Abstract
Objectives
Cancer progression is influenced by tumor microenvironment and communication of stromal cells and tumor cells. Interactions may enhance epithelial-mesenchymal transition (EMT) of tumor cells through signaling proteins such as Wnt/beta-catenin and matrix metalloproteinases (MMP), as well as loss of cellular integrity, which affects invasion, progression, and metastasis of head and neck squamous cell carcinoma (HNSCC). In this study, we are testing the hypothesis that interactions of human mesenchymal stromal cells (MSCs) with HNSCC might influence the expression of markers of EMT and tumor progression by co-culturing human MSC with the PCI-13 HNSCC line.
Materials and methods
Pooled MSCs were derived from the iliac bone marrow of seven patients and co-cultured in transwell permeable membrane wells with tumor cells of the established HNSCC cell line PCI-13 (UICC: T3, N1, M0). MSCs were characterized through fluorescence-activated cell sorting (FACS) analysis. Expression of Wnt3, E-cadherin, beta-catenin, MMP14, cathepsin b, and ETS1 was assessed by quantitative RT-PCR.
Results
We were able to show that co-culture of MSCs and PCI-13 leads to a significantly reduced expression of Wnt3, MMP14, and beta-catenin compared to controls, whereas the expression of cathepsin b and ETS1 was not significantly different between co-cultures and controls.
Conclusion
Our results suggest that the interaction between MSCs and PCI-13 may suppress EMT in cancer cells.
Clinical relevance
The influence of MSCs can suppress the onset of EMT in HNSCC, affecting tumor progression and therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, the tumor microenvironment and the communication between stromal cells and tumor cells have been identified as important factors in cancer progression. Several cross-talk routes between tumor cells and stromal cells are known to activate specific signaling pathways [1]. Carcinoma-associated fibroblasts (CAFs) have been evaluated as elements of the extracellular environment of tumors. Experimental evidence suggests that interactions of CAF/mesenchymal stromal cell (MSC) and tumor cells are found at the invasive edge of cancer, affecting tumor transition, invasive transformation, and progression [2]. Recent in vitro studies have shown an effect of MSCs on the proliferation of human cancer cells [3, 4]. This may become clinically relevant if reconstructive procedures are considered through tissue-engineered constructs after ablative surgery for malignant diseases. Unfortunately, little is known about the signaling pathways through which MSCs may influence tumor progression [5, 6].
One pathway of possible interactions may involve epithelial-mesenchymal transition (EMT) through signaling proteins such as Wnt/beta-catenin and matrix metalloproteinases (MMPs). Together, with the loss of E-cadherin, they are considered to affect tumor invasion, progression, and metastasis of head and neck squamous cell carcinomas (HNSCC) [7–10]. The deregulation of the Wnt/beta-catenin signaling pathway during EMT inhibits the adenomatous polyposis coli (APC)/glycogen synthase kinase 3 (GSK3) complex, which is involved in the degradation of beta-catenin, leading to a further increase of beta-catenin activity [11]. Nuclear transition of beta-catenin, moreover, increases the transcription of proteolytic enzymes like membrane-type MMP14 [12, 13]. Finally, MMP14 can promote tumor growth and invasive proliferation in vitro and in vivo and has also been found to be expressed in CAF of HNSCC [14, 15]. During this process of EMT, invasive tumor cells lose their epithelial cell polarity, morphology, and acquire mesenchymal as well as stemness-related features [16].
Besides the system of Wnt/beta-catenin and MMPs, other factors such as ETS1, a transcriptional factor which regulates critical functions in normal cell homeostasis, can contribute to tumor progression through effects on downstream target genes in EMT [17, 18]. Moreover, proteolytic enzymes like cathepsins can affect cancer progression by irreversibly cleaving peptide bonds and facilitating tissue penetration [19, 20]. Cathepsin b is frequently overexpressed in both cancer cells and the tumor stroma [21], favoring cell invasion into adjacent tissue and leading to poor prognosis in case of overexpression [22, 23]. An inhibition of cathepsin b can successfully stall liver tumor cell invasion and metastasis through the reduction of the proteinases activity and EMT [24]. However, little is known about the influence of cathepsin b and ETS1 in HNSCC.
