HP6% group, and 77.8% of those in HP15% group were aged 18–29.
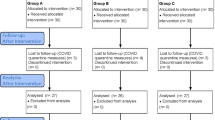
Figure 1 shows the patient flow throughout in the course of the study. Both groups began with 27 participants and concluded the bleaching with 26 individuals. Six months after bleaching, 19 participants from each group returned for the evaluation.
The frequency of patients distributed according to the color evaluated along the bleaching was demonstrated in Fig. 2. It was observed that 57.1% of the participants in the HP6% group and 43.7% in the HP15% groups showing the B1 color in T4 migrated to a darker color in T5.
Table 1 shows the color parameters according to the evaluation times. Intergroup comparisons at the same time interval revealed a significant difference on the Vita™ scale values at the end of bleaching and 6 months after bleaching. Intragroup comparisons between baseline and T3, T4, or T5 showed a significant difference in the parameters L, a *, and b * and Vita™ scale, for both groups. Intragroup comparisons between baseline and one week and 6 months after finishing the bleaching show that ΔE differed significantly for PH15% group.
Approximately 29.6% of the participants in HP6 and 44.4% in HP15% reported tooth sensitivity 1 week after the beginning of bleaching. Approximately 57.7% of the participants in HP6 and 53.8% of those in HP15% reported gingival irritation two weeks after the beginning of bleaching. Table 2 compares tooth sensitivity and gingival irritation between groups and across evaluation times. No significant differences were observed between groups in relation to tooth sensitivity or gingival irritation.
Table 3 reports the domains as well as the initial and final OIDP total scores by groups. No significant between-group differences were found in relation to the domains or global OIDP score.
Discussion
In the present study, low-concentration hydrogen peroxides used for in-office bleaching were effective and showed low levels of tooth sensitivity and gingival irritation. The bleaching with low-concentration peroxides did not generate adverse effects that affected the oral health-related quality of life of the participants. The color stability was low, and the groups did not keep the same color obtained at the end of treatment 6 months after bleaching. In the present study, the effectiveness of in-office bleaching for the HP6% (ΔE = 4.9) and HP15% (ΔE = 8.2) was similar to that of other studies that used the same HP concentrations and protocols presented [14,15,16]. The parameter ΔE is the shade difference between two objects or the same object evaluated in two distinct moments, calculated within the CIELAB color system [26]. The naked eye is able to distinguish color differences if the value of ΔE is higher than 3.3 [1]. In the present study, both bleaching groups had values of ΔE higher than 3.3, confirming the clinical effectiveness of tooth bleaching observed with the naked eye.
Quantitative color assessment is more objective, which eliminates the bias potential and variability of human judgment [27]. A spectrophotometer enables a color evaluation through the CIEL a*b* system. In this system, L * represents the value of luminosity or darkness, a * is the measure along the red-green axis and b * is the measure along the yellow-blue axis. A value a * positive indicates the red direction, a negative value of a * represents the green direction. A positive value of b * denotes a color in the yellow direction, whereas a negative value of b * indicates a color in the blue direction [26]. Bleaching it is expected to increase the value in the parameter L, and the values of the parameters a * and b * should approach zero [26]. In the present study, the HP6% group showed an increase in L at the end of treatment compared with baseline, indicating higher luminosity. The initial values for parameter a * were negative, consequently closer to green. With bleaching, these values became even more negative, bringing even more of the green. The parameter b * decreased in yellowing, approaching zero. The HP15% group showed tooth bleaching, despite a slight decrease in the L and a * parameters and a greater reduction in b *. These changes in color parameters were lower than those found in the other studies that using the same concentrations of the bleaching agents [14, 27, 28]. Yellower teeth at baseline showed better tooth bleaching results [29]. The minimum color change observed in the present study after treatment compared with others might be because the initial color was lighter than that normally used in other studies. The current patients desired to undergo the bleaching procedure, despite their lighter initial dental color. A decrease of 1 unit in the yellowing entails a color improvement of approximately 10% [30].
