Abstract
Objectives
The aim of this study was to assess the relationship between tooth loss, toothbrushing behaviour, diabetes type 2 (DM2), obesity and sleep apnea among diabetics.
Material and methods
DM2 patients (n = 165) in Istanbul, Turkey, were randomly selected from the outpatient clinics of two hospitals. Baseline clinical measurements (HbA1c, fasting blood glucose, high-density lipoprotein (HDL), low-density lipoprotein (LDL), body mass index (BMI), body-fat proportion, tooth loss) and self-administered questionnaires (toothbrushing, gingival bleeding, sleep apnea) provided data for factor and principal component analysis with Varimax rotation. Univariate statistics and chi-square tests were derived.
Results
Mean maxillary tooth loss (4.49 ± 3.69 teeth) was higher than in the mandible (3.43 ± 3.12 teeth, p< 0.001). Favourable HDL was measured among most patients (77 %); other favourable clinical measures occurred only in a minority of participants (HbA1c, 28 %; fasting blood glucose, 17 %; LDL, 30 %). Twice daily toothbrushing was reported by 33 % (17 %) for healthy BMI; 37 % when healthy body-fat proportions. There was risk of sleep apnea in 37 %. The higher number of lost teeth in the maxilla was linked with obesity and sleep apnea. Non-daily toothbrushers were more likely to have high LDL and low HDL cholesterol and a higher risk of sleep apnea. When “at least occasionally” bleeding on toothbrushing occurred, higher HbA1c levels and sleep apnea were more likely.
Conclusion
Oral care with early diagnosis and monitoring of glycaemic level can help prevent complications of DM2.
Clinical relevance
Dentists may play a key role in better managing and diagnosing sleep apnea early by referring the patients with severe tooth loss and periodontal disease for general medical examination.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Oral diseases (dental caries and periodontal diseases), diabetes type 2 (DM2) and obesity, largely preventable chronic diseases, are claimed to be present at pandemic levels and have severe consequences [1–4]. WHO has called for global action to prevent these diseases, a vital need requiring urgent investment [1, 3].
Current scientific evidence suggests that oral diseases, DM2, and obesity share common risk factors (poor dietary habits, a sugar-rich diet, smoking) [5–9] and biologic mechanisms [10–15]. Periodontal disease, one of the most common oral diseases, is a major cause of tooth loss. Studies establishing the relationship between DM2, periodontal health and subsequent tooth loss have been widely reported [16–18]. Obesity is a significant risk factor for DM2 and periodontal diseases [12, 13] and tooth loss [19, 20]. However, there has been no study, to our knowledge, on the links between DM2 and obesity and tooth loss.
Obstructive sleep apnea (OSA) is a common and treatable form of sleep-disordered breathing involving upper airway collapse during sleep [21]. Obesity is recognized as the strongest risk factor for OSA [22, 23]. It is unknown whether DM2 contributes to the development or aggravation of OSA, although this is likely [21]. Conversely, OSA may be a risk factor for DM2; strong evidence suggests that OSA may increase the risk of developing DM2. Tooth loss may favour the occurrence of OSA; the absence of teeth produces prominent anatomical changes that may influence upper airway size and function, such as loss of the vertical dimension of occlusion, reduction of the lower face height and mandible rotation [24]. The role of tooth loss in OSA has been a neglected issue.
The present study aimed to assess the links between tooth loss, oral health behaviour, DM2, obesity and sleep apnea among patients with DM2.
Methodology
The present study is part of a prospective three-stage (baseline initiation, maintenance and follow-up) intervention study among DM2 patients, Istanbul, Turkey (n = 200), who were randomly selected from the outpatient clinics of two hospitals. The power and sample size is calculated by G*power (effect size, w = 0.5–0.7, α err prob = 0.05, power (1 − β err prob) = 0.95) [25]. The eligibility criteria for the patients were age 30–65 years with at least four functional teeth, no psychological treatment and no hospitalization.