The current knowledge suggests that MSCs can affect cancer progression through interaction with HNSCC tumor cells on a number of pathways. It was thus the aim of this study to test the hypothesis that interactions of human MSCs with the HNSCC cell line PCI-13 affect the expression of markers of EMT and tumor progression such as Wnt3, beta-catenin, MMP14, E-cadherin, cathepsin b, and ETS1.
Material and methods
Isolation of human MSC
The isolation of human MSCs from iliac bone marrow of seven patients, aged between 8 and 58 years, was carried out in accordance with the patients’ informed consent and according to the guidelines and approval of the local ethics committee (no. 15/10/01). None of the patients was known to have infections, cancers, chronic diseases or any generalized bone marrow or connective tissue diseases. The isolation of MSC was performed using density gradient centrifugation for 20 min at 800g. The light band forming between lymphocyte and erythrocyte band was separated, and the cells acquired, washed, and centrifuged for 5 min at 300g. The number of cells was determined, and the cell suspension was plated onto 75-cm2 tissue culture flasks. Non-adherent cells were removed by the first medium change after 24 h. Single colonies of adherent fibroblast-like cells were first visible after 72 h of cultivation. All cultivations were performed at 37 °C and 5 % CO2.
Cultivation of human MSC
MSC were cultured in basal medium consisting of high glucose Dulbecco’s modified Eagle’s medium (DMEM) supplemented with 1 % non-essential amino acids, 1 % β-mercaptoethanol, 2 % gentamicin, and 10 % fetal bovine serum. When adherent cells reached approximately 80–90 % confluence, they were washed with phosphate-buffered saline (PBS), trypsinized, and centrifuged for 5 min at 250g. The cells were plated at a density of 1 × 104 cells/cm2. Mesenchymal and hematopoetic cluster antigens were evaluated by means of flow cytometry. The MSC isolates were then pooled and transferred into co-culture (passage 2).
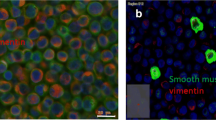
Flow cytometric analysis of human MSC
Trypsin/EDTA- treated cells (0.25 %) (passage 2) were washed twice with fluorescence-activated cell sorting (FACS) buffer (PBS, 1 % BSA, and 0.1 % NaN3), adjusted to approximately 5 × 105 cells/ml and subsequently stained. A 100-μl cell suspension was incubated with 10 μl phycoerythrin (PE)-conjugated monoclonal antibodies (mAbs) at 4 °C for 30 min. To discriminate human MSCs from cells of hematopoietic origin, isolates were stained for CD133 and CD45. In addition, the following antigens were included into the phenotyping profile: CD105, CD90, CD73, and STRO-1. All samples were filled up to a total volume of 500 μl with FACS buffer prior to analysis. Cells were analyzed on a Cytomics FC 500 flow cytometer using cytomics CXP software (Beckman Coulter, Krefeld, Germany). At least 10000 events were acquired and analyzed using a one-parametric protocol (FL1) and FSC/SSC dot plot diagram to exclude cell debris by gating. Non-specific isotype-matched controls were used to determine background fluorescence. All mAbs were purchased from Becton Dickinson (Heidelberg, Germany).
Cultivation of human HNSCC cell line PCI-13
Cryopreserved tumor cells of the established HNSCC cell line PCI-13 (UICC: T3, N1, M0) [25, 26] were thawed, resuspended, and cultured in tumor medium consisting of low glucose DMEM supplemented with 10 % fetal bovine serum and 2 % gentamicin. Adherence of the cells was observed within 24 h. After reaching 80–90 % confluence, cells were transferred into co-culture.
