Abstract
Objectives
Melatonin is a hormone, which is involved in the control of the circadian rhythm, but also acts as an antioxidant and immune modulator. Previous studies reported decreased salivary and serum melatonin levels in periodontitis. This prospective cohort trial assessed the effect of non-surgical periodontal therapy on melatonin levels.
Methods
Salivary and serum samples of 60 participants (30 patients suffering from a severe generalized form of periodontitis, 30 healthy controls) were collected at baseline and 19 samples of periodontitis patients after treatment. Salivary and serum melatonin levels were determined by a commercially available ELISA kit and serum C-reactive protein (CRP) by a routine laboratory test.
Results
At baseline, periodontitis patients showed significantly increased serum CRP values and significantly decreased salivary melatonin levels compared to the control group. Clinical periodontal parameters significantly correlated with salivary melatonin levels and serum CRP. Periodontal therapy resulted in a recovery of the decreased salivary melatonin levels and a negative correlation was detected for the changes of salivary melatonin and the inflammatory parameter bleeding on probing. Serum melatonin levels showed no significant differences.
Conclusions
Salivary melatonin levels recovered after periodontal therapy and correlated with a decrease of local periodontal inflammation. This may imply the local involvement of melatonin in the pathogenesis of periodontitis due to its antioxidant abilities. However, the exact role of melatonin in periodontal disease remains to be investigated in future trials.
Clinical relevance
The present results suggest salivary melatonin as a risk indicator for the severity of periodontal disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Periodontitis is a chronic infectious inflammatory disease of the tissue surrounding and supporting the teeth. Overgrowth of several gram-negative bacteria in the dental plaque initiates the disease process by causing an excessive host immune response. Activation of the innate and adaptive immunity counteracts the bacterial attack, but at the same time causes destruction of the periodontal tissue by secreting high amounts of inflammatory cytokines, pro-osteoclastogenic factors, and matrix metalloproteinases [1, 2]. Furthermore, periodontal disease is associated with an imbalance in the oxidant/antioxidant systems [3, 4]. Periodontal therapy reduces inflammation of the periodontium and balances the oxidant/antioxidant status [5].
Melatonin, an indoleamine, is mainly produced by the pineal gland and secreted in a circadian rhythm [6]. It affects many physiologic processes, such as the control of circadian rhythm, the activation of the immune system, or the regulation of the body temperature [7]. The circadian secretion pattern of melatonin goes parallel in serum and saliva, but salivary melatonin levels do not constantly reflect absolute melatonin concentrations of the serum. In the bloodstream, melatonin can be bound to albumin or be present in a free fraction. Only the free melatonin fraction is able to diffuse passively into saliva [8]. As a second source, local release of melatonin from the submandibular glands has to be considered [9, 10].
In the oral cavity, particularly the antioxidant function of melatonin suggests its involvement in pathogenic processes of periodontal disease. Melatonin is a direct free radical scavenger and stimulates antioxidative enzymes and increases their efficiency [11]. Additionally, the metal binding capacity of melatonin inhibits microbial growth in vitro, especially of gram-negative microorganisms, which are mainly related to periodontal disease [12]. In murine macrophages, melatonin suppresses the production of nitric oxide and interleukin-6 induced by lipopolysaccharides of Prevotella intermedia [13]. So far, in periodontitis patients, melatonin levels in saliva, serum, and gingival crevicular fluid are reported to be decreased compared to healthy controls [14–16]. On the one hand, melatonin levels might be constantly lower and represent a risk indicator for the development of periodontal disease. On the other hand, melatonin levels might be depleted in response to an increased oxidative stress and the bacterial attack, which are both present in periodontitis. However, so far there is no proof of a functional role of melatonin in the oral cavity. This study aimed to assess the effect of periodontal therapy on salivary and serum melatonin levels.
Materials and methods
Patient recruitment
The present prospective cohort trial was performed at the Division of Conservative Dentistry and Periodontology (Bernhard Gottlieb School of Dentistry, Medical University of Vienna, Austria). The study protocol was approved by the ethics committee of the Medical University of Vienna (EK 623/2007). Written informed consent was obtained from all participants. This study included 60 participants: 30 patients suffering from a severe generalized form of periodontitis (28 patients with chronic and 2 with aggressive periodontitis according to the criteria of the AAP classification 1999 [17]; 21 to 49 years; 12 females and 18 males) and 30 periodontally healthy controls (23 to 51 years; 18 females and 12 males).
