Abstract
Objectives
The aim of the study was to compare the effectiveness of vasodilator isoxsuprine to dexamethasone with hyaluronidase injections and physiotherapy in the treatment of oral submucous fibrosis.
Materials and methods
Forty patients with oral submucous fibrosis were randomly assigned into three groups. Group A patients (n = 15) received 10 mg isoxsuprine tablets four times per day, group B (n = 15) biweekly dexamethasone with hyaluronidase intralesional injections, and group C (n = 10) placebo tablets. In addition, all patients were instructed physiotherapy exercises. The treatment time was 6 weeks and patients were followed-up for 4 months thereafter. The effect of the treatment was evaluated by measurements of inter-incisal distance and oral burning sensation and evaluation of histological findings of the diseased mucosa.
Results
Mouth opening increased and burning sensation decreased significantly in all groups, but the effects were significantly greater in groups receiving either oral isoxsuprine or dexamethasone with hyaluronidase injections in addition to physiotherapy. The decrease in burning sensation occurred more rapidly in patients receiving intralesional dexamethasone with hyaluronidase. Histological improvement was not observed in any of the groups.
Conclusions
Oral isoxsuprine as well as dexamethasone with hyaluronidase injections combined to physiotherapy alleviate symptoms of oral submucous fibrosis significantly more efficiently than physiotherapy alone.
Clinical relevance
Oral isoxsuprine can be considered as a new candidate drug for the treatment of oral submucous fibrosis. Physiotherapy exercises provide relief of symptoms and should be instructed to all patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Oral submucous fibrosis is a severely disabling and progressive disease with estimated malignant transformation rate of 7–13 % [1]. Areca nut, a highly addictive agent, has been identified as the major etiological factor of oral submucous fibrosis [2]. In addition, there are indications of genetic predisposition possibly related to immunological mechanisms. Nutritional deficiencies may further contribute to the course of the disease. The condition is predominantly affecting people from South and South-East Asia and people migrated from these areas among whom areca nut use is known to be common [1, 3].
Local irritation by areca nut results in epithelial injury and chronic inflammation which induces fibrosis and hyalinization [1, 3]. These changes initially affect the lamina propria and gradually further the submucosa and the musculature resulting in loss of tissue elasticity. The condition is hypothesized to result from collagen metabolism disorder either caused by reduced collagen breakdown or increased collagen synthesis [3]. Indeed, areca nut alkaloids have been shown to increase collagen synthesis by fibroblasts [4] and tannins to inhibit collagenase activity in vitro [5]. Fibrosis and malignant transformation has been suggested to be driven by betel-derived alkaloid induced upregulation of keratinocyte v 6 expression [6].
The initial symptoms include oral burning sensation, intolerance to spicy food, and mucosal ulcerations [7]. Disease progresses unless areca nut use is stopped at this stage. Signs of advanced disease are stiffening and blanching of oral mucosa along with development of fibrous bands on cheek, lips, and soft palate. Also pharynx and the upper part of the esophagus can be affected. This leads to reduced mouth opening and difficulties in taking care of oral hygiene, eating, swallowing, and speaking. Reduced mouth opening also complicates inspection of oral cavity for possible malignant lesions.
The severity of the disease has been proposed to be classified by the degree of trismus and other clinical findings [8, 9], histological findings [10], or all these together [11]. Staging of the condition can be helpful when choosing the line of therapy that should be used. Current treatment options include medical treatment with dietary supplements and immunomodulatory, proteolytic, and vasoactive agents [8, 12]. Surgical interventions may be necessary in advanced stages of disease. Medical and surgical treatment can be combined with physiotherapy or physiotherapy can be used alone.
Immunomodulatory therapy by corticosteroid injections is the primary medical treatment option in many centers. Corticosteroids of different types have been used in several studies [11, 13–19] yet little controlled evidence exists of its efficacy. Also proteolytic enzymes alone or combined to corticosteroids [13–16, 18, 19], vasodilative agents [16, 20–22], nutrients, and anti-oxidants [15–17] have been used and reported to provide varying degree of relief to the patients.