Indirect co-culture and proliferation analysis of MSC and PCI-13
PCI-13 and MSC co-culture was conducted using Thincert® permeable membrane cell culture inserts in six-well plates (Greiner Bio-One). MSC were seeded onto the insert membrane. PCI-13 culture was performed on the well floor. All cells were cultured in tumor medium. MSC and PCI-13 monolayer controls were performed in the insert or well floor, respectively. All analyses were carried out in three independent experiments per experimental group (n = 3) on sampling days 4 and 7. Proliferation of PCI-13 and MSC was determined by automatic cell count (CASY model TT, triplicate measurement) using electric impedance measurement.
RT-qPCR analysis of MSC and PCI-13
MSC and PCI-13 cultured via indirect co-culture were collected at different time points (4 and 7 days), washed twice with PBS, and total RNA was isolated using a standardized RNA Isolation Kit (RNeasy® Mini Kit, Qiagen) according to the manufacturer’s recommendations. Samples were treated with DNAse-I to remove genomic DNA contamination and purified using phenol-chloroform extraction. Samples were precipitated, washed in 75 % ethanol, resuspended in 50 μl RNase-free water, and stored at −80 °C. RNA quality was determined by the use of microfluidic electrophoresis (Agilent 2100 Bioanalyzer, Agilent Technologies). The RNA concentrations were determined by measuring the absorbance at 260 and 280 nm. In addition, sample quality was assured using electrophoresis (Agilent 2100 Bioanalyzer) according to the manufacturer’s recommendations. Samples of 200 ng RNA were reverse-transcribed using iScript cDNA Synthesis Kit (Bio-Rad). Aliquots of 5 μl from the reverse transcriptase reactions were used for amplification of transcripts using primers specific for Wnt3, E-cadherin, beta-catenin, MMP14, cathepsin b, ETS1, and GAPDH (Table 1). All samples were stored at −80 °C for further analysis. For relative cDNA quantification, the Bio-Rad MyIQ® real-time PCR Detection System with the Bio-Rad iQ® SYBR Green Supermix was used. PCR quantification was carried out after denaturation for 30 s at 98 °C, followed by amplification and measurement for 45 cycles of 1-s denaturation at 94 °C, 15-s annealing at 60 °C, and 10-s elongation at 72 °C. Electrophoretic separation of PCR products was carried out on 1.5 % (w/v) agarose gels and 0.7 ng/ml ethidium bromide. No additional signals were observed for all PCR products.
Statistical analysis
The detected cell count triplicates of each observation day were averaged for both PCI-13 cells and MSC. For the RT-qPCR, relative expression ratios were determined via the mathematical model for relative quantification by Pfaffl [27]. After log2-transformation, differences in cell proliferation and gene expression were identified by a two-way ANOVA model using the open source software “R.” The level of significance was set to 5 %.
Results
Immunophenotypic characterization of MSC from bone marrow
The isolated MSCs showed a distinct phenotypic population (>90 % homogeneous in passage 2). To further characterize the isolated cells, CD surface antigen marker expression was analyzed by means of flow cytometric measurement (Fig. 1). The MSC isolates were negative for CD45 (leukocyte common antigen) and CD133 (prominin-1), indicating that they were not of hematopoietic origin. Analysis for CD90 (thymocyte differentiation antigen-1, Thy-1) and the matrix receptor CD105 (endoglin, SH2) revealed strong expression. The cells expressed reduced levels of CD73 (5′-nucleotidase) and STRO-1.
Proliferation and expression of ETS1 and cathepsin b
PCI-13 and MSCs showed a continuous proliferation with an increasing cell number during the observation time. No significant effect on proliferation was observed, when the two cell types were co-cultured (Fig. 2a, b). The expression of cathepsin b was significantly increased over time in PCI-13 cells in both co-cultures and controls (p < 0.05, Fig. 3a). The expression was lower in co-cultured PCI-13 cells when compared to the controls, however not significant. The expression of cathepsin b in MSCs did not change over time in neither of the groups. The expression of ETS1 exhibited a slight but non-significant decrease in PCI-13 cells in both types of culture. ETS1 expression did not change in both groups of MSC cultures (Fig. 3b).
