Abstract
Objective
This study used three LASERs (red, green, and blue) with a spectrophotometer to compare the light propagation for the following: absorption (A), transmittance (T), attenuation (K), and scattering anisotropy coefficient (g) in dental tissues and nano-filled resin-based composites. This study used three distinct incremental build-up techniques, which included one shade (body), two shades (enamel and dentin), and three shades (enamel, transparent, and dentin).
Methods
Twenty human, un-erupted, recently extracted third molars (shade B1) were used to obtain 40 tooth slabs. The samples were randomized and equally distributed into four experimental groups. The Positive Control Group included dental tissues with enamel, dento-enamel junction DEJ, and dentin; the Technique 1 group (T1) included one shade tissues, B1B; the Technique 2 group (T2) included two-shades tissues, A2Dentin and B1Enamel; and the Technique 3 group (T3) included three shade tissues, A2Dentin, Transparent, and B1Enamel. Cavity preparation was standardized, and, using the spectrophotometer, each specimen was irradiated by three LASERs. A voltmeter recorded the light-output signal, and from this raw data, the following optical constants (A, T, K, g) were calculated.
Results
ANOVA, followed by a post hoc Tukey’s test (p < 0.05), revealed that absorption and transmittance in dental tissues were significantly different when comparing the three build-up technique groups. However, when examining attenuation coefficient, there was no significant difference in dental tissues for T2 and T3 as analyzed by blue and red lasers. There was also no significant difference among the three lasers for T2 and T3. There was also no significant effect of the types of experiments on the value of scattering anisotropy factor g for blue laser among the four experimental groups.
Conclusion
Within the limitations of this study, none of the build-up techniques were able to reproduce the dental tissues optical properties, and T2 and T3 resulted in a similar pattern of light propagation.
Clinical significance
The clinical success of restorative procedures depends on selecting materials and techniques that emulate the natural tooth and provide long-term stability in color and optical properties.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Restorative dentistry is a mixture of art, science, and technology. Successful esthetic reproduction of teeth, especially in terms of reproducing its natural color, requires an understanding of the interrelationship of optical properties and dental morphology. More importantly, this understanding is integral to obtaining direct build-ups that are imperceptible to surrounding tooth structures. Studies examining the differences in light propagation between dental tissues and RBC are sparse but are necessary for the success of restorative procedures that depend on selecting the right materials and techniques that emulate natural dental tissues and provide long-term stability in color and optical properties.
As defined by physics, color is light. When light hits an object, a range of interactions results. The light may be reflected, refracted, absorbed, scattered, and/or transmitted (Fig. 1) [1]. Small amounts of light are also reflected from the surface, at the boundary between the object and air, due to the change in refractive index (the refractive index of material is the ratio of the speed of light in a vacuum to the speed of light in the material) [2].
Transparency, absorption, scattering, and transmitted light play significant roles when studying the importance of light on color. This is especially important in the context of this study, which examined the interactions between light and natural tooth tissue and compared it to the interactions between light and composite restorative materials.
Transparency appears when light passes through a material and can vary, depending on the amount of light absorbed or scattered from different materials. The amount of light transmitted through a material thickness defines the level of translucency. For example, one way of measuring translucency is by determining total transmission, including scattering, by using a spectrophotometer with an integrating sphere, which can be expressed as transmission coefficient. Transparency is a crucial component when creating dental restorations with a light/composite interaction that closely resembles that of light/natural dentition, and numerous factors can affect the translucency of resin-based composite (RBC) restorations such as filler particles and opacifiers [3], resin matrix composition [4], and thickness [5]. Several studies have also evaluated the translucency of RBC [6] and the influence of other factors on the translucency such as resin polymerization, and aging [7, 8], flow-ability and light curing [9].
Equally important is the absorption of light from a material. When light passes through an object, it can be either absorbed, scattered, transmitted, or reflected based on the heterogeneity of the medium. Absorbed light is defined as the energy from light that is absorbed in the volume of the material observed. This process occurs when incident light is partially removed by interactions with molecules within the object.
