Abstract
Objectives
The aim of the study was to investigate the caries-preventive effect of newly developed fluoride and fluoride-free toothpastes specially designed for erosion prevention. The hypothesis was that these products might also show superior caries-inhibiting effect than regular fluoride toothpastes, since they were designed for stronger erosive acid challenges.
Materials and methods
Enamel specimens were obtained from bovine teeth and pre-demineralized (pH = 4.95/21 days) to create artificial caries lesions. Baseline mineral loss (ΔZB) and lesion depth (LDB) were determined using transversal microradiography (TMR). Ninety specimens with a median ΔZB (SD) of 6027 ± 1546 vol% × μm were selected and randomly allocated to five groups (n = 18). Treatments during pH-cycling (14 days, 4 × 60 min demineralization/day) were brushing 2×/day with AmF (1400 ppm F−, anti-caries [AC]); AmF/NaF/SnCl2/Chitosan (700 ppm F−/700 ppm F−/3500 ppm Sn2+, anti-erosion [AE1]); NaF/KNO3 (1400 ppm F−, anti-erosion [AE2]); nano-hydroxyapatite-containing (0 ppm F−, [nHA]); and fluoride-free toothpastes (0 ppm F−, negative control [NC]). Toothpaste slurries were prepared with mineral salt solution (1:3 wt/wt). After pH-cycling specimens presenting lesion, surface loss (mainly by NC and nHA) were discarded. For the remaining 77 specimens, new TMR analyses (ΔZE/LDE) were performed. Changes in mineral loss (ΔΔZ = ΔZB − ΔZE) and lesion depth (ΔLD = LDB − LDE) were calculated.
Results
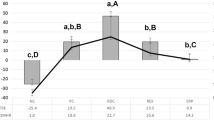
All toothpastes caused significantly less demineralization (lower ΔΔZ) than NC (p < 0.05, ANOVA) except for nHA. The fluoride toothpastes did not differ significantly regarding ΔΔZ and ΔLD (p > 0.05, ANOVA).
Conclusion/clinical relevance
While both anti-erosive and anti-caries toothpastes reduced mineral loss to a similar extent, the fluoride-free nano-hydroxyapatite-containing toothpaste seemed not to be suitable for inhibition of caries demineralization in vitro.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Toothpastes, one of the most widely practiced and effective way to deliver free or soluble fluoride, are probably the most common products in healthcare [1]. Since several years, however, fluoride-free toothpastes with other active components (i.e., nano-sized zinc-carbonate-hydroxyapatite or nano-hydroxyapatite (nHA)) have been marketed, claiming to be specifically effective against caries [2] or erosion [3].
Indeed, a few studies have indicated a significant remineralizing effect by nHA-containing toothpastes [4, 5]. The remineralizing potential of these new products was in the same order, although not significantly higher than that of fluoride. In a strongly remineralizing in vitro model, in which no pH-cycling was performed, it has been shown that a nHA-containing toothpaste (10 wt%) caused an enamel mineral gain, which was not significantly different than that of an amine fluoride toothpaste (1450 ppm F−) [4]. In situ, again, no significant difference in mineral gain has been shown by a nHA (10 wt%) and a sodium fluoride toothpaste (1100 ppm F−) [5]. However, analyzing nHA being incorporated in experimental pastes, more negative results have been observed [6]. For the experimental pastes containing 10 % as well as 20 % nHA, no significant difference could be observed for enamel subsurface demineralization compared both to no treatment and to placebo (paste without nHA and F−) [6]. Only when fluoride (0.2 % NaF) was combined to a nHA-containing (10 %) paste, a significant improvement of enamel remineralization could be observed, in situ. A reduction of demineralization using this combined nHA and fluoride treatment was still not achieved though [7].
Also for the use as solution, a significant remineralizing effect on artificial caries models has been observed [8]. When nHA was dissolved in solution (10 wt% nHA, pH = 4.0), significantly higher mineral gain could be observed compared to the negative control in a pH-cycling model [8]. Contrastingly, in a second study using the same model and the same test solution but with a neutral pH (10 wt% nHA, pH = 7.0), the nH was again effective in significantly increasing surface hardness as compared to a negative control, but less effective than the positive control, a neutral fluoride solution (1000 ppm F− as NaF) [9]. Furthermore, in a caries biofilm model, the daily treatment with nHA solution (10 wt%) also did not lead to an observable remineralization of the demineralized enamel [10]. In summary, although the gain in mineral content for fluoride-free nHA-containing toothpastes was as high as that of fluoride toothpastes in some studies [4, 5] and independently of the contrary results when nHA was incorporated in pastes or solutions [6, 9, 10], the designs of the majority of in vitro and in situ studies resulted in net remineralization models. Even the control groups remineralized. Only one study analyzed nHA under net demineralizing conditions on sound surfaces [6], and none of them analyzed the effect of nHA on pre-formed caries lesions and net demineralizing conditions yet. Thus, until now, there is very little information on the anti-caries effect of nHA-containing products especially under net demineralizing conditions.
