Abstract
A pulpotomy is the therapy for management of pulp exposures due to caries in symptom-free primary molars. The aim was to longitudinally compare the relative effectiveness of the Er:YAG laser, calcium hydroxide and ferric sulphate techniques with dilute formocresol in retaining symptom-free molars. Two hundred primary molars in 107 healthy children were included and randomly allocated to one technique. The treated teeth were blindly reevaluated after 6, 12, 18, 24 and 36 months. Descriptive data analysis and logistic regression analysis accounting for multiple observations per patient by generalised estimating equation were used. Additionally, various influences including tooth type, upper and lower jaws, type of anaesthesia, operator and the final restoration on treatment success were evaluated (Wald chi-square test). After 36 months, the following total (considering clinical and clinically symptom-free radiographic failures) and clinical success rates were determined (in percent): Formocresol 72 (92), laser 73 (89), calcium hydroxide 46 (75), ferric sulphate 76 (97). No significant differences were detected between formocresol and any other technique after 36 months. However, the odds ratio of failure appeared to be three times higher for calcium hydroxide than for formocresol. No significant differences in total success rates were seen regarding the aforementioned influencing clinical parameters. The correct diagnosis of the pulpal status, bleeding control and the specific technique are highly important for long-term success of pulpotomies in primary molars. According to the presented long-term data, pulpotomies using ferric sulphate revealed the best treatment outcome among the used techniques, while calcium hydroxide resulted in the lowest success rates after 3 years. Therefore, we can recommend ferric sulphate for easy and successful treatment of primary molars with caries-exposed pulps.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A pulpotomy is the common therapy for caries-exposed pulps in symptom-free primary molars; the purpose of a pulpotomy is to preserve the radicular pulp, avoid pain and swelling and ultimately retain the tooth for arch integrity [1, 2]. Although many techniques have been suggested, long-term studies, which ideally cover the functional lifetime of primary molars, are required to provide evidence of the most appropriate pulpotomy procedure [3, 4].
Dilute formocresol used to be the “gold standard” for pulpotomies. However, due to reports of cytotoxicity and potential mutagenicity (especially in children) [5–7], it has recently been replaced by alternative methods. The Erbium: Yttrium-Aluminum Garnet (Er:YAG) laser, with only slight thermal alteration to the pulpal tissue, has been suggested as an alternative due to its haemostatic, antimicrobial and cell-stimulating properties [8–11]. Besides this study, the data regarding the clinical use of lasers for pulpotomies in human teeth [10, 12, 13] are too small to draw conclusions about their effectiveness. Calcium hydroxide has been used widely, especially in Scandinavian countries; however, problems with internal resorption and less long-term success were reported [2, 14]. Ferric sulphate has been increasingly used due to its haemostatic effect, ease of use and good long-term success [1].
Following a correct diagnosis and appropriate pulpotomy technique, high emphasis has been placed on the final restoration, which seals the tooth from microleakage [2]. The final restoration is either provided by stainless steel crowns or composite resins depending on the substance defect.
This study aimed to determine the relative effectiveness of the Er:YAG laser, calcium hydroxide and ferric sulphate in comparison to dilute formocresol over 3 years and is reported according to the CONSORT statement [15]. The influence of several clinical parameters (tooth type, type of anaesthesia, upper and lower jaws, operator, type of final restoration and restoration failure) on pulpotomy success was also investigated.
Materials and methods
Participants
Participants were healthy children; they were not older than 8 years of age with at least one symptom-free, restorable primary molar with a caries-exposed vital pulp. Clinical exclusion criteria included spontaneous pain, swelling, tenderness to percussion, pathological mobility and initial, unsuccessful haemorrhage control. Teeth with pre-operative radiographic pathology, such as resorption, periradicular or furcal radiolucency, a widened periodontal ligament space or physiological root resorption involving more than one third of the root, were excluded. Children attending the Pedodontic Section, Department of Restorative Dentistry and Periodontology, University of Munich, that met the criteria were enrolled. After ethical approval (No. 281/99) and informed parental consent, the pulpotomies were performed by two pedodontists under local anaesthesia or general anaesthesia without the additional use of local anaesthetics.