Scattering is a kind of reflection that takes place when particles are present in the material. When light hits an obstacle in the medium, a scattering event can occur and can cause the light-propagation direction to change. If light finds another obstacle, a new scattering event can take place and the light-propagation direction changes again. Scattering depends on the refractive indexes of the medium, the wavelength of irradiation, and the particle which causes the scattering. Moreover, on the particle diameter and cross section [10], the direction and the amount of scattered light depends on the size of the particles and their refractive index relative to the refractive index of the material in which they are embedded [2].
Both absorption and scattering can be used to determine the penetration depth of light in tissues as a function of wavelength, which can be used as a possible application in imaging clinical diagnosis [11].
Other factors that can influence the color of an object include the following: transmitted light, which happens when the light emerges from a material propagating in the same direction as the incident light; and attenuation which is the gradual loss in intensity of any kind of flux through a medium. Under clinical examination of coronal dentine, light must first pass through the full thickness of the enamel before it reaches the dentine. The attenuation of light in sound enamel is relatively small and is not significantly affected by its structural orientation; however, the signal from underlying dentine would still carry significant information [12].
In an effort to examine the role of light and its importance in restorative procedures, this in vitro observational compared the differences in light propagation—light absorption (A), light transmission (T), light attenuation (K), and scattering anisotropy factor (g)—and how light responded within natural dental tissues (enamel, dento-enamel junction DEJ, and dentin) and how it responded in nano-filled RBCs that utilized one, two, or three shade build-ups and incremental techniques tested by three different lasers (blue, green, and red).
Materials and methods
Sample selection and preparation
For this study, 20 human, un-erupted, extracted, third-molar teeth were selected randomly from the Iowa Institute for Oral Health Research and Oral Surgery Department at The University of Iowa. The source of each tooth was unknown, and intact crowns without any defect were selected to avoid the age factor (wear and staining) that could compromise the results of the study.
In order to standardize shading between teeth, shade mapping was done using a Vita Easyshade Compact Spectrophotometer (Vita Zahnfabrik), which is a cordless version of the VITA Easyshade device (Fig. 2) that delivers instant, accurate shades regardless of lighting conditions and other elements that can lead to improper shade measurement.
After storing the teeth in artificial saliva with chloramine T in a refrigerator, the teeth were mounted in stone blocks using Die-Keen (Heraeus Kulzer), mixed with water, and poured in a mold. All teeth were placed and aligned so that the long axis of each tooth was parallel with the vertical wall of mold (parallel B-L, M-D surfaces to sides of mold and CEJ to horizontal plane with enough tooth above the mold surface to avoid stone contamination during bonding but with enough root embedded in stone for secure mounting). Almost an hour later, the stone blocks were separated from the mold and samples were checked to see if they were firmly embedded in stone blocks. The remaining wax and excess stone were removed, and the teeth were returned to artificial saliva until test (Fig. 2).
After the mounting and the storage, each tooth was laterally cut into slabs. All cuts were made with an automatic precision cut-off machine (Accutom-5 Struers, Ballerup). Three to four sawing discs (depending on the size of the tooth) with two or three separators (0.75 mm thickness) between each disc were used with each tooth to obtain slabs with 1.5 mm thickness (Fig. 2).
All restorative procedures were done by one calibrated operator using one visible-light activated restorative nano-composite (Filtek Supreme Ultra Universal Restorative 3 M) designed for anterior and posterior direct restorations. The purpose of using Filtek Supreme Ultra Universal Restorative (3 M) was due to its smaller particle size (nano-fills exhibit very good fracture and wear resistance) but also because it is well sculpted and demonstrates a good color stability.
The resin system was based on BIS-GMA, BIS-EMA, and UDMA with small amounts of TEGDMA. Translucent shades contained a combination of a nonagglomerated/nonaggregated, 75 nm silica nano-filler, and a loosely bound agglomerate silica nanocluster consisting of agglomerates of primary silica nano-particles of 75 nm size fillers. The cluster size range was 0.6 to 1.4 mm. The filler loading was 72.5% by weight.