Moreover, when nHA toothpastes were tested under strong demineralizing conditions, as in the frame-work of erosion, not as promising results have been observed. In a severe erosion model, the conventional fluoride toothpastes significantly reduced enamel tissue loss to 19–78 % of that of the control group (no treatment), whereas 10 wt% nHA could not significantly reduce enamel tissue loss [3]. Furthermore, 10 wt% nHA exhibited the overall highest enamel tissue loss and was significantly less effective than most of the NaF toothpastes [3].
Recently, also new agents have been incorporated to fluoride toothpastes, in order to either increase their preventive effect against dental erosion (like the inclusion of the metal ions as stannous, and biopolymers as chitosan) or decrease dentin hypersensitivity (like the inclusion of potassium nitrate (KNO3), strontium salts, bioglass, and arginine bicarbonate). The anti-erosive efficacy of commercial toothpastes containing some of these compounds has been demonstrated [3, 11–14], but up to now, the degree of efficiency of these toothpastes in a caries model has not been tested. Moreover, for toothpastes containing potassium nitrate, contradictory results related to its effects against erosion have been observed. Studies show sometimes small (19 % erosion reduction) but significantly better results than no treatment [3] and sometimes the opposite [15]. For stannous- and chitosan-containing toothpastes, significant effect on reduction of enamel erosive surface loss has been demonstrated [11, 12, 14], but to the best of our knowledge, its effect on caries model has not been published yet.
So far, there is very limited information about the anti-caries effect of nHA-containing products under demineralizing conditions, especially in relation to conventional fluoride compounds. Thus, the aim of this study was to investigate the caries-protective effect of newly developed fluoride and fluoride-free toothpastes specially designed for erosion prevention using a pH-cycling model causing net demineralization. Since some of these new toothpastes contain other active ingredients but no fluoride, and additionally the acid challenges during erosive episodes are stronger than in the caries process, it was hypothesized that no significant differences on inhibition of demineralization would be observed between the anti-caries and anti-erosive toothpastes, but for all compared with a fluoride-free control.
Materials and methods
A summary of the whole experimental set-up is described in a flowchart (Fig 1).
Specimens preparation
Bovine incisors were obtained from freshly slaughtered cattle (negative BSE test) and stored in 0.08 % thymol. Two hundred enamel specimens (5 mm × 4 mm × 3 mm) were prepared [16] (Fig. 2a). After embedding in acrylic resin (Technovit 4071; Heraus Kulzer, Hanau, Germany), enamel surfaces were ground flat and polished (waterproof silicon carbide papers, FEPA grit sizes: 800, 1200, 2400, 4000; Struers).
a Specimen preparation. (a) Frontal view of bovine front tooth; (b) separation of crown and root; (c) and (d) cuts perpendicular and parallel to the long axis of the tooth crown; (e) obtained specimens(5 mm × 4 mm × 3 mm); (f) specimen covered with resin; (g) pre-demineralized specimen, (control area (red) and treatment area); and (h) obtainment of the 100 μm-slices for baseline TMR analysis and submission of the other part of the specimen to pH-cycling. b Specially developed toothbrush holder to assure a standardized brushing force of 1.5 N (150 g). Before each ten measurements, brushing force was controlled using a laboratory balance. In order to cover the specimens, 25 ml of slurries were needed
Lesion formation
Half of the enamel surfaces were covered with a flow composite resin (Tetric EvoFlow; A4, Ivoclar Vivadent AG, Schaan, Principality of Liechtenstein) in order to assure enough mechanical and acid-resistance for the untreated control area. The other half remained uncovered (treatment area). To create artificial enamel caries lesions in uncovered areas, specimens were stored in a demineralization solution for 21 days (2.5 ml solution/mm2 enamel surface) [17]. The solution contained 50 mM acetic acid, 3 mM CaCl2 H2O, 3 mM KH2PO4, 6 μM methylhydroxydiphosphonate, and traces of thymol (pH 4.95; 37 °C). During that period, the pH was monitored daily and, if necessary, adjusted with small amounts of either 10 % HCl or 10 mM KOH to maintain a constant pH value [17].
After demineralization of the specimens, artificial carious lesions with intact surfaces were observed in all specimens. In order to calculate baseline mineral loss and lesion depth, thin slices of 100 μm (±10 μm) of each partially demineralized enamel specimen were cut perpendicular to the surface, as described below. These slices were prepared for transversal microradiographic (TMR) analysis in order to select specimens with comparable and homogeneous demineralization. In this way, 90 specimens with a mean (±SD) baseline mineral loss (ΔZB) of 6027 ± 1546 vol% × μm and a mean lesion depth (LDB) of 143 ± 28 μm were chosen from the 200 specimens originally prepared [18].