Interventions
Dilute formocresol (1:5 Buckley's solution), Er:YAG laser, calcium hydroxide and ferric sulphate (15.5%) were used as parallel intervention methods. In all groups, after rubber dam isolation and caries removal, the pulp chamber was opened with a sterile high-speed diamond bur, and the coronal pulp was removed by a sterile slow-speed round bur (#830RL016, #H1SE.204021, Brasseler, Lemgo, Germany) under continuous water irrigation. Complete removal of the coronal pulp tissue was performed via visual examination and by using a sterile hand excavator in the undercut areas. Haemorrhage control was achieved by placing sterile, saline-wetted cotton wool pellets on the radicular pulp stumps under slight pressure [16] and waiting 5 min for primary haemostasis [17]. Subsequently, blood clot remnants were removed, and the cavity was dried. An inclusion criterion included the achievement of complete haemostasis at this stage, i.e., before one of the four techniques was applied. When bleeding recommenced during placement of the medication or laser irradiation, the tooth was excluded from further follow-up.
In the control group, formocresol-moistened pellets were placed on the pulp stumps for 5 min. Er:YAG laser radiation (wavelength 2.94 μm) was delivered with a special handpiece (KEY Laser 1242; handpiece 2051, KaVo, Biberach, Germany) to the canal orifices; the parameters were set at 2 Hz and 180 mJ per pulse without water cooling [18]. The mean number of laser pulses per tooth was 31.5 ± 5.9, and they were equally distributed to each pulp stump. In the calcium hydroxide group, the canal orifices were dressed with aqueous calcium hydroxide (Calxyl®, OCO Präparate GmbH, Dirmstein, Germany), slightly dampened and covered with a calcium hydroxide cement (Kerr® Life, Kerr GmbH, Karlsruhe, Germany). Ferric sulphate-wetted pellets (Astringedent®, Ultradent Products Inc., Salt Lake City, UT, USA) were placed on the pulp stumps for 15 s.
A reinforced zinc oxide eugenol base (IRM®, Dentsply DeTrey, Konstanz, Germany) was then applied to the cavity floor followed by a glass ionomer cement (Ketac™ Bond, 3MESPE, Seefeld, Germany) and stainless steel crown (SSC, 3MESPE) or composite resin restoration (CRR, Tetric® Ceram, Ivoclar Vivadent, Schaan, Liechtenstein).
Follow-up
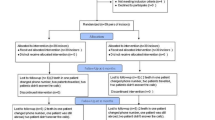
Clinical re-evaluations were performed at 6, 12, 18, 24 and 36 months ± 2 weeks, and radiographic examinations were performed at 12, 24 and 36 months. These examinations were performed independently by two experienced dentists (not the operators) who were blinded to the technique at any recall examination; forced consensus was made in cases of disagreement. The inter- and intra-examiner reproducibility was calculated by Cohen's unweighted kappa statistic [19]. The flow of participants and pulpotomies were followed from allocation to final data analysis after 36 months (Fig. 1).
Hypothesis and outcomes
Hypothesising that no difference in effectiveness exists between dilute formocresol and the three other techniques, the primary endpoint was a clinically and radiographically symptom-free tooth at 12, 24 and 36 months ± 2 weeks. Clinical failure parameters included spontaneous pain, tenderness to percussion, fistula, soft tissue swelling and pathological tooth mobility. Radiographic failure parameters included periapical or furcal radiolucency, pathologic external or distinct internal root resorption or widened periodontal ligament space. The restoration performance (partially or completely lost fillings, secondary caries at the margin, perforated or lost SSC crowns or severe gingival inflammation) was determined as a secondary outcome.
Sample size calculation
The sample size calculation (PS Power and Sample Size Calculation Program, Version 2.1.31) [20] was based on an internal pilot study comparing the success rates of calcium hydroxide (55.9%) and formocresol (90.1%) [21], as well as on a study comparing ferric sulphate (96.55%) and formocresol (77.78%) [22]. The first outcome difference led to a required sample size of 28 to detect a significant difference (80% power, two-sided 5% significance level), and the study comparing ferric sulphate and formocresol led to a required sample size of 50 per intervention group. For the Er:YAG laser group, no previous data for sample size calculation was available. Therefore, a sample size of 50 in each intervention group was planned.
Randomisation and blinding
Each tooth was randomly allocated to one of the four techniques by an assistant casting a concealed lot out of a box containing 4 × 50 lots (block randomisation) [19]. The allocation to the different techniques was not stratified by age. All other contributors to the study were blinded to generation and implementation of the treatment assignment. The outcome assessment and data analysis were blinded as the techniques were undistinguishable and coded.