Expression of EMT markers
Among the markers of EMT, E-cadherin displayed a significantly reduced level in PCI-13 cells co-cultutred with MSC after 7 days of cultivation in comparison to the control group (p < 0.05, Fig. 4a). This reduction of E-cadherin was accompanied by a significant reduction of Wnt3 expression in PCI-13/MSC co-culture (p < 0.05, Fig. 4b). In accordance with the decrease in Wnt3, beta-catenin expression was found to be reduced in PCI-13 under co-culture influence with MSC in comparison to the control (Fig. 5a). In addition, the reduced influence of beta-catenin on transcription was associated with a significantly decreased expression of MMP14 in PCI-13 cells under co-culture conditions with MSCs (p < 0.05, Fig. 5b). In contrast to PCI-13 cells, MSCs did not display significant changes in any of the markers of EMT (E-cadherin, Wnt3, beta-catenin, nor MMP14) in co-culture or control groups indicating that MSCs retained their profile without being influenced by co-cultured PCI-13.
Discussion
CAFs, MSCs, and tumor cells are often found at the invasive edge of cancer, affecting tumor transition, transformation, and progression [2, 28]. MSCs are considered to provide a progenitor reservoir for CAFs and thereby influence cancer progression [3, 4]. The present study thus evaluates possible interactions between MSCs and the HNSCC cell line PCI-13, which may contribute to invasiveness and progression of head and neck cancer. An indirect co-culture model of transwell cultures has been chosen to limit the analysis to paracrine communication between MSCs and PCI-13 cells. MSC and PCI-13 showed a continuous cellular increase during the observation time with no significant effect with respect to enhancement or suppression in indirect co-culture and control groups. Previous studies have reported contradictory results with the presence of MSCs favoring tumor growth of adenocarcinomas and tumors of mesenchymal origin [29], whereas others have found inhibitory effects of MSCs on the proliferation of breast cancer cells [30], hepatocellular cancer cells [4], myeloic leukemia cells [31], or HNSCC of the tonsils [32]. It thus appears that malignant tumors of different origins react differently in co-culture with MSCs in in vitro settings.
One of the interactions that may enhance tumor invasion, progression, and metastasis of HNSCC is EMT. During EMT, the loss of E-cadherin is associated with the loss of epithelial polarity features [16, 1]. In our study, the expression of E-cadherin was significantly reduced during the observation period in PCI-13 cells co-cultured with MSCs. This may indicate an enhancing effect of MSCs on the onset of EMT in HNSCCs. In addition, E-cadherin expression has been found to correlate with the degree of dedifferentiation where the least differentiated tumors showed reduced expression of E-cadherin [33]. However, while the loss of E-cadherin at the invasion stage seems to be critical for the detachment of tumor cells, its expression is heterogenic and can increase in different parts of the same tumor [34]. Moreover, a physiological downregulation of E-cadherin takes place during wound healing, allowing epithelial cells to move and cover injured tissue [35]. This process can be facilitated and enhanced in the presence of MSC [36]. Thus, in consideration of these diverse patterns of E-cadherin expression, the loss of E-cadherin in tumor cells may not be exclusively related to the onset EMT [37].
Tumor progression at the invasive front is influenced by beta-catenin allowing for an EMT dedifferentiation and a subsequent redifferentiation with regain of epithelial capabilities [38]. Beta-catenin is influenced by the interaction with E-cadherin and has been found to be reduced in our study as another marker of EMT. In the oral epithelium, beta-catenin links E-cadherin to the cytoskeleton. A reduction in E-cadherin would therefore be associated with a decrease in beta-catenin. The clinic-pathological significance of beta-catenin expression in whole tumor sections from HNSCC patients is controversial. While in some studies beta-catenin expression independently predicted short overall survival [39, 40], others reported no significant association with local recurrence, survival, or any other clinic-pathological feature [35, 41]. This might be due to the fact that tumor cells in HNSCC of different patients exhibit a heterogeneous cell population with different levels of expressions of E-cadherin and beta-catenin [38, 42–44].