Clinical history was recorded for all participants (personal data and medical history). Exclusion criteria were defined as follows: periodontal treatment or antibiotic therapy within the last 3 months, presence of any systemic disease (e.g., diabetes mellitus, asthma, and malignancies), working in night shifts, xerostomia or any other disease of the salivary glands, less than 20 teeth, intake of any drug known to alter melatonin levels (e.g., for sleeping disorders) or to be immunosuppressive, usage of partial or total prosthesis, pregnancy or lactation, acute infection, immunodeficiency, history of radio- or chemotherapy, and any conditions necessitating antibiotic premedication for dental appointment.
Orthopantomograms were taken from each participant and additionally full-mouth periapical radiographs (parallel technique) were recorded for the periodontitis patients to determine radiographic loss of alveolar bone. Periodontitis patients presented a severe (loss of supporting bone ≥1/3 of the root length), generalized (≥ 30 % affected sites) periodontal disease [17]. The control group enclosed individuals without any history of periodontal disease and attachment loss as well as with probing pocket depths (PD) ≤ 3 mm and a papilla bleeding index (PBI) simplified <20 % to exclude the presence of gingivitis [18].
Clinical periodontal examination
PD, clinical attachment level (CAL), and bleeding on probing (BoP) were measured on six sites per tooth (distal, median, and mesial points at buccal and palatinal aspects) using a periodontal probe (CP12, Hu-Friedy, Leimen, Germany). BoP is expressed in percent (sites positive for bleeding multiplied by 100 divided by the amount of measured sites). Approximal plaque index (API) and PBI simplified were recorded. After periodontal therapy the periodontal status was recorded a second time [18, 19].
Non-surgical periodontal therapy
Non-surgical periodontal therapy included extraction of hopeless teeth, restorative therapy, replacement of marginally insufficient fillings and instruction of patients in oral hygiene. Scaling and root planing was performed under local anesthesia quadrant-wise within 2 weeks. Nine patients received additional antibiotic treatment after finishing subgingival debridement due to clinical appearance and severity of periodontal disease. No post-treatment complications were recorded in any patient. Eleven patients dropped out, because they did not follow the time schedule of the study design and/or due to poor compliance on oral hygiene instructions. Nineteen patients were followed up including reevaluation of the periodontal status and a second saliva sampling 2 to 3 months after the initial therapy. A precondition for recording the second periodontal status was an improved oral hygiene and bleeding score (API and PBI < 25 %). This procedure is in accordance with the “Viennese Treatment Strategy” [20, 21].
Saliva and serum collection and analysis
The sample collection was carried out between 8:00 and 11:00 a.m. at constant light conditions similar to previous studies [14–16, 22]. Participants were asked to refrain from eating, drinking (except water), smoking, chewing gum, brushing teeth, and using mouth rinsing solutions beginning at midnight before sampling occurred, to exclude any possible interferences. A second sampling after periodontal therapy was collected within the same hour of the day as the first sampling to minimize deviations due to circadian rhythm of melatonin. Similar to previous studies [14, 15, 22] stimulated salivary samples were collected. A saliva collection system® (Greiner Bio One, Kremsmuenster, Austria), which provides a reliable and accurate quantification of the recovered saliva volume compared to conventional methods [23–25], was used according to the manufacturer's instructions. Original saliva proportion was assayed photometrically by a Saliva Quantification Kit® (Greiner Bio One, Kremsmuenster, Austria) at 450 nm according to the manufacturer's instructions. Venous blood was drawn from the antecubital vein into serum gel tubes (Greiner Bio One, Kremsmuenster, Austria). Sera were isolated by centrifugation (10 min at 2,150×g at 4 °C). Salivary and sera samples were divided into aliquots and stored at −40 °C until further analysis.