The data in the present study come from the baseline measurements. The data for the prospective study were collected initially and at the end of each of the three stages by (1) clinical measurements (body mass index (BMI), body-fat proportion, oral health) and (2) self-assessed questionnaires (including health behaviour questions and modified scales from well-known and widely used scales, e.g. PAID [26] and WHOQL-Bref [27]).
Ethical approval and written permission were granted by the Ministry of Health to conduct the study. The research was announced at the outpatient clinics by pamphlets, brochures, physicians and the head nurses. At baseline, patients interested in participating in the study were selected according to the eligibility criteria. Verbal and written information about the study were provided and then informed consent was obtained from patients. Afterwards, self-assessed questionnaires were distributed and collected on the same day. Following this step, participants were invited to the clinics for oral (caries and periodontal diseases) and general health examination (BMI, body-fat proportion) for the following week. Of the participating patients (n = 178, 89 % of the total), 95 % (n = 170) answered the questionnaires and 93 % (n = 165) participated in oral examinations. The characteristics of the participants are shown in Table 1.
Back-translation to and from Turkish was done for health behaviour questionnaires by two native speakers to ensure comparability with the original forms in English. The variables extracted for analysis from the main intervention study were as follows:
-
1.
Number of teeth lost, measured by the oral examinations: The number of teeth missing was recorded from the records of oral health examinations in the main study, which included examination of dental health status according to the International Caries Detection System criteria [28] and periodontal health by the Community Periodontal Need Index (CPI) and Periodontal Attachment Loss (PAL) [29]. All dental examinations were carried out by two dentists (Oktay I and Cinar AB), both with previous experience and accreditation in dental public health, and one periodontologist, (İlhan D) who was accredited in the measurement of CPI and PAL.
The numbers of missing teeth in each dental arch were categorised as two separate variables, and the sum of missing teeth was used to generate a third variable, “total loss”. For further analysis, variables were dichotomized using the means as cut points; the categories were “below mean” = 0 and “mean and above” = 1.
-
2.
Oral health behaviour: Self-reported toothbrushing frequency (TB) and gingival bleeding on the questionnaires were determined as follows: “How often do you brush teeth?” and “Have you ever observed your gums bleeding whilst brushing your teeth?” These measures were recorded on a five-point Likert scale ranging from “never” to “twice daily” and “always” to “never”. Self-reported TB was reclassified into “less than once a day”, “once a day” and “twice a day”. Self-reported gingival bleeding was classified into three categories: “never”, including “never or rarely”, “occasionally” and “usually”, consisting of “usually” or “always”. For further analysis, the variables were dichotomized (brushing daily = 0 vs. brushing less than daily = 1, gingival bleeding rarely = 0 vs. gingival bleeding at least occasionally = 1).
-
3.
Diabetes management: Glycated haemoglobin (HbA1c) results are expressed as the proportion of haemoglobin that is exposed to glucose [30]. Taking the target levels (HbA1c, <6.5 %; fasting blood glucose, <110 mg/dl; high-density lipoprotein (HDL), >39 mg/dl and low-density lipoprotein (LDL), <95 mg/dl) [30] as the cut points, the respective variables taken from the most recent health records were dichotomized as “favourable” = 0 and “unfavourable” = 1.
-
4.
Obesity: BMI was measured by the Tanita TBF-300-A Body Composition Analyzer and Scale. Weight and height, as anthropometric measures, were used to determine BMI [(weight in kilograms)/(height in metres)2]. A specifically trained researcher (AB Cinar) under the supervision of clinically accredited head nurses measured height to the nearest 0.1 cm according to accepted standards, using a portable stadiometer, in the outpatient clinics. In brief, the patients stood straight, with bare feet placed together and flat on the ground, arms loose and relaxed with the palms facing medially. Body weight was measured to the nearest 0.1 kg, with patients lightly dressed in bare feet, by Tanita TBF-300-A. Tanita TBF-300-A uses foot-to-foot bioelectrical impedance analysis to measure patients’ body composition (body weight, impedance, body-fat proportion, BMI, lean mass). For foot-to-foot BIA conduction, patients stood erect with bare feet on the analyser footpads. According to the current World Health Organization BMI cutoff points [31], BMI was categorised as follows: <18.49 kg/m2 (underweight), 18.5–24.9 kg/m2 (normal/healthy range), 25.0–29.9 kg/m2 (overweight/pre-obese), 30.0–34.9 kg/m2 (obese class I), 35–39.9 kg/m2 (obese class II) and 40.0 kg/m2 (obese class III). There were no patients in the underweight category; those who were overweight and obese (classes I–III, 29.4 %, 12.5 % and 7.5 %, respectively) were classified as obese for further analysis.