One calibrated operator performed all procedures and tests, and the design of all composite preparations and restorations was standardized. The tooth lengths were checked with a periodontal probe and were marked down to 4 mm with all samples. The preparations were standardized using #58 carbide bur. Thickness of each sample was 1.5 mm, length of the cavity is 4 mm, and width 3 mm. Samples were randomly assigned into four groups:
-
Group 1: Natural sample (control group)
-
Group 2: Technique 1 (T1) 1 shade
After preparing the cavity with carbide bur #58, 35% phosphoric acid etchant (Fig. 2) was applied to enamel and then to dentin (etchant remained on dentin for less than 15 s). The cavity was rinsed thoroughly for 15 s or until excess moisture was completely removed from the operatory field.
The dentin surface was slightly moistened. The adhesive system Optibond FL (Kerr) was applied starting with primer with microbrush for 30 s with continuous gentle agitation (Fig. 2). The surface was initially air-dried primer gently and then finished with moderate air pressure to evaporate all solvents. The dried surface was shiny and evenly primed appearance. Adhesive was applied with a microbrush to spread evenly, removing any excess that could cause pooling or marginal buildup. The surface was then light cured for 35 s (18.6 J/cm2). The RBC was applied using 1 shade (B1 Body) in multiple increments (+/−2 mm) and then lightly cured for 30 s (16 J/cm2).
-
Group 3: Technique 2 (T2) 2 shades
The same techniques from T1 were used for acid etching and adhesive procedures in group 3 samples; however, the RBC was applied using two shades; A2Dentin and B1Enamel. A2D was applied to restore the dentin, and B1E was used to restore the enamel surface. The enamel and dentin were easily visualized under ×3.5 magnification (Surgitel MicroLine Loups). Consequently, the dentin and enamel height were marked down and restored with A2D and B1E, respectively, by using composite hand instruments and then light cured for 30 s (16 J/cm2).
-
Group 4: Technique 3 (T3) 3 shades
The same techniques were used for acid etching and the adhesive procedures as groups 2 and 3; however, RBC was applied in three shades: A2Dentin, Transparent, and B1Enamel. The A2D composite material was applied to restore the dentin, the transparent shade restored the DEJ, and B1E repaired the enamel surface. Dentin, DEJ, and enamel were marked down and restored with A2D, T, B1E, respectively, and then light cured for 30 s (16 J/cm2).
After restoring all teeth cavities, height was measured at 4 mm using a digital caliber. A diamond disc (Struers Inc.) on a laboratory straight handpiece (KaVo Dental) was used to section the samples from the mounted blocks at 4 mm height. Adjustments were made using a polishing paper to get the most accurate thickness and length. Specimens were polished on wet 400 and 600 grit silicon carbide grinding paper on a grinder-polisher (Buehler-Met II, Buehler) at 200 rpm for 5 min using light hand pressure. (A step-by-step procedure is presented in Fig. 2, and the techniques used are shown in Fig. 3)
After the finishing procedure, all samples were washed and cleaned in running water and their thickness was re-measured to achieve a uniform thickness of 1.5 ± 0.05 mm. The occlusal surface was flattened in order to grip the sample with the holder without slipping (this allowed a more accurate position on the rotary stage for measurements). Teeth were kept hydrated at all times until restorations were done and then were stored back in artificial saliva.
Experimental setup
Light transmittance (T), light absorption (A), and light attenuation (K)
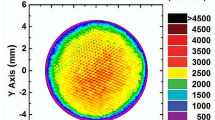
The set ups used for light propagation measurements (Fig. 4) schematically consisted of a laser source, a goniometric rotary stage, and a photodiode detector connected to an amplifier-multimeter (34401A, Agilent Technologies) measuring system. The detector was mounted at one of the collimators that had an aperture of 5 cm in diameter, and the samples were placed at the center of the rotary stage of the spectrophotometer at 0° angle and irradiated with the laser beam that was placed on the other collimator from occlusal to cervical. The laser energy light propagated through the sample and was detected by the power meter.
Before each measurement, calibration was done with every reading starting at 8.1 V with the surrounding light and without hitting the sample. Due to the sensitivity of the laser, five readings were obtained for each sample and the means were calculated. Three portable lasers with different wavelengths were used. A blue laser wavelength was measured at 405 ± 10 nm, a green laser wavelength was 532 ± 10 nm, and the red laser wavelength was 650 ± 10 nm. The experimental temperature was 70 °F with humidity of 1%. Samples were kept hydrated at all times until the measurements were performed and were then put back in artificial saliva for storage. The distance between the sample and the laser source did not have a significant effect on the measurement because of the very low divergence angle of the laser beam. The beam noise level was 1 mW and its diameter 2.54 mm.