Dental bleaching has become one of the fastest growing areas of dentistry for patients and industry investment [31]. The incorporation of the nanoparticles TiO_N into hydrogen peroxide reduces the concentration of the latter, improves the biocompatibility of therefore prevents postoperative sensitivity and increases the safety of bleaching procedures. Irradiation with an appropriate light source will generate high concentrations of free radicals and other reactive oxygen species that are necessary to break down the molecular bonds of pigments within the tooth structure [32]. Titanium oxide nanoparticles doped with nitrogen enables the catalytic activity to occur when exposed to wavelengths in the band of the visible light, avoiding the use of ultraviolet light [15, 33]. The interaction between reduced concentration of hydrogen peroxide and the photocatalyzation by LED/laser light can result as low sensitivity [15]. Infrared lasers promote a high polarization of the nervous membrane, thus, reducing action potentials and the occurrence and the intensity of the sensitivity [30, 34].
When a lower concentration of hydrogen peroxide is used, it is necessary to have a greater number of applications to optimize the results of tooth bleaching [35]. In the present study, the number of applications and the contact time of the bleaching gel with the dental surface were the same for both groups. The results did not reveal significant differences in the color changes between the concentrations of bleaching agents considering the parameters L*, a* and b*. This null result demonstrates the greater performance of HP6% with TIO_N nanoparticles because although the peroxide concentration was halved, changes in the color parameters were practically the same between the groups. These results corroborate those of Matis et al. [2007] [36] and Bortolatto et al. [2014] [15], who observed that the contact time might be important in the bleaching process, and the concentration of the bleaching agent is not the most relevant factor. In the present study, cases of a dental darkening of approximately 57.1 and 43.7% were observed in HP6% and HP15%, respectively, 6 months after the bleaching. These results demonstrate that HP15% obtained higher color stability. The results of the present study corroborate with those of a study that evaluated the 9-month stability of HP6%, reporting a color return greater than 50% [33].
Reports of dental sensitivity are greater during the first 24 h after treatment, and can extend for approximately 5 days [37]. In the present study, both groups showed the rates of tooth sensitivity superior of 50% one week after bleaching. The sensitivity of 15% hydrogen peroxide was reported from 31% [15] to 64% [27]. Considering a scale from 0 to 10, the sensitivity of agents with low concentration varies from 0.6 [7, 38] to 2.4 [15]. In the present study, the sensitivity rate was higher than 40%. Although this rate was higher than that found in other studies, the median was lower, which demonstrated that many patients reported low-intensity dental sensitivity. The tooth sensitivity rate found for HP6% in-office bleaching group in the present study was higher than that presented by Bortolatto et al. [2016] [14] but lower than the rate of 50% [16] presented by Martin et al. [2015]. We did not find previous studies comparing the sensibility of 6% and 15% hydrogen peroxides. In the present study, the sensibility of HP 15% was statistically higher than HP6% 1 week after the beginning of bleaching. The higher HP15% sensibility is probably due to the concentration twice as higher than the HP6% agent.
Hydrogen peroxide can cause a burning sensation and tissue damage such as destruction and detachment of the epithelial layer when in contact with the gum [4]. In the present study, both groups had a gingival irritation rate greater than 50%, similar to the rate of 52% [27] previously found with HP15%. In both groups, the intensity of irritation was considered mild. Both groups had similar frequencies of gingival irritation rates in the course of treatment, without significant differences between them. The hypersensitivity and gingival irritation in the current study were minor and disappeared spontaneously without requiring an interruption in treatment; these results match those of Bizhang et al. [2009] [27]. No significant between-group differences in sensitivity or gingival irritation were found, showing that despite the higher frequencies of sensitivity and low gingival irritation, HP15% should be considered the first choice for bleaching since it presented a higher effectivity and stability.
Patient perceptions are important when assessing oral health needs and for determining the outcomes of dental procedures [39]. It is important to incorporate the assessment of the perception of changes after dental treatments into clinical trials [39]. The instruments that evaluate oral health-related quality of life are being increasingly used in dentistry research [40]. Bleaching can produce positive or negative effects on oral health-related quality of life [22]. The positive effects are related to the improvements in esthetics and appearance, which increase the ease of smiling [22]. The positive effects on quality of life are detected when major changes of color occur, especially when the teeth are no longer very yellowish [22, 29]. The negative effects are related to pain, discomfort and difficulty with oral hygiene caused by sensitivity or gingival irritation [22]. The Oral Impact on Daily Performance (OIDP) scale measures the consequences of oral disease on three levels, including oral health status, changes in oral tissues, and ability to perform daily activities [41]. This instrument has the advantages of using an objective approach that encompasses the main consequences of bleaching, avoids overlapping repeated scores of the same effect, and records only the significant effects [41]. The present study did not observed positive or negative effects of bleaching on oral health-related quality of life as assessed by the OIDP. The absence of a positive effect was most likely due to the discreet color change because the participants began with a light color and therefore did not experience large color variations. The low intensity of sensitivity and gingival irritation from bleaching might have contributed to the absence of negative effects.