Statistical methods
During follow-up, a clinical failure was recorded if the pulpotomy failed due to clinical symptoms and showed pathology on the radiograph. Those with radiographic changes but without clinical symptoms were recorded separately. The total failure rate included the clinical failures and those radiographic failures that were clinically symptom-free.
The 12-, 24- and 36-month total and clinical success and failure rates of each pulpotomy technique were calculated, considering previous and new failures at the time of recall in proportion to the number of previous failures plus the currently recalled pulpotomies. Additionally, the total success and failure rates for several parameters (type of anaesthesia, two operators, tooth type, upper and lower jaws, final restoration) were calculated across all techniques:
Multiplicity and therefore dependence of more than one pulpotomy within a patient was accounted for within the statistical analysis by using a generalised estimating equation (GEE) [23]. An exchangeable correlation structure was used because the correlation between any two pulpotomies was assumed to be the same across patients. A binary logistic GEE model was used to analyse the differences in effectiveness between formocresol and each of the other procedures (α-level = 0.05) [19], which is also given as an odds ratio with 95% confidence interval (OR ± 95% CI). The Wald chi-square test was applied to test the differences in overall effectiveness regarding the aforementioned parameters. All tests were performed using a 0.05 level of significance. All analyses were done using PASW 18.0.2 (SPSS Inc., Chicago, IL, USA).
Results
In total, 200 primary molars within 107 patients were allocated to the four techniques. Three teeth of the laser group and six of the calcium hydroxide group were excluded from follow-up and statistical analysis due to uncontrollable bleeding during radiation or placement of calcium hydroxide; a hyperaemic, inflamed radicular pulp is considered to be a contraindication for vital pulpotomy [1]. Thus, 191 pulpotomised teeth (Table 1) in 103 patients (56 males, 47 females; mean age 4.8 ± 1.6 years, range 2–8 years) were re-evaluated. After 36 months, 47 teeth had exfoliated physiologically, and 8 were lost to follow-up (due to patients moving away) leaving 136 pulpotomies within 77 patients for the intention-to-treat statistical analysis (Fig. 1).
The clinical and radiographic inter-examiner reproducibility at the 36-month recall was optimal (Cohen's κ = 1, κ = 0.76), and the intra-examiner reproducibility was optimal for both (Cohen's κ = 1).
The clinical and radiographic evaluation after 12 months [24] revealed the following total and clinical (placed parenthetically) success rates for the different methods (%): Formocresol 96 (100), laser 93 (98), calcium hydroxide 86 (95) and ferric sulphate 86 (100). There was no significant difference in effectiveness between formocresol and any of the other techniques after 12 months (p > 0.05) (Table 2).
After 24 months, the differences in total and clinical success rates between the techniques became more distinct (in percent) [24]: formocresol 85 (96), laser 78 (93), calcium hydroxide 53 (87) and ferric sulphate 86 (100). However, compared to formocresol, only calcium hydroxide performed significantly worse (p = 0.001); the odds of failure were 5.6 (95% CI 2.0–15.5) times higher than the odds for the formocresol method. Although not significant, the laser group had an odds ratio of 1.7 compared to the formocresol group (95% CI 0.6–5.2), and ferric sulphate had an odds ratio of 0.96 compared to the formocresol group (95% CI 0.3–3.0) (Table 2).
After 36 months, the differences in total and clinical success rates between the techniques were as follows (in percent): formocresol 72 (92), laser 73 (89), calcium hydroxide 46 (75) and ferric sulphate 76 (97). Although there was no longer a significant difference in effectiveness between formocresol and any of the other techniques after 36 months (p > 0.05), the odds of failure for calcium hydroxide were three times higher (95% CI 0.9–9.5) than for the formocresol method (Table 2). This was reflected by a p value of 0.07.
Eleven clinical failures and 34 radiographic failures without clinical symptoms were found within the 36 months (Table 3).
Within 36 months, no differences in overall total success rates (%) between pulpotomies performed under local or general anaesthesia (65/66), by operator 1 or 2 (72/61), in first or second primary molars (60/73), in the maxilla or mandible (72/64) and with SSC or CRR as a final restoration (66/68) were found (p > 0.05).