Scattering anisotropy coefficient (g)
Light scattering measurements were performed using the same light propagation set up described above with the addition of pellicle beamsplitters (74.9 mm, 51.6 mm Clear, Coated) (Fig. 5). The pellicle beamsplitters are ultra-lightweight membranes manufactured by stretching a 5 μm thick polymer membrane over a flat metal frame. The extreme thinness eliminates multiple reflections associated with plate beamsplitters and enables functionality at a broad wavelength range (375–2400 nm).
Samples were placed at the center of the rotary stage of the spectrophotometer at 45° angle and irradiated with the laser beam. The light propagated through the sample was then detected by the power meter. The measured light first reflected off the beamsplitter and then reflected off of the tooth without blocking backscattered light. The second instance, light passed through the beamsplitter at a 45° angle between the laser light and the tooth so that it reflected light from the laser toward the tooth and also transmitted light that scattered off the sample (it was detected by the photodiode for five scattering angles: 0°, 2°, 4°, 6°, and 8°). Angles were measured between 0° and 10°, and no signal was detected above this angulation.
All measurements were performed and obtained identically according to their groups, and data was collected using three lasers with different wavelengths. Blue laser wavelength of 405 ± 10 nm, green laser wavelength of 532 ± 10 nm, and red laser wavelength of 650 ± 10 nm. Temperature was 70 °F with humidity 1%. Samples were kept hydrated at all times during measurements and then they were put in artificial saliva for storage.
The data was processed and calculated using the following formulas:
-
A.
For light transmittance (T), light absorption (A), and light attenuation (K):
- Light transmittance was defined as T = I (λ)/I0(λ) where I is the intensity of the light leaving the sample. I0 is the intensity of the light entering the sample.
- Light absorption (A) was defined as A = log I0(λ)/I (λ) where A = − log T.
- Light attenuation (K) was defined as K = A/x where x is the thickness of the specimen.
-
B.
For coefficient of light scattering (g):
From the measurements of scattered light signal (V) at various scattering angles (θ), the scattering anisotropy factor (g) was calculated by using the following formula:
where the sums were taken over the evaluated scattering angles and signal values, at an increment of scattering angle equal to 4°.
Descriptive statistics were conducted. One-way ANOVA, followed by the post hoc Tukey’s HSD (honestly significant difference) test, was performed to detect the difference in light absorption (A), light attenuation coefficient (K), light transmittance (T), and scattering anisotropy factor (g) among the four experimental groups (i.e., Dental Tissues, T1, T2, T3) for each of the three laser colors (Graphs 1, 2, 3, and 4).
All tests utilized a significance level of 0.05, and statistical analyses were performed using the statistical package SAS® System version 9.4 (SAS Institute Inc.).
Results
A total of 40 samples were randomly and equally distributed into four experimental groups (Dental Tissues, T1, T2, and T3). Table 1 provides a summary of descriptive statistics on light absorption (A), light attenuation coefficient (K), light transmittance (T), and scattering anisotropy factor (g) by technique types and laser colors.
Assessing the difference in A, K, T, and g values among four experimental groups within each of three laser colors
Light absorption
This analysis revealed a significant effect of the types of experiments on the light absorption with blue laser (F(3, 36) = 436.23, p < 0.0001), green laser (F(3, 36) = 127.91, p < 0.0001), and red laser (F(3, 36) = 275.38, p < 0.0001). The post hoc Tukey’s HSD test indicated that mean light transmittance value observed in the T1 group was significantly greater than that observed for the other three groups, while mean light transmittance value obtained for the Dental Tissues group was significantly lower than observed in the T1, T2 to T3 groups. Moreover, no significant differences were found between the T2 and T3 groups.