Surface treatment
The obtained specimens were randomly divided into five groups, which received different fluoride treatments: fluoride-free toothpaste (0 ppm F−), as negative control [NC]; AmF (1400 ppm F−) anti-caries [AC]; AmF/NaF/SnCl2/Chitosan (700 ppm F−/700 ppm F−/3500 ppm Sn2+), anti-erosion [AE1]; NaF/KNO3 (1400 ppm F−), anti-erosion [AE2]; and nano-hydroxyapatite-containing (0 ppm F−) [NH] toothpastes (Table 1).
Toothpaste slurries and brushing procedure
From the toothpastes, slurries were prepared by mixing with the mineral salt solution (1 part toothpaste to 3 parts mineral solution, by weight). The slurries were freshly prepared at the beginning of each experimental day [3]. The pH values of all solutions were monitored with a pH-sensitive electrode.
Twice daily, all groups were immersed in toothpaste slurries for 1 min and 55 s and brushed for 5 s. The mineral solution was composed of 4.08 mmol H3PO4, 11.90 mM NaHCO3, 20.10 mM KCl, and 1.98 mM CaCl2 [19]. The mineral solution is supersaturated with respect to hydroxyapatite and has a pK-pI of 10.37 [3]. The brushing force was 1.5 N (150 g), standardized using a customized toothbrush holder (Fig. 2b) and a powered toothbrush connected to an oscillating-rotating brush head (Braun Oral B Professional Care 8500 + Brush Head: Precision Clean, Oral B, Procter & Gamble GmbH, Germany) was used [20]. The most external and longer bristles were removed from the brushing heads and only the center rounded-end bristles fitting exactly the exposed enamel area were maintained. In order to simulate the time needed to brush one tooth, the brushing time per specimen was calculated dividing the mean brushing time of adults [21] by the total number of teeth (28) excluding the thirds molars.
pH-cycling conditions
After surface treatment, specimens were submitted to a pH-cycling for 14 days [17]. The pH-cycling involved four demineralization times of 1 h each (total 4 h/day) and four remineralization times of at least 2 h during the day and a longer overnight period (total 18 h/day). Brushing was performed twice daily in the periods between 08:00–09:00 h and 20:00–21:00 h always after a demineralization phase (total brushing time all 90 specimens 2 h/day). The demineralization contained 3 mM CaCl2 * 2 H2O, 3 mM KH2PO4, 50 mM CH3COOH (lactic acid), and 6 μM methylhydroxydiphosphonate (MHDP), pH 5 (37 °C). The remineralization solution contained 1.5 mM CaCl2 * 2 H2O, 0.9 mM KH2PO4, and 20 mM N-2-hydroxyethylpiperazine-N′2-ethanesulfonic acid (HEPES) as buffer, pH 7 (37 °C). For both solutions, the pH was adjusted with small amounts of 10 % HCl or 10 mM KOH to maintain a constant pH [17]. The pH-cycling solutions were refreshed daily. The amount of each solution was large enough to prevent the solutions from becoming saturated with or depleted of mineral ions (2.5 ml solution/mm2 enamel surface).
Determination of free fluoride in the slurries
For the fluoride-containing toothpastes, total soluble fluoride concentrations in the slurries were determined directly and 12 h after preparation. Two hundred milligrams of the toothpaste slurries (1 part toothpaste to 3 parts mineral solution, by weight) were diluted in 100 ml distilled water at room temperature. Four milliliters of the diluted slurries were centrifuged at 10,000 g for 10 min and 1 ml of the supernatant was added to 1 ml TISAB II (Thermo Fisher Scientific, Beverly, Mass., USA). To calibrate the electrode, four fluoride solutions (3.8, 1.9, 0.38, and 0.19 mg/l) were prepared, since these concentrations are in the same range of the expected sample concentrations. After calibration, the fluoride concentration of the toothpastes were determined using a fluoride-sensitive electrode (type 96–09 BNC; Thermo Fisher Scientific) [3, 22, 23]. Analyses were made in triplicate.
Transversal microradiography analysis
After the pH-cycling, from each specimen, a slice of approximately 300-μm thickness (Exakt GmbH, Norderstedt, Germany) was obtained and subsequently ground and polished to a thickness of 100 μm (±10 μm) using waterproof silicon carbide papers (FEPA grit sizes: 800, 1200, 2400, 4000; Struers). The parallelism of the specimens was tested with a digital micrometer with a precision of 0.001 mm (Mitutoyo, Japan). Contact microradiographs of the enamel specimens were obtained with a nickel-filtered copper (CuKa) X-ray source (PW 1730; Philips, Kassel, Germany) operating at 20 kV and 20 mA. The radiation source-to-film distance was 28 cm. The exposure time was 10 s and a high-resolution film (Motion picture fine grain positive film 71337″; FUJIFILM Corporation Japan) was used and developed under standardized conditions according to the manufacturer’s recommendations.
Microradiographs were digitalized by an image-analyzing system (Diskus software version 4.80; Königswinter, Germany) that is interfaced to a universal microscope (Leica DMRX; Germany) and a personal computer. A transversal microradiography (TMR) software (Version 5.25 by Joop de Vries, Groningen, Netherlands) was used to calculate the mineral loss (ΔZB/ΔZE) and the lesion depth (LDB/LDE) before and after pH-cycling.