Salivary and serum melatonin levels were determined using a commercially available ELISA kit (Non-Extraction Melatonin Saliva ELISA, IBL, Hamburg, Germany) according to the manufacturers' instructions. Optical densities were plotted against a standard curve and concentrations expressed as picograms per milliliter. The standard range of the ELISA for salivary melatonin was 0.5 to 50 pg/ml with an analytical sensitivity of 0.3 pg/ml. The standard range of the ELISA for serum melatonin was 3 to 350 pg/ml with an analytical sensitivity of 1.6 pg/ml. Serum levels of C-reactive protein (CRP) were measured on a Chemistry Immuno-System Olympus AU640. The assay (Olympus OSR6199, Olympus Diagnostics, Melville, NY) is linear from 0.08 to 80 mg/l and has a lower detection limit of 0.08 mg/l.
Statistical analysis
Normal distribution of the data was controlled graphically and by the Kolmogorov–Smirnov test. When normally distributed, an independent samples t test was performed; otherwise, the Mann–Whitney U test was applied. The differences of salivary melatonin levels of patients before and after treatment were analyzed by a paired t test. Differences in serum melatonin, serum CRP, PD, CAL, and BoP, respectively, were analyzed in a similar manner. To analyze the effect of age or intake of antibiotics, respectively, on the difference of salivary melatonin, linear regression models were calculated with the baseline values of salivary melatonin as additional independent variable. The correlations between the values of salivary and serum melatonin, PD, CAL, BoP, and serum CRP, respectively, before treatment were analyzed by Spearman correlations. Pearson correlations coefficient was applied to investigate possible correlations between salivary and serum melatonin levels before treatment as well as the change of salivary melatonin after treatment and the change in PD, CAL, BoP, and serum CRP, respectively. Statistical analyses were performed using R 2.11.0 [26] and SPSS Version 19.0 (SPSS, Chicago, IL, USA) and p values <0.05 were considered as statistically significant.
Results
Periodontal and inflammatory parameters of the study population at baseline
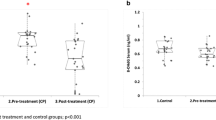
The clinical parameters PD, CAL and BoP, salivary and serum melatonin levels, and serum CRP levels of healthy individuals and periodontitis patients at baseline are given in Table 1 and Fig. 1. Before therapy, periodontitis patients showed significantly higher levels of PD (p < 0.001), CAL (p < 0.001), BoP (p < 0.001), and serum CRP (p = 0.011) compared to the control group.
Salivary melatonin levels (a), serum CRP levels (b), and BoP (c) of the control group and the periodontitis patients (perio) before and after therapy; data are expressed as mean ± S.E.M.; #p < 0.05, indicates significant differences between control and periodontitis group, *p < 0.05 indicates significant differences between before and after therapy
Effect of periodontal disease on melatonin levels
Salivary, but not serum melatonin levels were significantly decreased in the periodontitis group (saliva, p = 0.008; serum, p = 0.377). In the whole study population, there was a significant correlation between salivary and serum melatonin levels (rho = 0.392, p = 0.002). The correlations between salivary melatonin and serum CRP levels with clinical periodontal parameters (PD, CAL, and BoP) are presented in Table 2. Serum melatonin levels correlated neither with clinical periodontal parameters (p > 0.389) nor with serum CRP (p = 0.343).
Effect of periodontal treatment on melatonin levels
The effectiveness of periodontal therapy was proved by significantly decreased periodontal parameters (Table 3 and Fig. 1; PD, p < 0.001; CAL, p = 0.028; and BoP, p < 0.001). Serum CRP levels did not differ after periodontal therapy (Fig. 1; mean difference [95 % CI], −0.44 [−1.13; 0.25]; p = 0.20). Salivary melatonin levels increased following periodontal treatment (Fig. 1; mean difference [95 % CI], 2.43 [0.42; 4.44]; p = 0.021) and recovered after therapy to values comparable to those of the control group (Fig. 1; p = 0.340). The intake of antibiotics and age showed no significant effect on the change of salivary melatonin levels after periodontal treatment (p = 0.6 and p = 0.2). Serum melatonin levels were unaffected by periodontal treatment (Table 3; p = 0.21). A negative correlation was present between the change of salivary melatonin and BoP values (Fig. 2; rho = −0.53, p = 0.02). Other tested parameters (PD, CAL, and serum CRP) showed no significant negative correlation (p > 0.4).