Light attenuation coefficient
Analysis revealed that there was a significant effect of the types of experiments on the light attenuation coefficient with blue laser (F(3, 36) = 24.49, p < 0.0001), green laser (F(3, 36) = 18.96, p < 0.0001), and red laser (F(3, 36) = 22.51, p < 0.0001). The post hoc Tukey’s HSD test indicated that mean light attenuation coefficient value observed in T1 group was significantly greater than observed for the other three groups, while no significant difference was found among the Dental Tissues, T2, and T3 groups with blue and red laser. However, with the green laser, mean light attenuation coefficient value obtained in the Dental Tissues was significantly lower than that observed in T1 to T3 groups. Moreover, no significant difference was found between T2 and T3 groups.
Light transmittance
Analysis revealed that there was a significant effect of the types of experiments on the light transmittance with blue laser (F(3, 36) = 453.32, p < 0.0001), green laser (F(3, 36) = 132.10, p < 0.0001), and red laser (F(3, 36) = 259.85, p < 0.0001). The post hoc Tukey’s HSD test indicated that mean light transmittance value observed in T1 group was significantly lower than that observed for the other three groups, while mean value in the Dental Tissues group was significantly greater than that observed in T1 to T3 groups. Moreover, no significant difference was found between T2 and T3 groups.
Scattering anisotropy factor
Analysis revealed that there was no significant effect of the types of experiments on the value of scattering anisotropy factor g for blue laser (F(3, 36) = 0.43, p = 0.7315), meaning that there was no significant difference in mean value of scattering anisotropy factor g among the four experimental groups.
For green laser, there was a significant effect of the types of experiments on the value of scattering anisotropy factor g (F(3, 36) = 6.21, p = 0.0016). The post hoc Tukey’s HSD test indicated that the mean value of scattering anisotropy observed in the Dental Tissue group was significantly greater than what was observed in T1 and T3 groups, while no significant difference was found between Dental Tissues and T2 or among T1 to T3 groups.
For red laser, there was a significant effect of the types of experiments on the value of scattering anisotropy factor g (F(3, 36) = 3.42, p = 0.0273). The post hoc Tukey’s HSD test indicated that the mean value of scattering anisotropy observed in T3 group was significantly lower than what was observed in the Dental Tissues group, while no significant difference was found among the Dental Tissues, T1, and T2 groups, and among the T1 to T3 groups.
Discussion
The tooth slabs selected used in this study were obtained from a pool of natural, extracted teeth at the University of Iowa, Oral Surgery Department. The facility receives a supply of teeth from the College of Dentistry where extractions of un-erupted third molars are often carried out.
This in vitro observational study assessed the difference in the light propagation of different shades of a nano-filled RBC (Filtek Supreme Ultra Universal Restorative 3 M). This system was chosen for its wide acceptance and popularity among clinicians [13] and is also the standard RBC used at the College of Dentistry & Dental Clinics at the University of Iowa. Following the manufacturer’s recommendations, the study’s researchers selected shades to match and emulate the natural dental tissues used in the study. Additionally, other shades were used to compare the optical properties of techniques tested in this study. Samples were kept hydrated during all measurements, especially since the translucency of dental tissue was influenced by dehydration caused by the replacement of water around the enamel prisms and by the air.
Light absorption (A)
Beer-Lambert’s law is best known for its solutions to absorbing radiation and that absorption depends on concentration and the path-length of light. Watts and Cash also emphasized that surface reflection could affect light absorbance measurements [14].
With respect to Beer-Lambert’s law and the outcomes uncovered in the analysis of the study’s experimental results, the study’s researchers concluded that their theoretical predictions and experimental findings coincide. That finding, by itself, is not surprising because each layering approach presents distincts thickness of composites with different opacity and overall appearance. For example, the T1 group presented a significantly higher refractive index than the other three groups, which is the result of chromatic saturation (a primary cause of opacity and lack of vitality of composite restorations as opposed to natural dentition). This explains that using one body shade without an enamel shade will provide an opaque material within a specific thickness, which will obstruct penetration of light [15]. Additionally, mean values in the Dental Tissues group were significantly lower than those observed in T1 to T3 groups, which shows that dental tissue is more transparent than composite material.
Light attenuation coefficient (K)
The T1 group was significantly greater than that observed for the other three groups, while no significant difference was found among the Dental Tissues, T2, and T3 groups. The same applied in light absorption. The lighter the color of the composite resulted in less energy being attenuated or lost on the material. Using one shade of the RBC showed that light was absorbed and attenuated more than other groups.