In the present study, the efficacy of a vasodilative agent, isoxsuprine, combined with physiotherapy, was compared to intralesional injections of dexamethasone with hyaluronidase and physiotherapy or physiotherapy alone on the symptoms of oral submucous fibrosis. Our results show that all of these treatments increase mouth opening and reduce burning sensation significantly, but both isoxsuprine and dexamethasone with hyaluronidase alleviated these symptoms significantly more efficiently compared to physiotherapy alone. Burning sensation decreased sooner in patients having dexamethasone with hyaluronidase injections compared to isoxsuprine treatment group. In the follow-up samples, significant histological improvement was not observed in any of the groups.
Materials and methods
Patients
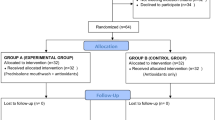
The study protocol was approved by the ethics committee of Mumbai government dental college and hospital and written informed consent was obtained from the patients. Patients with oral submucous fibrosis were recruited from the outpatient clinic of Mumbai government dental college and hospital. Initially, a total number of 54 patients entered the study. Only patients who complied with the study protocol and fulfilled the diagnostic criteria of oral submucous fibrosis were included in the final study population of 40 patients.
The diagnostic criteria were history of oral burning sensation when eating, subjectively observed gradual reduction in mouth opening and a feeling of loss of elasticity in buccal tissues and bilateral buccal fibrous bands observed objectively on palpation by the investigator. Five patients did not experience burning sensation, but otherwise all patients fulfilled all four diagnostic criteria. All patients had a history of gutka or areca nut use, and the majority of patients had in addition smoked or chewed tobacco. Patients with oral malignancy, other mucosal diseases (including chronic ulcers, leukoplakia, lichen planus, and infectious mucositis), trismus due to other conditions, earlier treatment for oral submucous fibrosis, systemic diseases, regular medication, patients debilitated by high age, and pregnant women were excluded from the study.
Study protocol
Patients entering the study were explained in detail about the condition affecting their oral cavity and about the study protocol. A thorough medical history of each patient was obtained and a detailed clinical examination of the oral cavity was carried out by a single investigator. Inter-incisal distance was measured mouth fully open using the mesial incisal edges of right maxillary and mandibular central incisors as reference points. In patients missing maxillary and/or mandibular central incisor, the distance between the highest points in maxillary and mandibular alveolar crest midline was recorded. The measurement was done with a vernier caliper and geometric divider. Intensity of burning sensation at the time of the visits was evaluated by using a modified visual analog scale (VAS). A scale consisting of a 10 cm line on which 0 cm corresponded to “no burning sensation” and 10 cm “burning sensation as bad as it could be” was designed. The patients were asked to quantify current burning sensation on VAS and the corresponding number was recorded. Patients’ teeth were cleaned of stains and a pretreatment punch biopsy was taken from the diseased buccal mucosa to histologically grade the severity of the condition.
The patients were then randomly divided into three groups (A–C). All patients were instructed to carry out mouth opening and cheek blowing exercises and advised to discontinue the habit (chewing of betel nut, tobacco, gutka, mawa, etc.). Mouth opening exercise was carried out by positioning a maximal number of tongue spatulas between the teeth. A spatula was added every 5–10 days to gradually increase the opening. Exercises were instructed to be done three times per day during treatment and follow-up periods.
In addition, group A patients (n = 20) were administered isoxsuprine 10 mg tablets orally (Tablet Duvadilan, Solvay pharma) four times a day. Group B patients (n = 17) were given twice a week bilateral intralesional injections of 2 ml dexamethasone (Injection Dexona, Cadila Healthcare Ltd) with 1,500 IU hyaluronidase (Injection Hyalase, CP Pharmaceuticals LTD) mixed with 1 ml of 2 % lignocaine solution with adrenaline 1:80,000 (Lignox 2 % A, Indoco Remedies Ltd) at the site of palpable fibrous bands on the buccal mucosa. Group C patients (n = 17) received orally placebo capsules containing fine sugar.
Oral status and VAS scores were recorded twice a week during the 6-week treatment period by a single investigator. The discontinuation of the habit was controlled by inspection for possible intraoral stains and interviewing the patient and accompanying persons or relatives. Following physiotherapy instructions was controlled by interviewing the patients. The patients were asked to report immediately if there were symptoms suggestive of relapse or side effects.