Discussion
The present study confirmed previous reports on decreased melatonin levels in patients suffering from periodontal disease. In addition to that, we demonstrated for the first time a regeneration of salivary melatonin levels of periodontitis patients related to non-surgical periodontal therapy. The increase of salivary melatonin correlated significantly with the decrease of BoP, a clinical parameter indicating local inflammation.
Periodontitis and periodontal tissue destruction may be triggered by a shortage of antioxidants to balance increased oxidative stress [4, 27]. In the oral cavity, melatonin acts as an antioxidative, anti-inflammatory, and bone-preserving agent suggesting a role in periodontal disease [28–30]. So far, decreased serum and salivary melatonin levels in periodontitis patients were described in several studies [14–16, 22], which is confirmed by the present study. Salivary melatonin levels in periodontitis patients were decreased by one third before therapy compared to the healthy controls. Yet, in contrast to previous studies, which used an index to classify periodontal disease, this is the first study to prove a significant correlation of salivary melatonin levels with full-mouth assessed clinical periodontal parameters. Serum melatonin levels were not influenced by the presence of periodontal disease, although changed serum CRP levels confirmed a systemic involvement. Serum CRP levels were three times increased in periodontitis patients and correlated significantly with clinical periodontal parameters confirming the presence and severity of periodontal disease both locally and systemically in coincidence with the existing literature [31–33]. On the one hand, melatonin levels in the oral cavity could be constantly lower and represent a risk indicator for the development of periodontal disease. On the other hand, melatonin levels might be depleted in periodontal disease in response to increased oxidative stress and bacterial attack.
After successful non-surgical periodontal therapy, salivary melatonin levels were significantly increased by about 25 % and negatively correlated with a decrease of local inflammation. Reducing the inflammation seems to allow a recovery of salivary melatonin levels and indicates a reestablishment of the homeostasis of the oxidant/antioxidant system in the oral cavity. A modulatory effect of non-surgical periodontal therapy on the oxidant/antioxidant system locally and systemically was described previously by assessing other parameters, such as the total antioxidant capacity or reactive oxygen metabolites in the serum, saliva, or gingival crevicular fluid [5, 27]. A recent publication on a direct production of melatonin by the salivary glands supports the local role of melatonin [10], and further, a melatonin receptor was detected in the rat buccal mucosa and in human and mouse dental structures, indicating a role of melatonin during tooth development as well [7, 10]. In this study, the effect of the severity of periodontal inflammation on melatonin levels was assessed, but not, whether there is a difference between aggressive and chronic periodontitis. Until now, there is no report showing a difference of melatonin levels due to different types of periodontal disease. In the present study, only two patients with aggressive periodontitis (according to the criteria of the AAP classification 1999 [17]) were included, which did not influence the results on salivary melatonin levels. Because of limited sample number in this study comparison of melatonin levels between these two types of periodontitis was not performed. It remains an interesting aspect for future clinical trials with an increased sample size to investigate, whether there is a difference between aggressive and chronic periodontitis. Altogether, this clinical trial implies salivary melatonin as a risk indicator for the severity of periodontal disease. Still a functional role of melatonin in periodontal disease needs to be further investigated in future studies.
In view of the biorhythm of melatonin, the optimal sampling time for melatonin would be between 12:00 and 2:00 a.m. due to maximal secretion of melatonin. For feasibility in a clinical trial, the samples were collected at about 8:00 a.m. in the morning in the present study similar to previous studies [14–16, 22]. The aim of this study was to assess the influence of periodontal therapy on melatonin levels. Therefore, the sample collection was performed at the same time point before and after therapy to avoid the influence of the circadian rhythm of each participant, but melatonin levels of this study population do not represent the peak of secretion.