Body shades present intermediate translucency and opacity between enamel and dentin. This allows substitution in both enamel and dentin in only one layer [16]. Therefore, the concepts of “artificial enamel” and “artificial dentin” refer to composite resins designed to replace the physical and mechanical, as well as the color and optical properties of the tooth [17]. Studies have also shown that an ideal material for replacing dentin should have properties such as a uniform hue, opacity, and a wide range of saturations [18]. An important factor that affected the final outcome of a restoration depended on the thickness and the varying degrees of translucency, as well as the opacity of several layers of composite.
Enamel from its optical entity is the most difficult to imitate between all dental tissues. It is a common practice between practitioners to layer artificial enamel and dentin composites according to the actual thickness of the missing natural enamel and dentin; however, no known composite behaves exactly like natural enamel or dentin. By using composite resins to imitate dental tissues, and by pursuing a tooth’s anatomic and chromatic variability, the definitive restoration will be esthetically pleasing.
The use of artificial enamels within the same refractive index as natural dental tissues should be expected as an ideal reproduction of the optical characteristics. Unfortunately, having the correct refractive index is not only the components needed to mimic a restoration. Choosing artificial dentin and enamel composites of the proper opacities and determining the correct thickness of each layer is crucial and should be just as significant as the use of refractive indices [19].
Light transmittance (T)
When looking at light transmittance, the T1 group was significantly lower than what was observed for the other three groups, while the mean value in the Dental Tissues group was significantly greater than that observed in the T1 to T3 groups. Moreover, no significant difference was found between the T2 and T3 groups. This finding showed that light transmittance is inversely proportional to light absorption when thickness is a constant factor.
The refractive index of composite enamel (1.62) has an optical behavior similar to natural enamel. Increasing its thickness increases the refractive index value. With composite enamel, it is possible to manage the relationship between translucency value and the esthetic integration in a better way, especially since light passes through two bodies (natural enamel and composite enamel) with the same refractive index. In this way, there is no light deviation; however, from a clinical point of view, there is a problem since it produces a gray line at the margin. Moreover, in restorations of free-incisal enamel, this composite integrates perfectly, substituting the natural enamel with a high value without using dentin body [20].
A study by Naeimi Akbar and collaborators [21] compared the translucency of different shades of two highly esthetic multilayered restorative composite resins (shades from Esthet-X and from Filtek Supreme composite resins). The study revealed that there was a significant decrease in translucency from A2B to D2B and also in diffuse translucency from A4D to C6D shades of Filtek Supreme composite resin. Opaque dentin shades had the lowest total and diffused translucency values, and the translucent enamel shades had the highest translucency values in Filtek Supreme resin. Dentin shades also had the lowest total and diffused translucency values, and enamel shades had the highest translucency values. These findings were consistent with another study by Kamishima and collaborators [22] that showed that opaque shades of the composite resins were less translucent than other shades. Similarly, Ikeda and collaborators demonstrated that opaque shades were less translucent than body shades in several restorative composite materials. Light propagation of these materials is affected by the difference in the refractive indices between resin matrix and filler. As mentioned before, different shades of composite resins have different compositions of filler contents and nano-filler particle sizes. The lower the filler size and content of the composite resins, the more translucent the material.
Scattering anisotropy factor (g)
In this study, goniometric measurements were made for three wavelengths in the visible range, allowing a spectral characterization of the materials studied. Taking this into account, to compute the g factor that represents the phase function, researchers considered the average between the two values corresponding to both angular directions of rotation.
Many works deal with scattering anisotropy in turbid media but do not generally consider the asymmetry of experimental phase functions in the recovery of the g factor by goniometric measurements [23,24,25].
Scattering in a heterogeneous system, as enamel prisms surrounded by a fluid medium (e.g., water), is a function caused by the difference in refractive indices of two components. The refractive index of dental enamel [26] is approximately 1.7. Since the refractive index of water is 1.33 and air is 1.00, larger differences and greater scattering are produced at an enamel-air interface [27]. Even if different intensity is used between all samples, there is no difference in the light interaction between all dental tissues.