Over 3 years, 3 out of 109 SSC were lost but had an intact cement base; however, there was one pulpotomy failure (formocresol). Of the 82 CRR, 18 fillings were unacceptable (4 totally lost, 3 partially lost, 11 showed secondary caries) with seven pulpotomy failures (two formocresol, one laser, two calcium hydroxide, two ferric sulphate). Although restoration failure did not significantly influence the success or failure of the pulpotomy (p = 0.08), the odds, however, of pulpotomy failure in the case of a restoration failure was 3.7 times higher (95% CI 0.9–15.5) than in the case of an intact restoration.
No adverse events or side effects were recognised during the study.
Discussion
Although calcium hydroxide performed significantly worse than formocresol after 24 months [24], the difference was no longer significant after 36 months (p = 0.07), which may have been due to the number of exfoliations throughout the study resulting in a decreased sample size. However, the risk of failure was three times higher when using calcium hydroxide than when using dilute formocresol. The total failure rate of 54% after 3 years is comparable to other recently published studies, especially when taking the shorter follow-up periods into account (1 or 2 years). Total failure rates as high as 64% after 2 years have been reported [25], 44% after 1 year when using light-cured calcium hydroxide [26], 54% after 2 years [27], 67% after 1 year when the pulpotomies were performed by dental students [28] and 20% and 40% after 1 year for teeth either restored with stainless steel crowns or amalgam, respectively [39]. Earlier studies reported lower total failure rates such as 23% after a mean clinical review of 22 months and a mean radiographic review of 19 months [29]. Distinct internal areas of resorption were the cause of radiographic failure in 4 out of 13 cases within the 36 months (Table 3); those results were not higher in percentage than in the other groups (FC 2/6, L 3/6, FS 2/9). In contrast, several other studies reported evidence of internal resorption as the main failure mode for calcium hydroxide pulpotomies [14, 25].
The Er:YAG laser pulpotomies had a comparable total failure rate (27%) to formocresol (28%) after 3 years. Therefore, the tendency for inferior effectiveness at the 24-month recall was not continued. The selected parameters (2 Hz and 180 mJ per pulse) had been based on the only available animal study at that time [18]. A later study suggested lower energy levels per pulse for the Er:YAG laser [10]. The study investigated the effect of three different energy levels (34, 68 and 102 mJ per pulse) on the pulp tissue of rat molars during pulpotomy histopathologically after 1 week; the results showed a higher degree of inflammation signs with increasing energy levels. A clinical study using the Nd:YAG laser for pulpotomies reported total failure rates of 29% after 1 year and no significant difference between the use of the laser and dilute formocresol [13]. A surprisingly low total failure rate of 5.9% after 6–64 months for Nd:YAG laser pulpotomies in human primary molars has been reported in a study from Taiwan [12]. Nevertheless, for a dentist who does not use lasers routinely, this method might be rather complicated to handle when compared to the application of solutions like formocresol or ferric sulphate.
While no significant superiority of ferric sulphate, when compared to dilute formocresol, was assured after 3 years, this method revealed the best absolute outcomes with a clinical failure rate of only 3% (one clinical failure) and a total failure rate of 24% from nine failures seen radiographically after 3 years. A meta-analysis of 11 studies comparing formocresol and ferric sulphate supported our findings of mean clinical and radiographic success rates of 92% ± 8% and 73% ± 18%, respectively, for ferric sulphate. Significant differences involving formocresol were not shown [30]. A literature review from the year 2006 evaluating 48 clinical trials also found similar clinical/radiographic results for formocresol and ferric sulphate [3]. The distinct difference between the clinical and radiographic success rates for ferric sulphate pulpotomies was pointed out earlier [31]; this difference emphasises the importance of regular radiographic monitoring.
Remarkably, 18 out of 82 composite resin restorations failed, but only 3 out of 109 stainless steel crowns failed. Although restoration failure did not significantly influence the success of the pulpotomy (p = 0.08), the risk, however, of pulpotomy failure in the cases of restoration failure was 3.7 (95% CI 0.8–15.5) times higher than in cases of intact restorations. Earlier reports have shown that restoring pulpotomised primary molars with resin-based materials or amalgam is inferior to the reported success rates when using stainless steel crowns; however, restoration failure did not influence treatment prognosis significantly [32, 33].