Numerous studies suggest a positive effect of melatonin on periodontal disease [11, 13, 34]. Firstly, melatonin functions as a direct free radical scavenger, reduces free radical generation, stimulates other antioxidative enzymes, and increases their efficiency [11]. Melatonin, for example, is able to detoxify nitric oxide, whose synthesis is increased in periodontal diseased tissue [11, 35]. Secondly, immuno-modulating effects of melatonin on the function of macrophages or leukocytes are reported. In murine macrophages, melatonin suppresses the production of nitric oxide and interleukin-6 induced by lipopolysaccharides of P. intermedia [13]. In acute pyelonephritis in rats, exogenously administered melatonin reduces neutrophil infiltration and production of inflammatory mediators [34]. Similar effects of melatonin in the oral cavity might modulate the immune response during periodontal inflammation, which is initiated by the bacterial attack and is primarily responsible for the hard and soft tissue damage. In vivo, intravenous melatonin administration significantly decreased inflammatory (interleukin-6, -8, and tumor necrosis factor alpha) and oxidative (nitrite/nitrate levels) parameters in children with respiratory distress syndrome [36]. Further, melatonin has a metal-chelating capacity for iron (III), copper, and zinc, which causes a reduction of their cytoplasmic availability and is related to the antioxidant properties of melatonin by making transition metals unavailable for the Fenton reaction. Further, binding free iron inhibits particularly the growth of gram-negative bacteria, which are mainly responsible for periodontal disease [12, 37]. Finally, melatonin seems to influence bone turnover. It stimulates osteoblast differentiation, bone formation and production of collagen type I and suppresses bone resorption and osteoclast formation [38–40] and recently, a potential beneficial effect of melatonin on the repair of bony defects by promoting angiogenesis was shown in an in vivo animal study [41].
The combination of the various properties (antioxidative, immune-modulatory, antibacterial, and promoting bone formation) may address melatonin or its derivatives as an interesting adjuvant in the treatment of periodontal diseases. Melatonin is non-toxic and highly lipophilic, diffuses rapidly into all body fluids, cells and subcellular compartments and is an uncommonly safe molecule over a wide range of doses [42]. Until now, melatonin is applied as therapeutic agent in sleeping disorders (e.g., jet lag, shift work, or sleep deterioration associated with aging) and as an adjuvant therapy for reduced cytotoxicity during chemo- or radiotherapy in cancer treatment, for macular degeneration or irritable bowel syndrome [43–45]. In the oral cavity the local application of melatonin into the alveolar socket after tooth extraction decreases the oxidative stress in beagle dogs [46]. Further, melatonin improves osseointegration of dental implants in animal studies [47–50].
Conclusions
In conclusion, this study implied that salivary melatonin levels may be related to periodontal inflammation possibly due to its antioxidant abilities: Before therapy, salivary melatonin levels were lower in periodontitis patients compared to healthy controls and significantly correlated with clinical periodontal parameters. Further, after non-surgical periodontal therapy, a recovery of the decreased salivary melatonin levels and a significantly negative correlation to the reduction of local inflammation was proved. This melatonin response was only detectable in saliva and not in the serum. However, elevated serum CRP levels confirmed a systemic involvement of periodontal disease. These results suggest salivary melatonin as a risk indicator for the severity of periodontal disease. Further research is required to clarify the mechanisms of melatonin in the pathogenesis of periodontal disease and to understand its clinical relevance.
References
Brook I (2003) Microbiology and management of periodontal infections. Gen Dent 51:424–428
Holtfreter B, Kocher T, Hoffmann T et al (2010) Prevalence of periodontal disease and treatment demands based on a German dental survey (DMS IV). J Clin Periodontol 37:211–219