The body-fat proportion was also measured by the Tanita TBF-300-A, and the ideal range proportions were specified for gender, age and height and digitally calculated by the apparatus. Therefore, a patient’s body-fat proportion was compared with his/her ideal value, and in further analysis, this was recorded as a new variable, “ideal fat” (yes = 0 vs. no = 1-over fat-); there were no patients with body-fat proportions under the ideal range.
-
5.
Sleep apnea probability was assessed by four questions which were recorded using a five-point scale (0 = “never”, 1 = “seldom”, 2 = “sometimes”, 3 = “often”, 4 = “very often”): (a) “How often do you wake up during the night?”; (b) “Do you feel excessively sleepy during the daytime?”; (c) “Do you snore loudly?”; and (d) “Do you fall asleep involuntarily during the daytime?” Based on earlier studies by Tuomilehto [32] and Partinen [33], the sum of these four questions was used to estimate sleep apnea probability. For further analysis, the variable was dichotomized using the mean (7.69) as the cut point. The categories were moderate risk (below mean, score 0) and high risk (mean or above, score 1).
Statistical methods
Factor analysis was applied to these variables using principal component analysis and Varimax rotation to analyse the interrelationships and common underlying dimensions among dental health, obesity and lifestyle factors by classifying these variables into discriminative clusters, so called components, based on their factorial loadings, ranging from the highest to the lowest values, among patients with DM2. Factors were extracted according to meeting the Kaiser criterion of eigenvalue >1.
Descriptive statistics, frequency distributions and the contingency coefficient for determining associations between variables were applied. In addition, chi-square tests by cross-tabulation were applied to compare proportions and corresponding odds ratios were calculated. Statistical significance was set at p < 0.05.
Results
The mean number of teeth lost was 7.92 (±6.04); the mean in the maxilla (4.49 ± 3.69 teeth) was significantly higher than in the mandible (3.43 ± 3.12 teeth, p < 0.001). The mean for HbA1c and fasting blood glucose were respectively 7.5 (±1.65) and 162.2 (±69.7). Favourable clinical measures (HbA1c < 6.5 %, fasting blood glucose < 110 mg/dl, HDL > 39 mg/dl and LDL < 95 mg/dl) were reported among a minority of patients (HbA1c = 28 %, fasting blood glucose = 17 %, LDL = 30 %), except that a majority of patients reported favourable HDL (77 %).
More than half of the patients brushed their teeth at least once a day (60 %; daily, 33 %; two or three times daily, 27 %; Table 1). Self-reported gingival bleeding “at least occasionally” was reported by 66 % of the participants. Among these, those brushing their teeth less than daily were more likely to have bleeding on brushing (45 %) compared with once-daily (34 %) and twice-daily toothbrushers (21 %, p < 0.001). Toothbrushing frequency was negatively correlated with fasting blood glucose (r s = −0.18, p < 0.005) and positively with HDL (r s = 0.23, p < 0.001).
A minority of patients had healthy BMI (17 %) and ranged within the healthy body-fat proportions (37 %). The mean BMI was 30.59 (±5.77) and the mean for body-fat proportion was 27.75 (±11.77). BMI was positively correlated with body-fat proportion (r s = 0.85, p < 0.001). BMI and ideal body-fat proportion were positively correlated with HbA1c (r s = 0.24, p < 0.001; r s = 0.20, p < 0.05). BMI was negatively correlated with HDL (r s = −0.25, p < 0.005). The same association was observed between HDL and fasting blood glucose level (r s = −0.27, p < 0.001).