Calculation of integrated mineral loss and lesion depth
The mineral content was calculated by the TMR software based on the specimen’s gray levels. The average mineral content of sound enamel was assumed to be 87 vol%, and the mineral density of sound enamel to be 2.88 g/cm3, as measured by previous studies [24, 25]. The lesion depth was calculated using a threshold of 95 % of the mineral content of sound enamel (i.e., 82.7 %). Thus, integrated mineral loss (ΔZ), lesion depth (LD), and ‘R’ value (being the ratio of mineral loss (∆Z) to lesion depth (LD)) could be calculated [26, 27].
Baseline mineral loss (ΔZB) and lesion depth (LDB) of pre-demineralized surfaces were subtracted from the respective values after pH-cycling, named here ‘effect’ (ΔZE, LDE) [28, 29]. Changes in mineral loss (ΔΔZ = ΔZB − ΔZE), lesion depth (ΔLD = LDB − LDE) and ‘R’ values were then calculated.
Statistical analysis
Data were analyzed using SPSS statistical software (SPSS 22.0; SPSS, Munich, Germany). Before analysis, all variables were tested for normal distribution (Shapiro-Wilk test). Within one experimental group, changes in mineral loss and lesion depth before and after pH-cycling (ΔZB vs. ΔZE and LDB vs. LDE) were analyzed using t test. Analysis of variance (ANOVA) was used for pair-wise multiple-comparisons to detect differences in changes of mineral loss (∆∆Z) and lesion depth (ΔLDE) between treatments. All tests were performed at a 5 % level of significance.
Results
Free fluoride in the slurries
The highest amount of total soluble fluoride was detected for AE1, both immediately and 12 h after slurry preparation. For NC and nHA very small amounts of fluoride (<2 ppm) and no fluoride were detected immediately and after 12 h after slurry preparation, respectively (Table 2).
TMR Analysis
After pH-cycling, specimens presenting lesion surface loss (mainly by NC and nHA) were discarded and for the remaining 77 specimens, new TMR analyses (ΔZE/LDE) were performed.
No significant difference between the groups could be observed for ΔZB (p > 0.05, ANOVA). After pH-cycling, specimens of NC and nHA showed a significantly increase in mineral loss (p < 0.05, t test), whereas for AC, AE1, and AE2, a small non-significant increase could be observed (p > 0.05, t test). Figure 3 shows the representative TMR microradiographs and the respective mineral distribution profiles of the lesions before and after pH-cycling.
Representative TMR images of the lesions before (left) and after pH-cycling (middle) as well as the respective mineral distribution profiles (right). In the diagrams, the gray line represents the mineral distribution profile of the lesion at baseline and the dark black line after pH-cycling (effect). All the mineral content assessments were conducted with TMR/WIM Calculation Program
For comparisons between the groups, all toothpastes caused significantly lower ΔΔZ (SD) than NC (−4557 ± 2178 vol% × μm) (p < 0.05, ANOVA), except for nHA (−2119 ± 1896 vol% × μm) (p = 0.114, ANOVA). Both AE’s and AC toothpaste did not differ significantly in ΔΔZ (p > 0.05, ANOVA) (Table 3).
With respect to lesion depth, only AE2 showed statistically significantly lower ΔLD means than NC (p = 0.039, ANOVA). Among all other groups, no statistically significant differences were detected (p > 0.05, ANOVA) (Table 3).
Discussion
Most of the anti-erosive toothpastes significantly reduced enamel carious mineral loss as compared to the negative control, but they were not significantly superior to the conventional AmF toothpaste. Thus, the null hypothesis was partially accepted. The only exception is the nHA toothpaste that did not significantly reduced enamel demineralization as compared to the negative control. On the one hand, this is in agreement with the findings of a recent in situ study, in which an experimental nHA paste (not a toothpaste) was not able to decrease enamel demineralization [7]. On the other hand, this is in contrary to some previous studies that showed a significant remineralizing effect for nHA solutions [8, 9] and also for a nHA toothpaste [4]. However, the latter studies analyzed only the remineralizing effect of nHA, and this effect has also never been tested in controlled clinical trials. So, it is still unclear how well these compounds would work under more complex conditions of real oral environment. Furthermore, in a biofilm model simulating more clinical variables, as the presence of a plaque biofilm over the tooth surface, remineralization of previously demineralized enamel could also not be observed [10].
It can be speculated that one of the reasons, why the nHA toothpaste did not show a significant anti-caries effect in the present study, could be the neutral pH of the formulation (nHA: pH 7.5) and the delivery form. It is known that, firstly, solutions normally have a stronger effect on influencing tooth de- and remineralization than toothpastes [1], and secondly, it has been demonstrated that, at least for nHA solutions, a threefold increase of enamel mineral gain (593.6 to 1837.8 vol% × μm) can be observed, when the pH of the solution is decreased from 7 to 4 [8]. Besides that, the positive remineralizing effect observed by a recent nHA toothpaste study [4] might be related to the type of pH-cycling model used (without demineralization periods resulting in net remineralization). In the presence of free fluoride, the enamel critical pH for demineralization shifts approximately 0.5–1.0 units to a more acidic critical pH [30]. As fluoride-free compounds do not have this action, it can be expected that they result in a worse inhibition of demineralization than that of a fluoride toothpaste [30]. Under constant remineralization conditions (without any demineralization periods) [4], this (unfavorable) effect, of course, cannot be observed at any time.