One week after completion of therapy, each patient was subjected to post-treatment biopsy. The patients were further clinically examined every 15 days for 4 months.
Analysis of biopsy samples
Biopsy specimens were examined blinded by a single pathologist. The specimens were grouped according to the presence of signs typical for oral submucous fibrosis and graded by severity of findings as described earlier [10]. By stage, the groups were assigned a histological score ranging from 0 to 4 for the purpose of comparison and statistical analysis. Criteria for staging and corresponding scoring are presented in Table 1.
Pre- and post-treatment biopsy samples were also specifically evaluated for the presence of certain particular histological findings used for staging of oral submucous fibrosis. These included epithelial atrophy and hyperplasia, hyperkeratosis or parakeratosis, epithelial atypia, the amount of subepithelial collagen and inflammatory reaction, hyalinization, or sclerosis and the degree of vascularity.
Statistical analyses
All findings were tabulated and data were subjected to statistical analysis by Student’s t test by Prism 4.0 software (Primer for Windows, Microsoft). P values of less than 0.05 were considered statistically significant.
Results
Characteristics of the final study population
Of the initially recruited 54 patients, 40 were included in the final study population and randomly assigned to groups A (n = 15), B (n = 15), and C (n = 10). All together 14 patients were not able to adhere to the study protocol and were therefore excluded. The number of excluded patients was five in group A, two in group B, and seven in group C. The majority of drop-outs occurred during the first 3 weeks of the treatment period. The drop-outs did not give any specific reason for low adherence to study protocol, nor reported of any side-effects from the treatment.
The demographics of the subgroups are presented in Table 2. In the final study population, 82.5 % of patients were males and 17.5 % were females. In each group, there was a male predominance. There was no significant difference in age between the groups (group A vs B, p = 0.352; A vs C, p = 0.419; B vs C, p = 0.841). None of the patients in the final study group reported of any harmful side-effects during the study. The symptoms related to oral submucous fibrosis did not worsen compared to the situation at the beginning of the study in any participant.
Effect of treatments on mouth opening
Figure 1 shows the changes in mouth opening measured as inter-incisal distance in the beginning of the study, at end of the treatment and at the end of the 4 months follow-up period. At starting point, the inter-incisal distance differed significantly only between groups B and C (p = 0.004) with group B patients having more restricted mouth opening. The differences between groups A and B (p = 0.144) or A and C (p = 0.496) were not significant. The majority of patients had a mouth opening in the range of 20–40 mm. In group A, two patient had an opening of less than 20 mm and two patients bigger than 40 mm, the respective values for group B are 4 and 0 and for group C, 2 and 0.
The inter-incisal distance widened significantly in all groups (Fig. 1) suggesting that physiotherapy improves mouth opening. At the end of the follow-up period, the improvement was, however, significantly greater in treatment groups A and B compared to group C conducting physiotherapy alone (A vs C, p < 0.00001; B vs C, p < 0.00001). Mouth opening improved in average the most (4.0 mm) in group B patients having injections of dexamethasone with hyaluronidase whereas in group A having isoxsuprine the average improvement was 3.0 mm. This difference was not, however, significant (p = 0.164) suggesting that both of these treatments combined to physiotherapy are more efficient than physiotherapy alone. The outcome was achieved already at the end of the treatment period and maintained throughout the follow-up period in group A (p = 0.092) and group B (p = 0.111). In group C, some further improvement occurred during follow-up period compared to the end of the treatment period (p = 0.015).
Effect of treatments on burning sensation
In the beginning of the study, there was no difference between the groups in burning sensation evaluated by modified VAS (A vs B, p = 0.809; A vs C, p = 0.751; B vs C, p = 1). In group A (3/15) and in group B (2/15), subjects had no burning sensation in the beginning of the study. Instead in group C, all subjects had some degree of burning sensation (Fig. 2).
In group A, 10/12 patients and all patients in group B who initially had burning sensation had complete relief of pain during the treatment period and the abolishment of burning sensation endured till the end of the follow-up period. Burning sensation was alleviated but not abolished entirely also in the remaining two patients with baseline burning sensation in group A during the treatment period. In this group, one patient had some relapse in burning sensation during the follow-up period. His VAS score was 8 in the beginning, 4 after the treatment, and 6 in the end of the follow-up period.