A high risk of sleep apnea was estimated in 37 % of the participants. The increased risk of sleep apnea was positively correlated with BMI (r s = 0.42), having over fat (r s = 0.324) and HbA1c (r s = 0.21, p < 0.001); it was negatively correlated with self-reported gingival bleeding (r s = −0.21, p < 0.001). The patients reporting “gingival bleeding at least occasionally on brushing” were more likely to have a higher mean of sleep apnea (8.24 ± 2.97) compared with those reporting “gingival bleeding rarely on brushing” (6.72 ± 2.83, p < 0.05). Patients who were obese and having excess fat were more likely to have a “high risk” of sleep apnea compared with those with healthy BMI and body-fat proportion in the normal ranges (OR = 6.47, 95% CI = 1.58–26.3; OR = 1.83, 95% CI = 1.06–3.01).
Total tooth loss was positively correlated with BMI (r s = 0.22) and sleep apnea (r s = 0.24, p < 0.005; Table 2). The same correlations applied to maxillary tooth loss (r s = −0.21 and r s = −0.25, p < 0.005). The number of teeth lost in the upper jaw was also correlated with HbA1c (r s = 0.19, p < 0.005). Patients with below average maxillary tooth loss were more likely to have healthy BMI (OR = 3.26, 95% CI = 1.14–9.35) and favourable fasting blood glucose (OR = 3.26, 95% CI = 1.03–10.28) than those who had lost above average number of teeth (p < 0.005). There was no significant difference for maxillary tooth loss between those with normal body-fat proportion and those with over fat (p = 0.057).
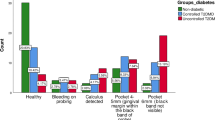
Principal component analysis revealed that the increased number of teeth lost in the upper jaw was correlated with obesity and high risk of sleep apnea (Table 3). Those who brushed their teeth daily were more likely to have high HDL and low LDL. Those who reported gingival bleeding at brushing “at least occasionally” were more likely to have higher HbA1c levels.
Discussion
DM2 patients are more likely to have deep periodontal pockets and to lose teeth than non-diabetic controls [16]. Recent research supports the bidirectional relationship between diabetes and periodontal disease; poor oral health negatively contributes to glycaemic control, whereas poor DM2 management negatively affects oral health [15, 18]. The level of glycaemic control is of key importance in determining increased risk of periodontal disease [34, 35] and subsequent tooth loss [18]. In line with these findings, the present research found that HbA1c was correlated with the total number of teeth lost and the numbers lost in each jaw. HbA1c and the number of teeth lost in the upper jaw were positively correlated with self-reported gingival bleeding, suggesting that these three factors share lifestyle or pathogenic factors or factors such as an increased inflammatory reaction due to destruction of the periodontal tissue. Therefore, gingival bleeding observed by the patient may signify initial inflammation, which may lead to periodontal tissue destruction, subsequent tooth loss and an increase in blood glucose. Self-reported gingival bleeding may thus be looked on as an early risk indicator of tooth loss and high HbA1c levels.
Toothbrushing is the most effective life-long method for reducing inflammation and subsequent tooth loss [36]; thus, it may improve diabetes management. The frequency of toothbrushing and the link with diabetes have been relatively little studied. Lower toothbrushing frequency is related to a higher prevalence of diabetes mellitus, measured in terms of fasting blood glucose levels, high LDL and low HDL [37]. Syrjälä et al. [38] showed that toothbrushing frequency was positively correlated with diabetes adherence (regular measurement of blood glucose, adjustment of insulin to exercise and meal times, diet, and exercise). In line with these findings, in the present study, toothbrushing frequency among DM2 patients was positively correlated with HDL and negatively with fasting blood glucose. This may be explained as follows: Toothbrushing removes the principal aetiologic factor in periodontal disease, plaque, from all surfaces of the teeth; it decreases mean pocket depth [39] and, thereby, the inflammatory reactions, which increase in periodontal disease [12]. Periodontal disease is a common chronic subclinical inflammation associated with increased levels of pro-atherogenic plasma lipoproteins (cholesterol, in particular LDL) [40, 41]. Periodontal disease and fasting blood glucose are correlated; hyperglycaemia, resulting from impaired fasting blood glucose, may increase the risk of periodontal disease, but chronic systemic inflammation from periodontal disease may also stimulate inflammatory cytokines (C-reactive protein, tumour necrosis factor a and interleukin-6), leading to hyperglycaemia [12, 42, 43]. Our findings imply that people with DM2 may need to be evaluated for daily oral health care habits. It is also possible that regular toothbrushing may contribute to the reduction of high fasting blood glucose levels and to the increase of HDL among patients with DM2. This should be verified in future studies as the present study is among the extremely few publications [37], to our knowledge, that investigate the link between toothbrushing frequency and diabetes management, measured in terms of fasting blood glucose, LDL and HDL.