Akalin FA, Toklu E, Renda N (2005) Analysis of superoxide dismutase activity levels in gingiva and gingival crevicular fluid in patients with chronic periodontitis and periodontally healthy controls. J Clin Periodontol 32:238–243
Sculley DV, Langley-Evans SC (2002) Salivary antioxidants and periodontal disease status. Proc Nutr Soc 61:137–143
Wei D, Zhang XL, Wang YZ et al (2010) Lipid peroxidation levels, total oxidant status and superoxide dismutase in serum, saliva and gingival crevicular fluid in chronic periodontitis patients before and after periodontal therapy. Aust Dent J 55:70–78
Reiter RJ (1991) Pineal melatonin: cell biology of its synthesis and of its physiological interactions. Endocr Rev 12:151–180
Kumasaka S, Shimozuma M, Kawamoto T et al (2010) Possible involvement of melatonin in tooth development: expression of melatonin 1a receptor in human and mouse tooth germs. Histochem Cell Biol 133:577–584
Laakso ML, Porkka-Heiskanen T, Alila A et al (1990) Correlation between salivary and serum melatonin: dependence on serum melatonin levels. J Pineal Res 9:39–50
Cutando A, Aneiros-Fernandez J, Lopez-Valverde A et al (2011) A new perspective in oral health: potential importance and actions of melatonin receptors MT1, MT2, MT3, and RZR/ROR in the oral cavity. Arch Oral Biol 56(10):944–950
Shimozuma M, Tokuyama R, Tatehara S et al (2011) Expression and cellular localizaion of melatonin-synthesizing enzymes in rat and human salivary glands. Histochem Cell Biol 135:389–396
Reiter RJ, Tan DX, Mayo JC et al (2003) Melatonin as an antioxidant: biochemical mechanisms and pathophysiological implications in humans. Acta Biochim Pol 50:1129–1146
Tekbas OF, Ogur R, Korkmaz A et al (2008) Melatonin as an antibiotic: new insights into the actions of this ubiquitous molecule. J Pineal Res 44:222–226
Choi EY, Jin JY, Lee JY et al (2011) Melatonin inhibits Prevotella intermedia lipopolysaccharide-induced production of nitric oxide and interleukin-6 in murine macrophages by suppressing NF-kappaB and STAT1 activity. J Pineal Res 50(2):197–206. doi:10.1111/j.1600-079X.2010.00829.x
Cutando A, Gomez-Moreno G, Villalba J et al (2003) Relationship between salivary melatonin levels and periodontal status in diabetic patients. J Pineal Res 35:239–244
Gomez-Moreno G, Cutando-Soriano A, Arana C et al (2007) Melatonin expression in periodontal disease. J Periodontal Res 42:536–540
Srinath R, Acharya AB, Thakur SL (2010) Salivary and gingival crevicular fluid melatonin in periodontal health and disease. J Periodontol 81:277–283
Armitage GC (1999) Development of a classification system for periodontal diseases and conditions. Ann Periodontol 4:1–6
Saxer UP, Muhlemann HR (1975) Motivation and education. SSO Schweiz Monatsschr Zahnheilkd 85:905–919
Lange DE, Plagmann HC, Eenboom A et al (1977) Clinical methods for the objective evaluation of oral hygiene. Dtsch Zahnarztl Z 32:44–47
Bruckmann C, Durstberger G, Matejka M (2006) The “Viennese Treatment Strategy”. Part II. Stomatologie 103(1):11–16
Durstberger G, Bruckmann C, Matejka M (2006) The “Viennese treatment strategy”. Part II. Stomatologie 103(2):33–38
Cutando A, Galindo P, Gomez-Moreno G et al (2006) Relationship between salivary melatonin and severity of periodontal disease. J Periodontol 77:1533–1538
Bertl K, Haririan H, Laky M et al (2012) Smoking influences salivary histamine levels in periodontal disease. Oral Dis 18:410–416
Haririan H, Bertl K, Laky M et al (2012) Salivary and serum chromogranin A and alpha-amylase in periodontal health and disease. J Periodontol. doi:10.1902/jop.2012.110604
Raggam RB, Santner BI, Kollroser M et al (2008) Evaluation of a novel standardized system for collection and quantification of oral fluid. Clin Chem Lab Med 46:287–291
Team RDC (2010) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna
Tamaki N, Tomofuji T, Ekuni D et al (2009) Short-term effects of non-surgical periodontal treatment on plasma level of reactive oxygen metabolites in patients with chronic periodontitis. J Periodontol 80:901–906
Cutando A, Gomez-Moreno G, Arana C et al (2007) Melatonin: potential functions in the oral cavity. J Periodontol 78:1094–1102
Reiter RJ, Tan DX, Manchester LC et al (2007) Medical implications of melatonin: receptor-mediated and receptor-independent actions. Adv Med Sci 52:11–28