Compared to the beginning of the study, burning sensation decreased significantly in all groups by the end of the follow-up period (A, p < 0.00001; B, p < 0.00001; C, p = 0.003; Fig. 2). The amount of decrease was comparable between groups A and B (p = 0.403) but significantly more in groups A and B compared to group C (A vs C, p < 0.00001; B vs C, p < 0.00001).
The time to obtain complete relief was significantly shorter (p = 0.001) in group B compared to group A. None of the patients in group C obtained complete relief, but in average, burning sensation was alleviated significantly at the end of the follow-up period (p = 0.003) but not yet at the end of the treatment period (p = 0.177).
Effect of treatments on histological findings
In all groups, the mean histological score corresponded to early stage oral submucous fibrosis (Table 3) as classified by Pindborg and Sirsat [10] (Table 1). The scoring of pretreatment samples did not differ significantly between the groups (data not shown). Individually histology ranged from very early to moderately advanced in groups A and C and from early to moderately advanced in group B. Post-treatment biopsy did not reveal any major improvement in histological scores. In groups A and C there was no change in the scores, whereas in group B slight but statistically nonsignificant improvement (p = 0.334) was observed.
Examination of individual histological features related to oral submucous fibrosis similarly revealed no major changes between pre- and post-treatment samples (Fig. 3). Altogether, in group A (105/120), group B (104/120), and in group C (73/80) features remained unchanged. Some improvement in epithelial signs of oral submucous fibrosis was observed altogether in 13/60 evaluations in group A, 11/60 in group B, and 2/40 in group C. The improvement was most commonly seen as decreased atrophy and hyper- or parakeratosis. In subepithelial tissue, only 1/60 evaluations in group A, 4/60 in group B, and 0/40 in group C were indicative of remission and seen as decreased inflammation or sclerosis and increased vascularity. Progressive signs of disease was observed in 1/120 evaluations in groups A and B, and in 5/80 evaluations in group C.
Analysis of changes in specific histological features in biopsy samples. Posttreatment samples were compared to pretreatment samples. The number of patients in each group with signs of remission, progression of disease or no change in a specific histological feature is presented. Patients in group A a received isoxsuprine tablets, group B b injections of dexamethasone and hyaluronidase and group C c placebo tablets
Discussion
In this study, we found a vasodilative agent, isoxsuprine, and dexamethasone with hyaluronidase injections combined to physiotherapy to have significantly better outcome in reducing burning sensation and in increasing mouth opening compared to physiotherapy alone in patients with oral submucous fibrosis. When dexamethasone with hyaluronidase was used, a complete cessation of burning sensation was achieved more rapidly than with isoxsuprine. Physiotherapy alone improved oral opening significantly but the improvement was significantly less than in groups receiving either isoxuprine or dexamethasone with hyaluronidase in addition. Physiotherapy also significantly reduced oral burning sensation but not as efficiently as the other two treatments. Significant histological improvement was not observed in any of the groups.
In oral submucous, fibrosis increased fibrosis invariably gives rise to obliteration of vascular lumen thereby reducing the blood supply. The rationale behind the use of peripheral vasodilator is to dilate the capillaries to help to restore the supply of nutrients and drainage of metabolic waste products in the diseased area. This is the first study in which a vasodilator isoxsuprine has been used for the treatment of oral submucous fibrosis. Isoxsuprine is a phenylalanine derivative of epinephrine [23]. It is a β-adrenoreceptor agonist which causes an overall increase in the cytosolic calcium concentration level that stimulates the production and release of several endothelium-derived vasodilators. In addition, isoxsuprine inhibits platelet aggregation and decreases blood viscosity.
Efficacy of isoxsuprine tablets was compared with intralesional injections of dexamethasone with hyaluronidase. Dexamethasone has anti-inflammatory properties. Diminished inflammation leads to decreased fibroblast proliferation and reduced collagen synthesis and consequently less fibrosis. Hyaluronidase decreases collagen formation and degrades hyaluronic acid. Therefore, hyaluronic acid may also soften the already formed fibrosis unlike.