One drawback of this study was a high dropout rate that reached 29.6% in 6-months follow-up. This dropout rate is an imminent bias source, decreasing the test power to reject the null hypothesis when the alternative hypothesis is true. Nevertheless, the losses were identical in both treatments and did not affect the balance between the comparison groups.
Despite the greater frequency of sensitivity, 15% hydrogen peroxide demonstrated higher bleaching effectiveness at the end of treatment and greater color stability at 6-month follow-up, compared to 6% hydrogen peroxide.
Conclusions
The low-concentration bleaching agents used for in-office tooth bleaching were effective and showed low levels of tooth sensitivity and gingival irritation. These bleaching agents did not generate adverse effects that affected the oral health-related quality of life of the participants. At 6-month follow-up, HP15% presents greater color stability than HP6%.
References
ADA (2006) Dentist dispensed home-use tooth bleaching products. In: Am. Dent. Assoc. http://www.ada.org/ada/seal/standards/guide_home_
Joiner A (2006) The bleaching of teeth: a review of the literature. J Dent 34:412–419. https://doi.org/10.1016/j.jdent.2006.02.002
Bruzell EM, Pallesen U, Thoresen NR, Wallman C, Dahl JE (2013) Side effects of external tooth bleaching: a multi-centre practice-based prospective study. Br Dent J 215:E17. https://doi.org/10.1038/sj.bdj.2013.1047
SCCP The Scientific Committee on Consumer Products (2005) Public consultation on a preliminary opinion on hydrogen peroxide in tooth whitening products. http://ec.europa.eu/health/ph_risk/committees/04_sccp/docs/sccp_cons_01_en.pdf
Haywood VB, Caughman WF, Frazier KB, Myers ML (2001) Tray delivery of potassium nitrate-fluoride to reduce bleaching sensitivity. Quintessence Int 32:105–109
Kossatz S, Dalanhol AP, Cunha T, Loguercio A, Reis A (2011) Effect of light activation on tooth sensitivity after in-office bleaching. Oper Dent 36:251–257. https://doi.org/10.2341/10-289-C
Martin J, Fernandez E, Bahamondes V et al (2013) Dentin hypersensitivity after teeth bleaching with in-office systems. Randomized clinical trial. Am J Dent 26:10–14
de Souza Costa CA, Riehl H, Kina JF, Sacono NT, Hebling J (2010) Human pulp responses to in-office tooth bleaching. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 109:e59–e64. https://doi.org/10.1016/j.tripleo.2009.12.002
Munro IC, Williams GM, Heymann HO, Kroes R (2006) Use of hydrogen peroxide-based tooth whitening products and its relationship to oral cancer. J Esthet Restor Dent 18:119–125. https://doi.org/10.1111/j.1708-8240.2006.00006.x
Munro IC, Williams GM, Heymann HO, Kroes R (2006) Tooth whitening products and the risk of oral cancer. Food Chem Toxicol 44:301–315. https://doi.org/10.1016/j.fct.2005.07.012
Goldberg M, Grootveld M, Lynch E (2010) Undesirable and adverse effects of tooth-whitening products: a review. Clin Oral Investig 14:1–10. https://doi.org/10.1007/s00784-009-0302-4
Gerlach RW, Zhou X (2002) Comparative clinical efficacy of two professional bleaching systems. Compend Contin Educ Dent 23:35–41
Reis A, Kossatz S, Martins GC, Loguercio AD (2013) Efficacy of and effect on tooth sensitivity of in-office bleaching gel concentrations: a randomized clinical trial. Oper Dent 38:386–393. https://doi.org/10.2341/12-140-C
Bortolatto JF, Trevisan TC, Sadalla P et al (2016) A novel approach for in-office tooth bleaching with 6% H2O2/TiO_N and LED/laser system—a controlled , triple-blinded , randomized clinical trial. Lasers Med Sci 31:437–444. https://doi.org/10.1007/s10103-016-1866-2