In a previous study [7] that used the same methodology, the scattering anisotropy factor showed similar spectral variations for all materials (dental-resin composites, human enamel, and zirconia ceramic) except for the human dentin (that may be due to the different internal structure of dentine, which is an anisotropic tissue compared to other materials investigated).
Limitations in the study included the following:
-
1.
This was an in vitro study and was difficult to replicate this type of experiment clinically.
-
2.
Using posterior teeth. When teeth are placed in the oral cavity, different light angulations are directed toward the posterior teeth and gives different results; however, the concept of this study can be applied to anterior teeth, as the light matching is not critical for posterior as much as anterior teeth.
-
3.
Using only one thickness. Thickness is a factor that influences light propagation through a material and different thicknesses need to be evaluated.
-
4.
Using only one type of composite (nano-filled resin-based composite). Different composites need to be evaluated, such as hybrid and micro-filled.
Future research also needs to be directed toward evaluating different types of materials for resin-based composites. Moreover, additional parameters should be measured for complete analysis of the light propagation. For example, scattering and backscattering coefficients play a significant role in light interactions with the matter. Additionally, thickness is an important factor for light propagation, and different thicknesses should be evaluated. Aging the samples should also be studied to evaluate the color stability of restorative materials.
Conclusions
This study identified characteristics of different RBC build-up techniques and compared the results to natural dental tissues. Findings from the study showed that no single monochromatic composite resin can completely replicate the complex orientation of color found in natural dental tissue, and it is necessary to select various colors when using artificial enamel and artificial dentin layers. In order to reconstruct the natural polychromatic effect, the layers also need to be irregular with undulated placement of varied composite resin colors. This composition allows optical properties of light passing through the natural tooth and the restoration composite to reflect, refract, absorb, and transmit according to the optical densities of the hydroxyapatite crystal, enamel rods, dentinal tubules, and restorative material, thus rendering the tooth multicolored.
Within the limitations of this study, the following attributes were revealed:
-
1.
None of the simple build-up techniques were able to reproduce optical properties seen in dental tissues within absorption (A), attenuation (K), transmission (T), and coefficient of light scattering (g).
-
2.
Both the T2 and T3 groups resulted in a similar pattern of light propagation.
-
3.
T2 and T3 showed closer patterns of light propagation when compared to natural dental tissues.
References
Sakaguchi RL, Powers JM (2012) Craig’s restorative dental materials, 13th edition. Br Dent J 213(2):90–90
Paravina RD (2004) Esthetic color training in dentistry. Elsevier Mosby, London
Lee YK (2008) Influence of filler on the difference between the transmitted and reflected colors of experimental resin composites. Dent Mater 24(9):1243–1247. https://doi.org/10.1016/j.dental.2008.01.014
Azzopardi N, Moharamzadeh K, Wood DJ, Martin N, van Noort R (2009) Effect of resin matrix composition on the translucency of experimental dental composite resins. Dent Mater 25(12):1564–1568. https://doi.org/10.1016/j.dental.2009.07.011
Arimoto A, Nakajima M, Hosaka K, Nishimura K, Ikeda M, Foxton RM, Tagami J (2010) Translucency, opalescence and light transmission characteristics of light-cured resin composites. Dent Mater 26(11):1090–1097. https://doi.org/10.1016/j.dental.2010.07.009
Grajower R, Wozniak WT, Lindsay JM (1982) Optical properties of composite resins. J Oral Rehabil 9(5):389–399. https://doi.org/10.1111/j.1365-2842.1982.tb01027.x
Johnston WM, Reisbick M (1997) Color and translucency changes during and after curing of esthetic restorative materials. Dent Mater 13(2):89–97. https://doi.org/10.1016/S0109-5641(97)80017-6