In our study, isoxsuprine medication combined with physiotherapy improved mouth opening and reduced burning sensation significantly. Earlier another vasodilator, pentoxifylline, has been reported to relieve symptoms, increase mouth opening and improve oral function [21, 22]. In addition to vasodilation, pentoxifylline decreases platelet aggregation and adhesion and accumulation of collagen and has anti-inflammatory properties [24]. Thus, some its beneficial effects may in part be due to other effects than vasodilation. Based on our experience with isoxsuprine, vasodilation, however, also appears to be a significant mechanism in providing the relief in this group of drugs. Furthermore, isoxsuprine may have some still unknown effects that might affect positively on the symptoms.
In association with pentoxifylline use, mild gastric irritation and central nervous system symptoms were the reported side-effect from the treatment [21]. Although isoxsuprine may cause side-effects, such as facial flushing and with bigger doses tachycardia and hypotension [23] with the used dosage no side-effects were observed or reported.
Vasodilator nylindrin hydrochloride supplemented with vitamins A, E, B complex, iodine, placental extract, corticosteroids, and physiotherapy was reported to provide improved mouth opening in 62 % of patients [20]. Instead, a 4-week treatment with vasodilator buflomedical hydrochloride with vitamin B complex and topical triamcinolone did not significantly improve mouth opening but alleviated burning sensation in 88 % of the patients [16]. Of the studied vasodilators, isoxsuprine appears to be both effective and well tolerated with the used dosage.
Both isoxsuprine and dexamethasone with hyaluronidase treatments alleviated significantly burning sensation and increased mouth opening, but with isoxsuprine the relief in burning sensation was achieved in average later during the 4-week therapy. Based on our study, it is impossible to differentiate the effects of dexamethasone and hyaluronidase as the outcome resulted from combination therapy. Hyaluronidase was earlier shown to decrease burning sensation quicker than dexamethasone but with a shorter enduring effect, whereas a combination of these two medications was shown to give an even longer lasting relief [14].
Physiotherapy was found to significantly improve oral opening, but the increase was significantly greater in both treatment groups compared to physiotherapy alone group. Isoxsuprine and dexamethasone with hyaluronidase injections were found to increase oral opening equally well. One confounding factor in the interpretation of these results is the initial more restricted oral opening in the group receiving injection therapy compared to physiotherapy alone group. In accordance with our study, mouth opening exercises have also earlier been shown to increase mouth opening but instead was not shown to have effect on oral pain [18]. Interestingly, 4 weeks biweekly injections of hydrocortisone with hyaluronidase did not increase oral opening or reduce oral pain [18] suggesting that longer lasting cortisone preparation such as dexamethasone should be used instead if administered biweekly or that treatment should be repeated more frequently or be longer.
These results suggest that physiotherapy benefits the patients by improving oral opening and decreasing burning sensation and should therefore be recommended to all patients. When combined with either oral isoxsuprine or dexamethasone with hyaluronidase injections, a significant further increase in mouth opening and reduction in burning sensation can be achieved. Of these two, dexamethasone with hyaluronidase therapy alleviates the pain more rapidly. From the practical point of view, the benefit of isoxsuprine is that its use does not require frequent visits to the clinic. The risk of repeated dexamethasone with hyaluronidase injection is tissue atrophy and injury whereas isoxsuprine may have systemic side-effects at least with bigger doses. Studies with longer follow-up times are required to establish the duration of the relief of symptoms and the effect on progression of disease of varying severity, because the stage of the disease may affect the treatment response.