The Wnt/beta-catenin pathway is frequently altered in different forms of cancer and EMT [45, 7]. In our study, Wnt3 expression has been found to be significantly reduced in HNSCC cells co-cultured with MSCs. The reduction of Wnt would lead to a stabilization of the APC/GSK3 complex, which in turn leads to increased phosphorylation and cleavage of beta-catenin and hence would explain the observed reduction of beta-catenin. Finally, MMP14, a member of the MMP family involved in EMT, has been found to be significantly reduced in HNSCC cells co-cultured with MSCs. This is in line with the observed decrease in beta-catenin, as a reduced nuclear transition of beta-catenin leads to a decrease in MMP14 expression [46].
Taken together, it appears that three of the four markers of EMT addressed in this study are downregulated concordantly in PCI-13 during co-culture with MSCs in a sense that EMT is suppressed. The isolated loss of E-cadherin appears to contradict this but is not necessarily indicative for the onset of EMT as extensive analysis of gene regulatory networks in EMT could not identify a master regulator. It has been suggested that EMT requires multiple simultaneous regulatory mechanism leading to a successful transition [18]. The results from the present study thus indicate that the paracrine effect of MSCs do not support but rather suppress the onset of EMT in PCI-13. This is supported by the fact that ETS1, whose downstream targets genes regulate critical functions in EMT [18], and other progression factors such as cathepsin b, have not shown significant changes in the present study when co-cultured with MSCs.
References
Smith A, Teknos TN, Pan Q (2013) Epithelial to mesenchymal transition in head and neck squamous cell carcinoma. Oral Oncol 49(4):287–292. doi:10.1016/j.oraloncology.2012.10.009
Routray S, Sunkavali A, Bari K (2013) Carcinoma-associated fibroblasts, its implication in head and neck squamous cell carcinoma: a mini review. Oral Dis. doi:10.1111/odi.12107
Fierro FA, Sierralta WD, Epunan MJ, Minguell JJ (2004) Marrow-derived mesenchymal stem cells: role in epithelial tumor cell determination. Clin Exp Metastsis 21(4):313–319
Qiao L, Xu Z, Zhao T, Zhao Z, Shi M, Zhao RC, Ye L, Zhang X (2008) Suppression of tumorigenesis by human mesenchymal stem cells in a hepatoma model. Cell Res 18(4):500–507. doi:10.1038/cr.2008.40
Gottschling S, Granzow M, Kuner R, Jauch A, Herpel E, Xu EC, Muley T, Schnabel PA, Herth FJ, Meister M (2013) Mesenchymal stem cells in non-small cell lung cancer—different from others? Insights from comparative molecular and functional analyses. Lung Cancer 80(1):19–29. doi:10.1016/j.lungcan.2012.12.015
Nishimura K, Semba S, Aoyagi K, Sasaki H, Yokozaki H (2012) Mesenchymal stem cells provide an advantageous tumor microenvironment for the restoration of cancer stem cells. Pathobiology 79(6):290–306. doi:10.1159/000337296
Gos M, Miloszewska J, Przybyszewska M (2009) Epithelial-mesenchymal transition in cancer progression. Postepy Biochem 55(2):121–128
Higashikawa K, Yoneda S, Taki M, Shigeishi H, Ono S, Tobiume K, Kamata N (2008) Gene expression profiling to identify genes associated with high-invasiveness in human squamous cell carcinoma with epithelial-to-mesenchymal transition. Cancer Lett 264(2):256–264. doi:10.1016/j.canlet.2008.01.045