Yu B, Lee YK (2008) Differences in color, translucency and fluorescence between flowable and universal resin composites. J Dent 36(10):840–846. https://doi.org/10.1016/j.jdent.2008.06.003
Sidhu S, Ikeda T, Omata Y, Fujita M, Sano H (2006) Change of color and translucency by light curing in resin composites. Oper Dent 31(5):598–603. https://doi.org/10.2341/05-109
Fernandez-Oliveras A, Rubiño M, Perez MM (2012) Scattering anisotropy measurements in dental tissues and biomaterials. Journal of the European Optical Society - Rapid publications, Europe, v. 7, May. 2012. ISSN 1990-2573
Taroni P, Pifferi A, Torricelli A, Comelli D, Cubeddu R (2003) In vivo absorption and scattering spectroscopy of biological tissues. Photochem Photobiol Sci 2(2):124–129
Hariri I, Sadr A, Shimada Y, Tagami J, Sumi Y (2012) Effects of structural orientation of enamel and dentine on light attenuation and local refractive index: an optical coherence tomography study. J Dent 40(5):387–396. https://doi.org/10.1016/j.jdent.2012.01.017
Naeimi Akbar H, Moharamzadeh K, Wood DJ, Van Noort R (2012) Relationship between color and translucency of multishaded dental composite resins. International Journal of Dentistry 2012(5):1–5. https://doi.org/10.1155/2012/708032
Watts DC, Cash AJ (1994) Analysis of optical transmittance by 400–500nm visible light into aesthetic dental biomaterials. J Dent 22(112):7
Vanini L (1996) Light and color in anterior composite restorations. Pract Periodontics Aesthet Dent 8(7):673–682
de Araujo Junior EM, Baratieri LN, Monteiro Junior S, Vieira LC et al (2003) Direct adhesive restoration of anterior teeth: part 3. Procedural considerations. Pract Proced Aesthet Dent 15(6):433–437 quiz 438
Fahl N, Denehy GE, Jackson RD (1995) Protocol for predictable restoration of anterior teeth with composite resins. Pract Periodontics Aesthet Dent 7(8):13–21 quiz 22
Dietschi D, Ardu S, Krejci I (2006) A new shading concept based on natural tooth color applied to direct composite restorations. Quintessence Int 37(2):91–102
Villarroel M, Fahl N, De Sousa AM, De Oliveira OB (2011) Direct esthetic restorations based on translucency and opacity of composite resins. J Esthet Restor Dent 23(2):73–87. https://doi.org/10.1111/j.1708-8240.2010.00392.x
Vanini L (2012) Moving beyond classical shade guides to achieve natural restorations. Dental Tribune
Naeimi Akbar H, Moharamzadeh K, Wood DJ, Van Noort R (2012) Relationship between color and translucency of multishaded dental composite resins. Int J Dent 2012:708032. https://doi.org/10.1155/2012/708032
Kamishima N, Ikeda T, Sano H (2005) Color and translucency of resin composites for layering techniques. Dent Mater J 24(3):428–432. https://doi.org/10.4012/dmj.24.428
Steinke JM, Shepherd AP (1988) Comparison of Mie theory and the light scattering of red blood cells. Appl Opt 27:4027–4033. https://doi.org/10.1364/AO.27.004027
Sardar DK, S FS, Perez JJ (2001) Optical characterization of melanin. J Biomed Opt 6:404–411. https://doi.org/10.1117/1.1411978
Sardar DK, Yom RM, Tsin AT, Sardar R (2005) Optical scattering, absorption and polarization of healthy and neovascularized human retinal tissues. J Biomed Opt 10:051501. https://doi.org/10.1117/1.2065867
Houwink B (1974) The index of refraction of dental enamel apatite. Br Dent J 137:472–475. https://doi.org/10.1038/sj.bdj.4803346
Spitzer D, Bosch JT (1975) The absorption and scattering of light in bovine and human dental enamel. Springer Verlag 17:129–137
Funding
The work was supported by the Project Pool from ADEA (American Dental Education Association).
Author information
Authors and Affiliations
Ethics declarations
Conflict of interest
Author Hanan Elgendy declares that she has no conflict of interest. Author Rodrigo Rocha Maia declares that he has no conflict of interest. Author Fredrick Skiff declares that he has no conflict of interest. Author Gerald Denehy declares that he has no conflict of interest. Author Fang Qian declares that she has no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Elgendy, H., Maia, R.R., Skiff, F. et al. Comparison of light propagation in dental tissues and nano-filled resin-based composite. Clin Oral Invest 23, 423–433 (2019). https://doi.org/10.1007/s00784-018-2451-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-018-2451-9