Obstructive sleep apnea (OSA) is an increasingly common sleep disorder. It is characterized by repetitive upper airway obstructions leading to intermittent hypoxia and sleep fragmentation, mostly due to frequent pharyngeal obstruction and collapse. Obesity [44] and several structural changes in facial morphology (retrognathic mandibles, posteriorly placed pharyngeal walls) [45], have been implicated as contributing factors. Based on recent literature, there are complex interactions among obesity, DM2 and OSA involving multiple pathways [22, 46, 47]. The link between tooth loss and these three factors may provide new insights into public health. The role of tooth loss in the pathogenesis of OSA has been a neglected issue. Bucca et al. [24] have found that complete tooth loss favours upper airway obstruction during sleep by modifying the anatomy and function of the pharyngeal airway and the tongue and by favouring inflammatory oedema. In that study, the number of apnoea/hypopnoea episodes and oxygen saturation were greater in patients with tooth loss. Recurrent obstructive events with intermittent hypoxia and sleep fragmentation in OSA are primary triggers for a disturbance in pathogenetic mechanisms [48] and may modulate systemic inflammation [49]. The risk of systemic inflammation is already elevated among patients with DM2: Periodontal disease may increase the cytokine levels in diabetic patients and thereby contribute to systemic inflammation, whereas diabetes produces hyper-inflammatory reactions that may increase the risk of periodontal disease among patients with DM2 [50]. This seems to be very important for overweight DM2 patients with periodontal disease who already have an increased risk of systemic inflammation: These three health conditions (obesity, periodontal disease and DM2) are linked by the pro-inflammatory cytokines which appear to induce inflammation [12]. In light of all these, the link between tooth loss, OSA and BMI, in terms of correlation and clustering, may imply that tooth loss, in particular in the maxilla, seems to be an important predisposing factor either by leading to anatomical changes or signalling active periodontal infection. The correlation between maxillary tooth loss and HbA1c and fasting blood glucose may imply some underlying pathogenic or biologic mechanisms between OSA, tooth loss and DM2. This may have important public health implications and lead to improved health and oral health among DM2 patients. Daily toothbrushing may act as a preventive health behaviour in the prevention of OSA by reducing gingival inflammation, considering the correlation of OSA with toothbrushing and gingival bleeding in the present study. There is a vital need for further research to understand better the relationship between OSA, tooth loss, diabetes and obesity as this is the first study exploring this relation, as far as we know.
Self-reported toothbrushing frequencies and gingival bleeding may sometimes be imprecise. Reporting may be affected by the perceived social desirability of these behaviours in families and society, but there is evidence endorsing the reliability of self-reported behaviour measures like toothbrushing frequency [51, 52] and gingival bleeding [52, 53].
The limitation of this study is that it does not refer to a clinical intervention. There seems to be a need for clinical studies exploring the biological markers for tooth loss, OSA, diabetes and obesity. Follow-up studies on the impact of periodontal treatment (which reduces subsequent tooth loss) on OSA, diabetes and obesity are also needed to identify risk factors and improve the well-being of DM2 patients. Furthermore, the present study, based on a limited number of participants, should be replicated with a larger sample. The background characteristics of the participants are relevant to the results and may have an impact on the correlations found, but the focus of the present study was to explore the relationship between oral health, diabetes type two and sleep apnea among diabetics regardless of the background characteristics. There is need for further studies to examine the impact of these characteristics.