Two of the fluoride compounds tested here (sodium fluoride and amine fluoride) have proved to be clinically effective [31]. Indirect evidence exists also for the stannous-containing fluoride formulation, if the clinical studies with stannous fluoride are considered [31–33]. However, there is currently no clinical study providing a direct comparison of their anti-caries efficacy. Here, under in vitro conditions, a similar reduction of further mineral loss between the three types of fluoride toothpastes (AmF, AmF/NaF/SnCl2/Chitosan, NaF/KNO3) having similar free fluoride content could be observed. Thus, the results indicate that the preventive effect of toothpastes may be more related to the amount of free fluoride than to the type of fluoride compound. Similar findings have also been found in a meta-analysis, showing that the main type of fluoride compounds did not influence the magnitude of the treatment effect [31].
The observed reduction of enamel demineralization for all three fluoride-containing toothpastes (AmF, AmF/NaF/SnCl2/Chitosan, and NaF/KNO3) tested might be related, though, to different mechanisms of action, since they contain different fluoride compounds and other active ingredients. One of the mechanisms, through which fluoride interferes with the dynamics of dental caries formation or progression, is the formation of different fluoride reservoirs [34]. However, this adsorbed fluoride (reservoir) is presumed to exhibit the main effect for caries prevention, when solely amine or sodium fluoride toothpastes are used [34]. For the Sn-containing products, inhibition of enamel acid dissolution occurs actually through deposition of an amorphous Sn-rich layer over the surface, as well as the incorporation of Sn into enamel [35]. Additionally, chitosan, the other active product present in the AmF/NaF/SnCl2/Chitosan toothpaste, has an anti-demineralization property, being able to significantly inhibit phosphorous release under pH-cycling conditions [36]. The combination of chitosan and Sn, as in the toothpaste formulation tested, results in a synergistic preventive effect at least for erosion [3, 11, 12]. If this is also true for carious conditions is yet to be investigated. In the present study, however, it did not result in a significantly higher preventive effect than the obtained with a conventional AmF toothpaste as well as to the NaF/KNO3 product.
Another point to be considered is that some specimens of groups NC and nHA presented lesion surface loss and had to be discarded. This might be interpreted as an indicator for abrasive losses due to abrasive ingredients or brushing procedure (force/movement), as well as the reduced presence of free fluoride at the specimen-solution interface. Most probably, surface losses observed in NC and nHA were not caused by the effect of brushing alone. Since, the same oscillating-rotating movement and brushing force (1.5 N) were used for all specimens and not all groups showed lesion surface loss. In this case, it can be speculated that the absence of fluoride was a greater influencing factor, as the lesion surface becomes less mineralized in the absence of fluoride [37]. Only in the special case of the nHA toothpaste, not only the absence of fluoride but probably also the abrasive ingredients played an important role in the observed effects. As a recent study showed that the nHA toothpaste had a three to nine times higher RDA value as compared to the same toothpastes tested here (AmF, AmF/NaF/SnCl2/Chitosan, NaF/KNO3) [14].
The study design chosen represent a relatively mild demineralizing model being intended to result in (slight) net demineralization, even for the fluoride groups. This should simulate the clinical situation of patients at high caries risk, as for example, patients with a frequent intake of readily fermentable carbohydrates. Besides, as in the natural caries process, in the present model demineralizing challenges were followed by remineralizing phases, allowing the fluoride ion to have an effect on both phases. Both the number of demineralization phases (6× demin/day) as well as the total demineralization time per day (4 h/day) was similar to other pH-cycling studies [38, 39]. These conditions resulted in subsurface initial caries lesions showing net demineralization in our pilot tests (data not shown), so this model fulfilled the conditions intended to be simulated. Nevertheless, it is still only an in vitro pH-cycling model, which only partly resembles the clinical situation. It has, however, the advantage of being ideal for an initial screening of possible effects of new therapies, before more time- and resources-consuming in situ studies can be conducted [32, 40]. For the simulation of toothbrushing conditions, a powered toothbrush with rotating-oscillating movement under a controlled and constant brushing force of only 1.5 N was used. This in contrast to some previous (erosive) in vitro studies (using linear movements and 2.0–2.5 N) [12, 14], but in the range of values measured during patient’s brushing (linear strokes/1.5–3 N) [21]. Nonetheless, previous studies indicated that powered toothbrushes produce significantly higher degrees of enamel abrasion [41]. Considering this and the fact that a powered toothbrush was used here, the lowest brushing force recommended as clinically similar, namely 1.5 N, was used to avoid excessive surface abrasion [42, 43].