Aprelikova O, Palla J, Hibler B, Yu X, Greer YE, Yi M, Stephens R, Maxwell GL, Jazaeri A, Risinger JI, Rubin JS, Niederhuber J (2012) Silencing of miR-148a in cancer-associated fibroblasts results in WNT10B-mediated stimulation of tumor cell motility. Oncogene 32(27):3246–3253. doi:10.1038/onc.2012.351
Hakim SG, Kosmehl H, Sieg P, Trenkle T, Jacobsen HC, Attila Benedek G, Ribbat J, Driemel O (2011) Altered expression of cell-cell adhesion molecules beta-catenin/E-cadherin and related Wnt-signaling pathway in sporadic and syndromal keratocystic odontogenic tumors. Clin Oral Investig 15(3):321–328. doi:10.1007/s00784-010-0388-8
Yi N, Liao QP, Li ZH, Xie BJ, Hu YH, Yi W, Liu M (2013) RNA interference-mediated targeting of DKK1 gene expression in Ishikawa endometrial carcinoma cells causes increased tumor cell invasion and migration. Oncol Lett 6(3):756–762. doi:10.3892/ol.2013.1439
Ulasov I, Thaci B, Sarvaiya P, Yi R, Guo D, Auffinger B, Pytel P, Zhang L, Kim CK, Borovjagin A, Dey M, Han Y, Baryshnikov AY, Lesniak MS (2013) Inhibition of MMP14 potentiates the therapeutic effect of temozolomide and radiation in gliomas. Cancer Med 2(4):457–467. doi:10.1002/cam4.104
Devy L, Huang L, Naa L, Yanamandra N, Pieters H, Frans N, Chang E, Tao Q, Vanhove M, Lejeune A, van Gool R, Sexton DJ, Kuang G, Rank D, Hogan S, Pazmany C, Ma YL, Schoonbroodt S, Nixon AE, Ladner RC, Hoet R, Henderikx P, Tenhoor C, Rabbani SA, Valentino ML, Wood CR, Dransfield DT (2009) Selective inhibition of matrix metalloproteinase-14 blocks tumor growth, invasion, and angiogenesis. Cancer Res 69(4):1517–1526. doi:10.1158/0008-5472.CAN-08-3255
Zhang W, Matrisian LM, Holmbeck K, Vick CC, Rosenthal EL (2006) Fibroblast-derived MT1-MMP promotes tumor progression in vitro and in vivo. BMC Cancer 6:52. doi:10.1186/1471-2407-6-52
Rosenthal EL, McCrory A, Talbert M, Carroll W, Magnuson JS, Peters GE (2004) Expression of proteolytic enzymes in head and neck cancer-associated fibroblasts. Arch Otolaryngol Head Neck Surg 130(8):943–947. doi:10.1001/archotol.130.8.943
Casarsa C, Bassani N, Ambrogi F, Zabucchi G, Boracchi P, Biganzoli E, Coradini D (2011) Epithelial-to-mesenchymal transition, cell polarity and stemness-associated features in malignant pleural mesothelioma. Cancer Lett 302(2):136–143. doi:10.1016/j.canlet.2011.01.009
Findlay VJ, LaRue AC, Turner DP, Watson PM, Watson DK (2013) Understanding the role of ETS-mediated gene regulation in complex biological processes. Adv Cancer Res 119:1–61. doi:10.1016/B978-0-12-407190-2.00001-0
Saunders LR, McClay DR (2014) Sub-circuits of a gene regulatory network control a developmental epithelial-mesenchymal transition. Development 141(7):1503–1513. doi:10.1242/dev.101436
Reiser J, Adair B, Reinheckel T (2010) Specialized roles for cysteine cathepsins in health and disease. J Clin Invest 120(10):3421–3431. doi:10.1172/JCI42918
Oliver JR, Kushwah R, Hu J (2012) Multiple roles of the epithelium-specific ETS transcription factor, ESE-1, in development and disease. Lab Invest 92(3):320–330. doi:10.1038/labinvest.2011.186
Bengsch F, Buck A, Gunther SC, Seiz JR, Tacke M, Pfeifer D, von Elverfeldt D, Sevenich L, Hillebrand LE, Kern U, Sameni M, Peters C, Sloane BF, Reinheckel T (2013) Cell type-dependent pathogenic functions of overexpressed human cathepsin B in murine breast cancer progression. Oncogene. doi:10.1038/onc.2013.395
Mohamed MM, Sloane BF (2006) Cysteine cathepsins: multifunctional enzymes in cancer. Nat Rev Cancer 6(10):764–775. doi:10.1038/nrc1949