Bortolatto JF, Pretel H, Floros MC, Luizzi ACC, Dantas AAR, Fernandez E, Moncada G, de Oliveira OB Jr (2014) Low concentration H(2)O(2)/TiO_N in office bleaching: a randomized clinical trial. J Dent Res 93:66S–71S. https://doi.org/10.1177/0022034514537466
Martín J, Vildósola P, Bersezio C, Herrera A, Bortolatto J, Saad JRC, Oliveira OB Jr, Fernández E (2015) Effectiveness of 6% hydrogen peroxide concentration for tooth bleaching—a double-blind, randomized clinical trial. J Dent 43:6–13. https://doi.org/10.1016/j.jdent.2015.05.011
Vildósola P, Bottner J, Avalos F, Godoy I, Martín J, Fernández E (2017) Teeth bleaching with low concentrations of hydrogen peroxide (6%) and catalyzed by LED blue (450 ± 10 nm) and laser infrared (808 ± 10 nm) light for in-office treatment: randomized clinical trial 1-year follow-up. J Esthet Restor Dent 29:339–345. https://doi.org/10.1111/jerd.12318
Fernández E, Bersezio C, Bottner J, Avalos F, Godoy I, Inda D, Vildósola P, Saad JRC, Oliveira OB Jr, Martín J (2017) Longevity, esthetic perception, and psychosocial impact of teeth bleaching by low (6%) hydrogen peroxide concentration for in-office treatment: a randomized clinical trial. Oper Dent 42:41–52. https://doi.org/10.2341/15-335-C
Angel P, Bersezio C, Estay J et al (2018) Color stability, psychosocial impact, and effect on self-perception of esthetics of tooth whitening using low-concentration (6%) hydrogen peroxide. Quintessence Int 49:557–566. https://doi.org/10.3290/j.qi.a40468
Bersezio C, Martín J, Angel P, Bottner J, Godoy I, Avalos F, Fernández E (2018) Teeth whitening with 6% hydrogen peroxide and its impact on quality of life: 2 years of follow-up. Odontology. https://doi.org/10.1007/s10266-018-0372-3
Schulz KF, Altman DG, Moher D (2010) CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. PLoS Med 7:1–7. https://doi.org/10.1371/journal.pmed.1000251
Meireles SS, Goettems ML, Dantas RVF, Bona ÁD, Santos IS, Demarco FF (2014) Changes in oral health related quality of life after dental bleaching in a double-blind randomized clinical trial. J Dent 42:114–121. https://doi.org/10.1016/j.jdent.2013.11.022
Tavares M, Stultz J, Newman M et al (2003) Light augments tooth whitening with peroxide. J Am Dent Assoc 134:167–175
Lobene RR, Weatherford T, Ross NM et al (1986) A modified gingival index for use in clinical trials. Clin Prev Dent 8:3–6
Abegg C, Fontanive VN, Tsakos G, Davoglio RS, de Oliveira MMC (2015) Adapting and testing the oral impacts on daily performances among adults and elderly in Brazil. Gerodontology 32:46–52. https://doi.org/10.1111/ger.12051
Commission Internationale de L’Eclairage (1978) Recommendations on uniform colour spaces, colour terms. Bureau Central de la CIE, Paris
Bizhang M, Chun Y-HP, Damerau K, Singh P, Raab WHM, Zimmer S (2009) Comparative clinical study of the effectiveness of three different bleaching methods. Oper Dent 34:635–641. https://doi.org/10.2341/08-069-C
Matis BA, Cochran MA, Eckert G (2009) Review of the effectiveness of various tooth whitening systems. Oper Dent 34:230–235. https://doi.org/10.2341/08-74
Gerlach RW, Zhou X (2001) Vital bleaching with whitening strips: summary of clinical research on effectiveness and tolerability. J Contemp Dent Pract 2:1–16
Martín J, Ovies N, Cisternas P, Fernández E, Oliveira Junior OB, de Andrade MF, Moncada G, Vildósola P (2015) Can an LED-laser hybrid light help to decrease hydrogen peroxide concentration while maintaining effectiveness in teeth bleaching? Laser Phys 25:1–5. https://doi.org/10.1088/1054-660X/25/2/025608
Suyama Y, Otsuki M, Ogisu S et al (2009) Effects of light sources and visible light-activated titanium dioxide photocatalyst on bleaching. Dent Mater J 28:693–699