References
Tilakaratne WM, Klinikowski MF, Saku T, Peters TJ, Warnakulasuriya S (2006) Oral submucous fibrosis: review on aetiology and pathogenesis. Oral Oncol 42:561–568
Angadi PV, Rao SS (2011) Areca nut in pathogenesis of oral submucous fibrosis: revisited. Oral Maxillofac Surg 15:1–9
Rajalalitha P, Vali S (2005) Molecular pathogenesis of oral submucous fibrosis—a collagen metabolic disorder. J Oral Pathol Med 34:321–328
Harvey W, Scutt A, Meghji S, Canniff JP (1986) Stimulation of human buccal mucosa fibroblasts in vitro by betel-nut alkaloids. Arch Oral Biol 31:45–49
Scutt A, Meghji S, Canniff JP, Harvey W (1987) Stabilisation of collagen by betel nut polyphenols as a mechanism in oral submucous fibrosis. Experientia 43:391–393
Moutasim KA, Jenei V, Sapienza K, Marsh D, Weinreb PH, Violette SM, Lewis MP, Marshall JF, Fortune F, Tilakaratne WM, Hart IR, Thomas GJ (2011) Betel-derived alkaloid up-regulates keratinocytealphavbeta6 integrin expression and promotes oral submucous fibrosis. J Pathol 223:366–377
Angadi PV, Rao S (2010) Management of oral submucous fibrosis: an overview. Oral Maxillofac Surg 14:133–142
Kerr AR, Warnakulasuriya S, Mighell AJ, Dietrich T, Nasser M, Rimal J, Jalil A, Bornstein MM, Nagao T, Fortune F, Hazarey VH, Reichart PA, Silverman S, Johnson NW (2011) A systematic review of medical interventions for oral submucous fibrosis and future research opportunities. Oral Dis 17(Suppl 1):42–57
More CB, Das S, Patel H, Adalja C, Kamatchi V, Venkatesh R (2012) Proposed clinical classification for oral submucous fibrosis. Oral Oncol 48:200–202
Pindborg JJ, Sirsat SM (1966) Oral submucous fibrosis. Oral Surg Oral Med Oral Pathol 22:764–779
Khanna JN, Andrade NN (1995) Oral submucous fibrosis: a new concept in surgical management. Report of 100 cases. Int J Oral Maxillofac Surg 24:433–439
Chole RH, Gondivkar SM, Gadbail AR, Balsaraf S, Chaudhary S, Dhore SV, Ghonmode S, Balwani S, Mankar M, Tiwari M, Parikh RV (2012) Review of drug treatment of oral submucous fibrosis. Oral Oncol 48:393–398
Kakar PK, Puri RK, Venkatachalam VP (1985) Oral submucous fibrosis—treatment with hyalase. J Laryngol Otol 99:57–59
Gupta D, Sharma SC (1988) Oral submucous fibrosis—a new treatment regimen. J Oral Maxillofac Surg 46:830–833
Borle RM, Borle SR (1991) Management of oral submucous fibrosis: a conservative approach. J Oral Maxillofac Surg 49:788–791
Lai DR, Chen HR, Lin LM, Huang YL, Tsai CC (1995) Clinical evaluation of different treatmentmethods for oral submucous fibrosis. A 10-year experience with 150 cases. J Oral Pathol Med 24:402–406
Kumar A, Bagewadi A, Keluskar V, Singh M (2007) Efficacy of lycopene in the management of oral submucous fibrosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 103:207–213
Cox S, Zoellner H (2009) Physiotherapeutic treatment improves oral opening in oral submucous fibrosis. J Oral Pathol Med 38:220–226
Singh M, Niranjan HS, Mehrotra R, Sharma D, Gupta SC (2010) Efficacy of hydrocortisone acetate/hyaluronidase vs triamcinolone acetonide/hyaluronidase in the treatment of oral submucous fibrosis. Indian J Med Res 131:665–669
Sharma JK, Gupta AK, Mukhija RD, Nigam P (1987) Clinical experience with the use of peripheral vasodilator in oral disorders. Int J Oral Maxillofac Surg 16:695–699
Rajendran R, Rani V, Shaikh S (2006) Pentoxifylline therapy: a new adjunct in the treatment of oral submucous fibrosis. Indian J Dent Res 17:190–198
Mehrotra R, Singh HP, Gupta SC, Singh M, Jain S (2011) Pentoxifylline therapy in the management of oral submucous fibrosis. Asian Pac J Cancer Prev 12:971–974
Cook P, James I (1981) Cerebral vasodilators (second of two parts). N Engl J Med 305:1560–1564
Samlaska CP, Winfield EA (1994) Pentoxifylline. J Am Acad Dermatol 30:603–621
Conflict of interest
The authors declare that there are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bhadage, C.J., Umarji, H.R., Shah, K. et al. Vasodilator isoxsuprine alleviates symptoms of oral submucous fibrosis. Clin Oral Invest 17, 1375–1382 (2013). https://doi.org/10.1007/s00784-012-0824-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-012-0824-z