Gocheva V, Zeng W, Ke D, Klimstra D, Reinheckel T, Peters C, Hanahan D, Joyce JA (2006) Distinct roles for cysteine cathepsin genes in multistage tumorigenesis. Genes Dev 20(5):543–556. doi:10.1101/gad.1407406
Tang N, Xie Q, Wang X, Li X, Chen Y, Lin X, Lin J (2011) Inhibition of invasion and metastasis of MHCC97H cells by expression of snake venom cystatin through reduction of proteinases activity and epithelial-mesenchymal transition. Arch Pharm Res 34(5):781–789. doi:10.1007/s12272-011-0512-6
Snyderman CH, Klapan I, Milanovich M, Heo DS, Wagner R, Schwartz D, Johnson JT, Whiteside TL (1994) Comparison of in vivo and in vitro prostaglandin E2 production by squamous cell carcinoma of the head and neck. Otolaryngol Head Neck Surg 111(3 Pt 1):189–196
Heo DS, Snyderman C, Gollin SM, Pan S, Walker E, Deka R, Barnes EL, Johnson JT, Herberman RB, Whiteside TL (1989) Biology, cytogenetics, and sensitivity to immunological effector cells of new head and neck squamous cell carcinoma lines. Cancer Res 49(18):5167–5175
Pfaffl MW (2001) A new mathematical model for relative quantification in real-time RT-PCR. Nucleic Acids Res 29(9):e45
Mravic M, Asatrian G, Soo C, Lugassy C, Barnhill RL, Dry SM, Peault B, James AW (2014) From pericytes to perivascular tumours: correlation between pathology, stem cell biology, and tissue engineering. Int Orthop 38(9):1819–1824. doi:10.1007/s00264-014-2295-0
Zhu W, Xu W, Jiang R, Qian H, Chen M, Hu J, Cao W, Han C, Chen Y (2006) Mesenchymal stem cells derived from bone marrow favor tumor cell growth in vivo. Exp Mol Path 80(3):267–274. doi:10.1016/j.yexmp.2005.07.004
Lu YR, Yuan Y, Wang XJ, Wei LL, Chen YN, Cong C, Li SF, Long D, Tan WD, Mao YQ, Zhang J, Li YP, Cheng JQ (2008) The growth inhibitory effect of mesenchymal stem cells on tumor cells in vitro and in vivo. Cancer Biol Ther 7(2):245–251
Zhu Y, Sun Z, Han Q, Liao L, Wang J, Bian C, Li J, Yan X, Liu Y, Shao C, Zhao RC (2009) Human mesenchymal stem cells inhibit cancer cell proliferation by secreting DKK-1. Leukemia 23(5):925–933. doi:10.1038/leu.2008.384
Lim YS, Lee JC, Lee YS, Lee BJ, Wang SG (2012) Growth inhibitory effect of palatine tonsil-derived mesenchymal stem cells on head and neck squamous cell carcinoma cells. Clin Exp Otorhinolaryngol 5(2):86–93. doi:10.3342/ceo.2012.5.2.86
Bagutti C, Speight PM, Watt FM (1998) Comparison of integrin, cadherin, and catenin expression in squamous cell carcinomas of the oral cavity. J Pathol 186(1):8–16. doi:10.1002/(SICI)1096-9896(199809)186:1<8::AID-PATH156>3.0.CO;2-H
Hung KF, Chang CS, Liu CJ, Lui MT, Cheng CY, Kao SY (2006) Differential expression of E-cadherin in metastatic lesions comparing to primary oral squamous cell carcinoma. J Oral Pathol Med 35(10):589–594. doi:10.1111/j.1600-0714.2006.00474.x
Kurtz KA, Hoffman HT, Zimmerman MB, Robinson RA (2006) Decreased E-cadherin but not beta-catenin expression is associated with vascular invasion and decreased survival in head and neck squamous carcinomas. Otolaryngol Head Neck Surg 134(1):142–146. doi:10.1016/j.otohns.2005.08.026
You DH, Nam MJ (2013) Effects of human epidermal growth factor gene-transfected mesenchymal stem cells on fibroblast migration and proliferation. Cell Prolif 46(4):408–415. doi:10.1111/cpr.12042
Hollestelle A, Peeters JK, Smid M, Timmermans M, Verhoog LC, Westenend PJ, Heine AA, Chan A, Sieuwerts AM, Wiemer EA, Klijn JG, van der Spek PJ, Foekens JA, Schutte M, den Bakker MA, Martens JW (2013) Loss of E-cadherin is not a necessity for epithelial to mesenchymal transition in human breast cancer. Breast Cancer Res Treat 138(1):47–57. doi:10.1007/s10549-013-2415-3