Tan DX, Chen LD, Poeggeler B, Manchester LC, Reiter RJ (1993) Melatonin: a potent, endogenous hydroxyl radical scavenger. Endocr J 1:57–60
Andrukhov O, Ulm C, Reischl H et al (2010) Serum cytokine levels in periodontitis patients in relation to the bacterial load. J Periodontol 82(6):885–892
Nakajima T, Honda T, Domon H et al (2010) Periodontitis-associated up-regulation of systemic inflammatory mediator level may increase the risk of coronary heart disease. J Periodontal Res 45:116–122
Shimada Y, Komatsu Y, Ikezawa-Suzuki I et al (2010) The effect of periodontal treatment on serum leptin, interleukin-6, and C-reactive protein. J Periodontol 81:1118–1123
Sener G, Tugtepe H, Velioglu-Ogunc A et al (2006) Melatonin prevents neutrophil-mediated oxidative injury in Escherichia coli-induced pyelonephritis in rats. J Pineal Res 41:220–227
Matejka M, Partyka L, Ulm C et al (1998) Nitric oxide synthesis is increased in periodontal disease. J Periodontal Res 33:517–518
Gitto E, Reiter RJ, Cordaro SP et al (2004) Oxidative and inflammatory parameters in respiratory distress syndrome of preterm newborns: beneficial effects of melatonin. Am J Perinatol 21:209–216
Gulcin I, Buyukokuroglu ME, Kufrevioglu OI (2003) Metal chelating and hydrogen peroxide scavenging effects of melatonin. J Pineal Res 34:278–281
Koyama H, Nakade O, Takada Y et al (2002) Melatonin at pharmacologic doses increases bone mass by suppressing resorption through down-regulation of the RANKL-mediated osteoclast formation and activation. J Bone Miner Res 17:1219–1229
Nakade O, Koyama H, Ariji H et al (1999) Melatonin stimulates proliferation and type I collagen synthesis in human bone cells in vitro. J Pineal Res 27:106–110
Roth JA, Kim BG, Lin WL et al (1999) Melatonin promotes osteoblast differentiation and bone formation. J Biol Chem 274:22041–22047
Ramirez-Fernandez MP, Calvo-Guirado JL, Sanchez de-Val JES et al (2012) Melatonin promotes angiogenesis during repair of bone defects: a radiological and histomorphometric study in rabbit tibiae. Clin Oral Investig. doi:10.1007/s00784-012-0684-6
Gomez-Moreno G, Guardia J, Ferrera MJ et al (2010) Melatonin in diseases of the oral cavity. Oral Dis 16:242–247
Dodson ER, Zee PC (2010) Therapeutics for circadian rhythm sleep disorders. Sleep Med Clin 5:701–715
Miller SC, Pandi-Perumal SR, Esquifino AI et al (2006) The role of melatonin in immuno-enhancement: potential application in cancer. Int J Exp Pathol 87:81–87
Sanchez-Barcelo EJ, Mediavilla MD, Tan DX et al (2010) Clinical uses of melatonin: evaluation of human trials. Curr Med Chem 17:2070–2095
Cutando A, Arana C, Gomez-Moreno G et al (2007) Local application of melatonin into alveolar sockets of beagle dogs reduces tooth removal-induced oxidative stress. J Periodontol 78:576–583
Calvo-Guirado JL, Gomez-Moreno G, Barone A et al (2009) Melatonin plus porcine bone on discrete calcium deposit implant surface stimulates osteointegration in dental implants. J Pineal Res 47:164–172
Calvo-Guirado JL, Gomez-Moreno G, Lopez-Mari L et al (2010) Actions of melatonin mixed with collagenized porcine bone versus porcine bone only on osteointegration of dental implants. J Pineal Res 48:194–203
Cutando A, Gomez-Moreno G, Arana C et al (2008) Melatonin stimulates osteointegration of dental implants. J Pineal Res 45:174–179
Takechi M, Tatehara S, Satomura K et al (2008) Effect of FGF-2 and melatonin on implant bone healing: a histomorphometric study. J Mater Sci Mater Med 19:2949–2952
Acknowledgments
The authors thank Mrs. Hedwig Rutschek and Mrs. Phuong Quynh Nguyen (laboratory technicians of the Bernhard Gottlieb School of Dentistry, Medical University of Vienna, Austria) for their excellent work in preparing and performing the experiments. Greiner Bio One supported this study by financing materials (reagents and saliva collection system) (Medical University of Vienna, §26, project number AP00345OFF).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bertl, K., Schoiber, A., Haririan, H. et al. Non-surgical periodontal therapy influences salivary melatonin levels. Clin Oral Invest 17, 1219–1225 (2013). https://doi.org/10.1007/s00784-012-0801-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-012-0801-6