Conclusion
Based on the correlations found between oral health (clinical and self-assessed) and diabetes-related variables, dental care may play a major role in the prevention of further complications of DM2 by enabling early diagnosis and monitoring of poor diabetes management. This requires further study. The findings of this study have a number of implications for future practice: Observation of frequent gingival bleeding and subsequent tooth loss may lead patients to consider the risk of sleep apnea and to have appropriate clinical examinations early. Dentists may also play a key role in better managing and diagnosing sleep apnea early by referring patients with severe tooth loss and periodontal disease for general medical examination. It could be relevant for physicians to be prepared to educate their DM2 patients on managing their oral and general health to prevent possible further complications. There seems a need for public health programmes, training programmes and campaigns to increase awareness among healthcare professionals and patients about the relationships between oral health, diabetes and sleep apnea. Future research on these factors is essential to counter the pandemic of DM2 complications and poor oral health.
References
WHO (2005) Preventing chronic diseases: a vital investment. Geneva. http://www.who.int/chp/chronic_disease_report/contents/en/index.html. Accessed February 2012
Petersen PE (2003) The World Oral Health Report 2003: continuous improvement of oral health in the 21st century—the approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol 31(Suppl 1):3–23
WHO (2010) Global strategy on diet, physical activity and health: facts related to chronic diseases. http://www.who.int/dietphysicalactivity/publications/facts/chronic/en/index.html. Accessed February 2012
Australian Government, Australian Institute of Health and Welfare (2007) Chronic diseases. http://www.aihw.gov.au/cdarf/diseases_pages/index.cfm. Accessed February 2012
Marshall TA, Eichenberger-Gilmore JM, Broffitt BA et al (2007) Dental caries and childhood obesity: roles of diet and socio-economic status. Community Dent Oral Epidemiol 35:449–458
Alm A, Fahreus C, Wendt LK et al (2008) Body adiposity status in teenagers and snacking habits in early childhood in relation to proximal caries at 15 years of age. Int J Paediatr Dent 18:189–196
WHO (2003) Diet nutrition and the prevention of chronic diseases. Report of the joint WHO/FAO Expert Consultation, WHO Technical Report Series, No. 916 (TRS 916). WHO, Geneva
Cinar AB, Murtomaa H (2008) Clustering of obesity and dental health with life-style factors among Turkish and Finnish pre-adolescents. Obes Facts 1:196–202
Cinar AB, Murtomaa H (2010) Interrelation between obesity, oral health and life-style factors among Turkish school children. Clin Oral Investig 15:177–184
Pischon N, Heng N, Bernimoulin JP et al (2007) Obesity, inflammation, and periodontal disease. J Dent Res 86:400–409
Al-Zahrani MS, Bissada NF, Borawskit EA (2003) Obesity and periodontal disease in young, middle-aged, and older adults. J Periodontol 74:610–615
Genco RJ, Grossi SG, Ho A et al (2005) A proposed model linking inflammation to obesity, diabetes, and periodontal infections. J Periodontol 76(11 Suppl):2075–2084
Lundin M, Yucel-Lindberg T, Dahllöf G et al (2004) Correlation between TNFalpha in gingival crevicular fluid and body mass index in obese subjects. Acta Odontol Scand 62:273–277
Nishimura F, Soga Y, Iwamoto Y et al (2005) Periodontal disease as part of the insulin resistance syndrome in diabetic patients. J Int Acad Periodontol 7:16–20
Nishimura F, Kono T, Fujimoto C et al (2000) Negative effects of chronic inflammatory periodontal disease on diabetes mellitus. J Int Acad Periodontol 2:49–55