Brabletz T, Jung A, Reu S, Porzner M, Hlubek F, Kunz-Schughart LA, Knuechel R, Kirchner T (2001) Variable beta-catenin expression in colorectal cancers indicates tumor progression driven by the tumor environment. Proc Natl Acad Sci U S A 98(18):10356–10361. doi:10.1073/pnas.171610498
Pukkila MJ, Virtaniemi JA, Kumpulainen EJ, Pirinen RT, Johansson RT, Valtonen HJ, Juhola MT, Kosma VM (2001) Nuclear beta catenin expression is related to unfavourable outcome in oropharyngeal and hypopharyngeal squamous cell carcinoma. J Clin Pathol 54(1):42–47
Ravindran G, Devaraj H (2012) Aberrant expression of beta-catenin and its association with DeltaNp63, Notch-1, and clinicopathological factors in oral squamous cell carcinoma. Clin Oral Investig 16(4):1275–1288. doi:10.1007/s00784-011-0605-0
Rosado P, Lequerica-Fernandez P, Fernandez S, Allonca E, Villallain L, de Vicente JC (2013) E-cadherin and beta-catenin expression in well-differentiated and moderately-differentiated oral squamous cell carcinoma: relations with clinical variables. Br J Oral Maxillofac Surg 51(2):149–156. doi:10.1016/j.bjoms.2012.03.018
Liu LK, Jiang XY, Zhou XX, Wang DM, Song XL, Jiang HB (2010) Upregulation of vimentin and aberrant expression of E-cadherin/beta-catenin complex in oral squamous cell carcinomas: correlation with the clinicopathological features and patient outcome. Mod Pathol 23(2):213–224. doi:10.1038/modpathol.2009.160
Wang X, Zhang J, Fan M, Zhou Q, Deng H, Aisharif MJ, Chen X (2009) The expression of E-cadherin at the invasive tumor front of oral squamous cell carcinoma: immunohistochemical and RT-PCR analysis with clinicopathological correlation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 107(4):547–554. doi:10.1016/j.tripleo.2008.11.021
Mahomed F, Altini M, Meer S (2007) Altered E-cadherin/beta-catenin expression in oral squamous carcinoma with and without nodal metastasis. Oral Dis 13(4):386–392. doi:10.1111/j.1601-0825.2006.01295.x
Polakis P (2000) Wnt signaling and cancer. Genes Dev 14(15):1837–1851
Neth P, Ciccarella M, Egea V, Hoelters J, Jochum M, Ries C (2006) Wnt signaling regulates the invasion capacity of human mesenchymal stem cells. Stem Cells 24(8):1892–1903. doi:10.1634/stemcells. 2005-0503
Acknowledgments
The work was supported by the Clinic of Oral and Maxillofacial Surgery and the medical faculty of the Georg-August-University Göttingen, Germany. We are grateful to Jutta Schulz for her technical assistance.
Ethical standards
The isolation of human MSC was carried out in accordance with the patients’ informed consent and according to the guidelines and approval of the local ethics committee (no. 15/10/01) of the Georg-August-University Göttingen. It has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Conflict of interest
The authors have no further interest in companies or other entities that have an interest in the information in the contribution. There is no conflict of interest pending.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Böhrnsen, F., Fricke, M., Sander, C. et al. Interactions of human MSC with head and neck squamous cell carcinoma cell line PCI-13 reduce markers of epithelia-mesenchymal transition. Clin Oral Invest 19, 1121–1128 (2015). https://doi.org/10.1007/s00784-014-1338-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-014-1338-7