Sulieman M, Addy M, Rees JS (2003) Development and evaluation of a method in vitro to study the effectiveness of tooth bleaching. J Dent 31:415–422
Vano M, Derchi G, Barone A, Genovesi A, Covani U (2015) Tooth bleaching with hydrogen peroxide and nano-hydroxyapatite: a 9-month follow-up randomized clinical trial. Int J Dent Hyg 13:301–307. https://doi.org/10.1111/idh.12123
Soares DG, Ribeiro APD, da Silveira Vargas F, Hebling J, de Souza Costa CA (2013) Efficacy and cytotoxicity of a bleaching gel after short application times on dental enamel. Clin Oral Investig 17:1901–1909. https://doi.org/10.1007/s00784-012-0883-1
Sulieman M, Addy M, MacDonald E, Rees JS (2004) The effect of hydrogen peroxide concentration on the outcome of tooth whitening: an in vitro study. J Dent 32:295–299. https://doi.org/10.1016/j.jdent.2004.01.003
Matis BA, Cochran MA, Franco M, al-Ammar W, Eckert GJ, Stropes M (2007) Eight in-office tooth whitening systems evaluated in vivo: a pilot study. Oper Dent 32:322–327. https://doi.org/10.2341/06-135
Sulieman MA (2008) An overview of tooth-bleaching techniques: chemistry, safety and efficacy. Periodontol 2000(48):148–169. https://doi.org/10.1111/j.1600-0757.2008.00258.x
Moncada G, Sepúlveda D, Elphick K, Contente M, Estay J, Bahamondes V, Fernandez E, Oliveira OB, Martin J (2013) Effects of light activation, agent concentration, and tooth thickness on dental sensitivity after bleaching. Oper Dent 38:467–476. https://doi.org/10.2341/12-335-C
Buck D, Newton JT (2001) Non-clinical outcome measures in dentistry: publishing trends 1988-98. Community Dent Oral Epidemiol 29:2–8
Preciado A, Del RJ, Lynch CD, Oyagüe RC (2013) A new, short, specific questionnaire (QoLIP-10) for evaluating the oral health-related quality of life of implant-retained overdenture and hybrid prosthesis wearers. J Dent 41:753–763. https://doi.org/10.1016/j.jdent.2013.06.014
Adulyanon S, Vourapukjaru J, Sheiham A (1996) Oral impacts affecting daily performance in a low dental disease Thai population. Community Dent Oral Epidemiol 24:385–389
Acknowledgements
The authors are grateful to CAPES (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior) for providing the scholarship to Nayara Kelly Lyrio Ferraz and to the Postgraduate Collegiate (Faculty of Dentistry, Universidade Federal de Minas Gerais). We thank Prof. Dr. Osmir Batista de Oliveira Júnior, FOAR-UNESP for loaning the LED/laser equipment Whitening Laser II DMC.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author Nayara Kelly Lyrio Ferraz declares no conflicts of interest.
The author Lilian Capanema Nogueira declares no conflicts of interest.
The author Isabela Moreira Neiva declares no conflicts of interest.
The author Raquel Conceição Ferreira declares no conflicts of interest.
The author Allyson Nogueira Moreira declares no conflicts of interest.
The author Claudia Silami Magalhães declares no conflicts of interest.
Ethical approval
This study followed the ethical principles established in the Helsinki Declaration of 1964, and was approved by the University Ethics Committee (Process no. 1.269.466). The study was registered as a clinical trial (NCT02816593-https://clinicaltrials.gov/ct2/results?term=NCT02816593&Search=Pesquisa) and reported in accordance with the CONSORT Statement (Consolidated Standards of Reporting Trials).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Ferraz, N.K.L., Nogueira, L.C., Neiva, I.M. et al. Longevity, effectiveness, safety, and impact on quality of life of low-concentration hydrogen peroxides in-office bleaching: a randomized clinical trial. Clin Oral Invest 23, 2061–2070 (2019). https://doi.org/10.1007/s00784-018-2607-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-018-2607-7