With the present set-up, anti-caries properties of different anti-erosive toothpastes could be analyzed under highly standardized conditions. However, the chosen study design could not take all oral factors into account. The complexity of any tooth–pellicle–plaque–saliva interface, for example, was not simulated [44]. Indeed, both saliva as well as the biofilm has been shown to modulate the effect of nHA products. The salivary proteins and the plaque biofilm can retain the nano-HA precipitates for a longer time over the tooth surfaces, creating calcium and phosphate reservoirs [7, 10]. Recently, an in vitro study demonstrated that nHA treatment greatly increased the calcium content of the Streptococcus mutans biofilm (eightfold higher than the NaF treatment), which theoretically should clinically result in supersaturation of the plaque fluid. So it is reasonable to believe that if the biofilm was also simulated here, possibly a little less demineralization would be observed for the nHA toothpaste. However, in the mentioned study, even under this positive condition (supersaturated plaque biofilm), the nHA treatment did not lead to the observable remineralization of demineralized enamel [10]. Thus, a complete change of the nHA-toothpaste results, if the biofilm was also simulated here, seems, at least, improbable.
The initial artificial caries lesions obtained in our study were created using the method described by Buskes et al. [17] and presented the same characteristics as natural ones. Such natural enamel white-spot lesions present normally more porous, though intact surface layer, covering a demineralized subsurface area, presenting 10–70 vol% of mineral content [45]; characteristics which were also observed here (Fig. 3). Besides that, recent TMR analyses of natural enamel lesions have shown deeper mean lesion depth, but a mean mineral loss (SD) of 6691 (5922) vol% × μm [46], which is quite similar to that of our baseline lesions (ΔZB = 6027 ± 1546 vol% × μm). Thus, it seems that the lesions formed here mimic the natural ones, and this contributes for the clinical relevance of our model. Another point to be commented is the use of bovine enamel as substrate. These teeth are more porous and present a higher rate of demineralisation progression, expressed as faster lesion formation than human enamel [47]. However, bovine teeth are easier to obtain, present the same mechanism of caries formation, and have a more homogeneous mineralization pattern, which results in a more consistent experimental response [48]. Therefore, they are considered as a suitable substrate for anti-caries in vitro and in situ studies.
To the best of our knowledge, no previous research paper compared the efficacy of the toothpastes, tested in the present study, in a caries model. However, there are some studies testing their efficacy under erosion conditions, which represent a stronger acid challenge for them. The observation of these studies shows that, at least regarding the nHA toothpaste, the same tendency for not causing significant reduction of enamel demineralization can be observed. In one of the studies, when toothbrushing was also simulated, the 10 wt% nHA toothpaste could not significantly reduce enamel surface loss, while the NaF/KNO3 and other fluoride toothpastes did [3]. Testing the effects in dentin, it has been observed that the 10 wt% nHA toothpaste could indeed cause a low but significant reduction in erosive surface loss compared to no treatment. However, this effect was also significantly lower than the protective effect achieved with both a NaF/KNO3 and a AmF/NaF/SnCl2/Chitosan toothpaste [14]. Thus, AmF, AmF/NaF/SnCl2/Chitosan, and NaF/KNO3 not only have a more promising anti-caries (as shown in the present study) but also a stronger erosion-protective effect compared to nHA.
Based on the results, both anti-erosive (AmF/NaF/SnCl2/Chitosan and NaF/KNO3) and the anti-caries (AmF) toothpastes reduced mineral loss to a similar extent and seem to be suitable for caries inhibition, in vitro. However, the nano-hydroxyapatite-containing toothpaste could not significantly inhibit caries progression in a bacteria-free and demineralizing pH-cycling model. Thus, care should be taken regarding patient recommendations and anti-caries marketing claims of this toothpaste, since its anti-caries benefits seem not to be fully proven.