Campus G, Salem A, Uzzau S, Baldoni E, Tonolo G (2005) Diabetes and periodontal disease: a case–control study. J Periodontol 76:418–425
Khader YS, Rice JC, Lefante JJ (2003) Factors associated with periodontal diseases in a dental teaching clinic population in northern Jordan. J Periodontol 74:1610–1617
Furukawa T, Wakai K, Yamanouchi K, Oshida Y, Miyao M, Watanabe T, Sato Y (2007) Associations of periodontal damage and tooth loss with atherogenic factors among patients with type 2 diabetes mellitus. Intern Med 46:1359–1364
Ostberg AL, Nyholm M, Gullberg B, Råstam L, Lindblad U (2009) Tooth loss and obesity in a defined Swedish population. Scand J Public Health 37:427–433
Hilgert JB, Hugo FN, de Sousa ML, Bozzetti MC (2009) Oral status and its association with obesity in southern Brazilian older people. Gerodontology 26:46–52
Botros N, Concato J, Mohsenin V, Selim B, Doctor K, Yaggi HK (2009) Obstructive sleep apnea as a risk factor for type 2 diabetes. Am J Med 122:1122–1127
Shah N, Roux F (2009) The relationship of obesity and obstructive sleep apnea. Clin Chest Med 30:455–465
Lam DC, Lui MM, Lam JC, Ong LH, Lam KS, Ip MS (2010) Prevalence and recognition of obstructive sleep apnea in Chinese patients with type 2 diabetes mellitus. Chest 138:1101–1107
Bucca C, Cicolin A, Brussino L, Arienti A, Graziano A, Erovigni F, Pera P, Gai V, Mutani R, Preti G, Rolla G, Carossa S (2006) Tooth loss and obstructive sleep apnoea. Respir Res 17:7–8
Baguley TS (2004) Understanding statistical power in the context of applied research. Appl Ergon 35:73–80
Polonsky WH, Anderson BJ, Lohrer PA, Welch G, Jacobson AM, Aponte JE, Schwartz CE (1995) Assessment of diabetes-related distress. Diabetes Care 18:754–776
WHO (2004) WHO Quality of Life-BREF (WHOQOL-BREF). http://www.who.int/substance_abuse/research_tools/whoqolbref/en/index.html. Accessed February 2012
ICDAS (International Caries Assessment and Detection System) http://icdas.smile-on.com/. Accessed February 2012
WHO (1997) Oral health survey: basic methods, 4th edn. WHO, Geneva
International Diabetes Federation Clinical Guidelines Task Force (2005) Global guideline for type 2 diabetes, chapter 6: Glucose control levels and chapter 12: Cardiovascular risk protection
WHO (2012) BMI classification. http://apps.who.int/bmi/index.jsp?introPage=intro_3.html:bmi Accessed February 2012
Tuomilehto H (2008) Sleep duration is associated with an increased risk for the prevalence of type 2 diabetes in middle-aged women—the FIN-D2D Survey. Sleep Med 9:221–227
Partinen M (1982) Sleeping habits and sleep disorders on Finnish men before, during and after military service. Ann Med Milit Fenn 57(Suppl 1):1–96
Mealey BL, Ocampo GL (2007) Diabetes mellitus and periodontal disease. Periodontology 2000 44:127–153
Tsai C, Hayes C, Taylor GW (2002) Glycemic control of type 2 diabetes and severe periodontal disease in the US adult population. Community Dent Oral Epidemiol 30:182–192
Löe H (2000) Oral hygiene in the prevention of caries and periodontal disease. Int Dent J50:129–139
Fujita M, Ueno K, Hata A (2009) Lower frequency of daily teeth brushing is related to high prevalence of cardiovascular risk factors. Exp Biol Med (Maywood) 234:387–394
Syrjala A-MH, Ylostalo P, Niskanen MC, Knuuttila MLE (2004) Relation of different measures of psychological characteristics to oral health habits, diabetes adherence and related clinical variables among diabetic patients. Eur J Oral Sci 112:109–114
Löe H (2000) Oral hygiene in the prevention of caries and periodontal disease. Int Dent J 50:129–139
Katz J, Chaushu G, Sharabi Y (2001) On the association between hypercholesterolemia, cardiovascular disease and severe periodontal disease. J Clin Periodontol 28:865–868