References
Lippert F (2013) An introduction to toothpaste—its purpose, history and ingredients. Monogr Oral Sci 23:1–14. doi:10.1159/000350456
Lynch RJ, Smith SR (2012) Remineralization agents—new and effective or just marketing hype? Adv Dent Res 24:63–67. doi:10.1177/0022034512454295
Ganss C, Lussi A, Grunau O, Klimek J, Schlueter N (2011) Conventional and anti-erosion fluoride toothpastes: effect on enamel erosion and erosion-abrasion. Caries Res 45:581–589. doi:10.1159/000334318
Tschoppe P, Zandim DL, Martus P, Kielbassa AM (2011) Enamel and dentine remineralization by nano-hydroxyapatite toothpastes. J Dent 39:430–437. doi:10.1016/j.jdent
Najibfard K, Ramalingam K, Chedjieu I, Amaechi BT (2011) Remineralization of early caries by a nano-hydroxyapatite dentifrice. J Clin Dent 22:139–143
Comar LP, Souza BM, Gracindo LF, Buzalaf MA, Magalhaes AC (2013) Impact of experimental nano-HAP pastes on bovine enamel and dentin submitted to a pH cycling model. Braz Dent J 24:273–278. doi:10.1590/0103-6440201302175
Souza BM, Comar LP, Vertuan M, Fernandes Neto C, Buzalaf MA, Magalhaes AC (2015) Effect of an experimental paste with hydroxyapatite nanoparticles and fluoride on dental demineralisation and remineralisation in situ. Caries Res 49:499–507. doi:10.1159/000438466
Huang S, Gao S, Cheng L, Yu H (2011) Remineralization potential of nano-hydroxyapatite on initial enamel lesions: an in vitro study. Caries Res 45:460–468. doi:10.1159/000331207
Huang SB, Gao SS, Yu HY (2009) Effect of nano-hydroxyapatite concentration on remineralization of initial enamel lesion in vitro. Biomed Mater 4:034104. doi:10.1088/1748-6041/4/3/034104
Zhang M, He LB, Exterkate RA, Cheng L, Li JY, Ten Cate JM, Crielaard W, Deng DM (2015) Biofilm layers affect the treatment outcomes of NaF and nano-hydroxyapatite. J Dent Res 94:602–607. doi:10.1177/0022034514565644
Ganss C, von Hinckeldey J, Tolle A, Schulze K, Klimek J, Schlueter N (2012) Efficacy of the stannous ion and a biopolymer in toothpastes on enamel erosion/abrasion. J Dent 40:1036–1043. doi:10.1016/j.jdent.2012.08.005
Carvalho TS, Lussi A (2014) Combined effect of a fluoride-, stannous- and chitosan-containing toothpaste and stannous-containing rinse on the prevention of initial enamel erosion-abrasion. J Dent 42:450–459. doi:10.1016/j.jdent.2014.01.004
Hara AT, Kelly SA, Gonzalez-Cabezas C, Eckert GJ, Barlow AP, Mason SC, Zero DT (2009) Influence of fluoride availability of dentifrices on eroded enamel remineralization in situ. Caries Res 43:57–63. doi:10.1159/000201591
Aykut-Yetkiner A, Attin T, Wiegand A (2014) Prevention of dentine erosion by brushing with anti-erosive toothpastes. J Dent 42:856–861. doi:10.1016/j.jdent.2014.03.011
Kato MT, Lancia M, Sales-Peres SH, Buzalaf MA (2010) Preventive effect of commercial desensitizing toothpastes on bovine enamel erosion in vitro. Caries Res 44:85–89. doi:10.1159/000282668
Meyer-Lueckel H, Paris S (2008) Progression of artificial enamel caries lesions after infiltration with experimental light curing resins. Caries Res 42:117–124. doi:10.1159/000118631
Buskes JA, Christoffersen J, Arends J (1985) Lesion formation and lesion remineralization in enamel under constant composition conditions. A new technique with applications. Caries Res 19:490–496
Lippert F, Lynch RJ, Eckert GJ, Kelly SA, Hara AT, Zero DT (2011) In situ fluoride response of caries lesions with different mineral distributions at baseline. Caries Res 45:47–55. doi:10.1159/000323846
Gerrard WA, Winter PJ (1986) Evaluation of toothpastes by their ability to assist rehardening of enamel in vitro. Caries Res 20:209–216
Esteves-Oliveira M, Pasaporti C, Heussen N, Eduardo CP, Lampert F, Apel C (2011) Prevention of toothbrushing abrasion of acid-softened enamel by CO2 laser irradiation. J Dent 39:604–611. doi:10.1016/j.jdent.2011.06.007
Ganss C, Schlueter N, Preiss S, Klimek J (2009) Tooth brushing habits in uninstructed adults–frequency, technique, duration and force. Clin Oral Investig 13:203–208. doi:10.1007/s00784-008-0230-8
Tenuta LM, Cury JA (2013) Laboratory and human studies to estimate anticaries efficacy of fluoride toothpastes. Monogr Oral Sci 23:108–124. doi:10.1159/000350479
Meyer-Lueckel H, Wierichs RJ, Gninka B, Heldmann P, Dorfer CE, Paris S (2015) The effect of various model parameters on enamel caries lesions in a dose-response model in situ. J Dent 43:1261–1267. doi:10.1016/j.jdent.2015.08.003
Angmar B, Carlstrom D, Glas JE (1963) Studies on the ultrastructure of dental enamel V. The mineralization of normal human enamel. I J Ultrastruct Res 8:12–23
De Josselin de Jong E, ten Bosch JJ, Noordmans J (1987) Optimised microcomputer-guided quantitative microradiography on dental mineralised tissue slices. Phys Med Biol 32:887–899