Katz J, Flugelman MY, Goldberg A et al (2002) Association between periodontal pockets and elevated cholesterol and low density lipoprotein cholesterol levels. J Periodontol 73:494–500
Choi YH, McKeown RE, Mayer-Davis EJ, Liese AD, Song KB, Merchant AT (2011) Association between periodontitis and impaired fasting glucose and diabetes. Diabetes Care 34:381–386
Zadik Y, Bechor R, Galor S, Levin L (2010) Periodontal disease might be associated even with impaired fasting glucose. Br Dent J 208:E20
Young T, Shahar E, Nieto FJ et al (2002) Predictors of sleep disordered breathing in community-dwelling adults: the Sleep Heart Health Study. Arch Intern Med 162:893–900
Ivanhoe JR, Cibirka RM, Lefebvre CA, Parr GR (1999) Dental considerations in upper airway disorders: a review of the literature. J Prosthet Dent 82:685–698
Tasali E, Mokhlesi B, Van Cauter E (2008) Obstructive sleep apnea and type 2 diabetes: interacting epidemics. Chest 133:496–506
Foster GD, Sanders MH, Millman R, Zammit G, Borradaile KE, Newman AB, Wadden TA, Kelley D, Wing RR, Sunyer FX, Darcey V, Kuna ST, Sleep AHEAD Research Group (2009) Obstructive sleep apnea among obese patients with type 2 diabetes. Diabetes Care 32:1017–1019
Tasali E, Ip MS (2008) Obstructive sleep apnea and metabolic syndrome: alterations in glucose metabolism and inflammation. Proc Am Thorac Soc 15:207–217
Meier-Ewert HK, Ridker PM, Rifai N, Regan MM, Price NJ, Dinges DF, Mullington JM (2004) Effect of sleep loss on C-reactive protein, an inflammatory marker of cardiovascular risk. J Am Coll Cardiol 43:678–683
Bascones-Martinez A, Matesanz-Perez P, Escribano-Bermejo M, González-Moles MÁ, Bascones-Ilundain J, Meurman JH (2011) Periodontal disease and diabetes—review of the literature. Med Oral Patol Oral Cir Bucal 1(6):e722–e729
Pine CM, Adair PM, Nicoll AD, Burnside G, Petersen PE, Beighton D et al (2004) International comparisons of health inequalities in childhood dental caries. Community Dent Health 21(1 Suppl):121–130
Cinar AB (2008) Preadolescents and their mothers as oral health-promoting actors: non-biologic determinants of oral health among Turkish and Finnish preadolescents. Thesis for Doctorate in Dentistry, University of Helsinki, Institute of Dentistry, Oral Public Health Department, November
Kallio P, Murtomaa H (1997) Determinants of self-assessed gingival health among adolescents. Acta Odontol Scand 55(2):106–110
Acknowledgments
We express our deepest thanks to Prof. Nazif Bagriacik (Head, Turkish Diabetes Association), Associate Prof. Mehmet Sargin and Head Diabetes Nurse Sengul Isik (Diabetes Unit, S.B. Kartal Research and Education Hospital) for all their support and help during the research. We thank Prof. Aytekin Oguz for his help on the preparation of the documents for ethical permission. We also thank to periodontologist Duygu İlhan for clinical periodontal examinations during the first phase of the study. We also would like to thank ZENDIUM for oral healthcare kits, SPLENDA (TR) for the promotional tools, ChiBall World Pty Ltd. for exercising chi-balls and IVOCLAR Vivadent, Plandent, Denmark, for help in the provision of CRT kits. Many thanks are due to our patients for their participation and cooperation. The research project is supported by FDI and the International Research Fund of the University of Copenhagen.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cinar, A.B., Oktay, I. & Schou, L. Relationship between oral health, diabetes management and sleep apnea. Clin Oral Invest 17, 967–974 (2013). https://doi.org/10.1007/s00784-012-0760-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-012-0760-y