Arends J, Dijkman T, Christoffersen J (1987) Average mineral loss in dental enamel during demineralization. Caries Res 21:249–254
Theuns HM, van Dijk JW, Driessens FC, Groeneveld A (1984) The surface layer during artificial carious lesion formation. Caries Res 18:97–102
Magalhaes AC, Moron BM, Comar LP, Wiegand A, Buchalla W, Buzalaf MA (2009) Comparison of cross-sectional hardness and transverse microradiography of artificial carious enamel lesions induced by different demineralising solutions and gels. Caries Res 43:474–483. doi:10.1159/000264685
Meyer-Lueckel H, Wierichs RJ, Schellwien T, Paris S (2015) Remineralizing efficacy of a CPP-ACP cream on enamel caries lesions in situ. Caries Res 49:56–62. doi:10.1159/000363073
Amaechi BT, van Loveren C (2013) Fluorides and non-fluoride remineralization systems. Monogr Oral Sci 23:15–26. doi:10.1159/000350458
Marinho VC, Higgins JP, Sheiham A and Logan S (2003) Fluoride toothpastes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev:CD002278. doi:10.1002/14651858.CD002278
Zero DT (2006) Dentifrices, mouthwashes, and remineralization/caries arrestment strategies. BMC Oral Health 6(Supp 1):S9. doi:10.1186/1472-6831-6-S1-S9
Wong MC, Clarkson J, Glenny AM, Lo EC, Marinho VC, Tsang BW, Walsh T, Worthington HV (2011) Cochrane reviews on the benefits/risks of fluoride toothpastes. J Dent Res 90:573–579. doi:10.1177/0022034510393346
Arends J, Christoffersen J (1990) Nature and role of loosely bound fluoride in dental caries. J Dent Res 69:601–605 discussion 634-6
Schlueter N, Hardt M, Lussi A, Engelmann F, Klimek J, Ganss C (2009) Tin-containing fluoride solutions as anti-erosive agents in enamel: an in vitro tin-uptake, tissue-loss, and scanning electron micrograph study. Eur J Oral Sci 117:427–434. doi:10.1111/j.1600-0722.2009.00647.x
Arnaud TM, de Barros NB, Diniz FB (2010) Chitosan effect on dental enamel de-remineralization: an in vitro evaluation. J Dent 38:848–852. doi:10.1016/j.jdent.2010.06.004
ten Cate JM, Duijsters PP (1982) Alternating demineralization and remineralization of artificial enamel lesions. Caries Res 16:201–210
ten Cate JM, Buijs MJ, Miller CC, Exterkate RA (2008) Elevated fluoride products enhance remineralization of advanced enamel lesions. J Dent Res 87:943–947
ten Cate JM, Exterkate RA, Buijs MJ (2006) The relative efficacy of fluoride toothpastes assessed with pH cycling. Caries Res 40:136–141
Lippert F, Juthani K (2015) Fluoride dose-response of human and bovine enamel artificial caries lesions under pH-cycling conditions. Clin Oral Investig 19:1947–1954. doi:10.1007/s00784-015-1436-1
Wiegand A, Begic M, Attin T (2006) In vitro evaluation of abrasion of eroded enamel by different manual, power and sonic toothbrushes. Caries Res 40:60–65. doi:10.1159/000088908
Ganss C, Schlueter N, Hardt M, von Hinckeldey J, Klimek J (2007) Effects of toothbrushing on eroded dentine. Eur J Oral Sci 115:390–396. doi:10.1111/j.1600-0722.2007.00466.x
Vieira A, Overweg E, Ruben JL, Huysmans MC (2006) Toothbrush abrasion, simulated tongue friction and attrition of eroded bovine enamel in vitro. J Dent 34:336–342. doi:10.1016/j.jdent.2005.07.010
ten Cate JM, Arends J (1978) Remineralization of artificial enamel lesions in vitro. II. Determination of activation energy and reaction order. Caries Res 12:213–222
Arends J, Christoffersen J (1986) The nature of early caries lesions in enamel. J Dent Res 65:2–11
Meyer-Lueckel H, Paris S, Kielbassa AM (2007) Surface layer erosion of natural caries lesions with phosphoric and hydrochloric acid gels in preparation for resin infiltration. Caries Res 41:223–230. doi:10.1159/000099323
Featherstone JD, Mellberg JR (1981) Relative rates of progress of artificial carious lesions in bovine, ovine and human enamel. Caries Res 15:109–114
Mellberg JR (1992) Hard-tissue substrates for evaluation of cariogenic and anti-cariogenic activity in situ. J Dent Res 71:913–919
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflict of interest.
Funding
The study was funded by both institutions involved and Mrs. Santos was granted a scholarship from the Science Without Borders (CSF) program from CNPq, Brazil (process number 238553/2012-4).
Ethical approval
This article does not contain any studies with human participants or animals performed by any authors.
Informed consent
For this type of study, formal consent is not required.
Additional information
R. J. Wierichs and J. A. Rodrigues contributed equally to the study
Rights and permissions
About this article
Cite this article
Esteves-Oliveira, M., Santos, N.M., Meyer-Lueckel, H. et al. Caries-preventive effect of anti-erosive and nano-hydroxyapatite-containing toothpastes in vitro. Clin Oral Invest 21, 291–300 (2017). https://doi.org/10.1007/s00784-016-1789-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-016-1789-0