Initially, haemostasis was achieved in all 200 teeth. Though, three teeth allocated to the laser and six to the calcium hydroxide group had to be excluded from follow-up due to uncontrollable bleeding, which recommenced during irradiation or placement of calcium hydroxide. This indicated a hyperaemic, inflamed radicular pulp. The various mechanisms of bleeding control via the applied techniques in this study are therefore interesting: First, non-medicated cotton pellets and waiting for primary haemostasis; second, formocresol fixes tissue in the coronal third of the radicular pulp and causes haemostasis by vessel thrombosis and impaired microcirculation [16]; third, in case of the Er:YAG laser, the pulp's microcirculation after irradiation has been reported to be instantly and reversibly decreased for 3–6 min [18]. No hyperaemic reactions that might have been caused by heat were reported. Fourthly, calcium hydroxide has been shown to create superficial necrosis which inhibits bleeding and fluid loss [29]. Last but not least, ferric sulphate precipitates protein plugs which occlude the capillaries resulting in haemostasis [34]. The plugs are caused by the reaction of blood with ferric and sulphate ions. Nonetheless, it might be assumed that the status of the pulp is more critical for pulpotomy success when using calcium hydroxide and the Er:YAG laser than when using formocresol or ferric sulphate.
This study presents important long-term data (36 months) in continuation of the previously published 12 and 24 months data [24] involving the different pulpotomy techniques and new data concerning the controlled use of the Er:YAG laser for pulpotomies. The external validity of this study is limited due to the pulpotomies being performed by specialists in a hospital where most patients present following a referral for special options such as general anaesthesia. There are now new methods, such as mineral trioxide aggregate, that promise even higher success rates than those reported in this study [2].
In conclusion, after 36 months, calcium hydroxide was the least effective pulpotomy technique, and ferric sulphate was the most effective; the differences with formocresol use were not shown to be significant. The Er:YAG laser showed the same level of effectiveness as formocresol.
References
Fuks AB (2008) Vital pulp therapy with new materials for primary teeth: new directions and treatment perspectives. Pediatr Dent 30:211–219
AAPD Clinical Affairs Committee of the American Academy Pediatric Dentistry - Pulp Therapy Subcommittee: Guideline on pulp therapy for primary and immature permanent teeth. Reference Manual 2010–2011;V32/No 6:194–201
Fuks AB, Papagiannoulis L (2006) Pulpotomy in primary teeth: review of the literature according to standardized criteria. Eur Arch Paediatr Dent 7:64–71, discussion 72
Nadin G, Goel BR, Yeung CA, Glenny AM (2008) Pulp treatment for extensive decay in primary teeth. In: The Cochrane Library Issue 4
Zarzar PA, Rosenblatt A, Takahashi CS, Takeuchi PL, Costa Junior LA (2003) Formocresol mutagenicity following primary tooth pulp therapy: an in vivo study. J Dent 31:479–485
Patchett CL, Srinivasan V, Waterhouse PJ (2006) Is there life after Buckley's formocresol? Part II—development of a protocol for the management of extensive caries in the primary molar. Int J Paediatr Dent 16:199–206
IARC International Agency for Research on Cancer (2006) Formaldehyde, 2-butoxyethanol and 1-tert-butoxypropan-2-ol. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans 88
Matsumoto K (2000) Lasers in endodontics. Dent Clin North Am 44:889–906
Schoop U, Moritz A, Kluger W, Patruta S, Goharkhay K, Sperr W, Wernisch J, Gattringer R, Mrass P, Georgopoulos A (2002) The Er:YAG laser in endodontics: results of an in vitro study. Lasers Surg Med 30:360–364
Kimura Y, Yonaga K, Yokoyama K, Watanabe H, Wang X, Matsumoto K (2003) Histopathological changes in dental pulp irradiated by Er:YAG laser: a preliminary report on laser pulpotomy. J Clin Laser Med Surg 21:345–350
Jayawardena JA, Kato J, Moriya K, Takagi Y (2001) Pulpal response to exposure with Er:YAG laser. Oral Surg Oral Med Oral Pathol Radiol Endod 91:222–229
Liu JF (2006) Effects of Nd:YAG laser pulpotomy on human primary molars. J Endod 32:404–407
Odabas ME, Bodur H, Baris E, Demir C (2007) Clinical, radiographic, and histopathologic evaluation of Nd:YAG laser pulpotomy on human primary teeth. J Endod 33:415–421
Sonmez D, Duruturk L (2008) Ca(OH)2 pulpotomy in primary teeth. Part I: internal resorption as a complication following pulpotomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 106:94–98
Moher D, Schulz KF, Altman DG (2001) The CONSORT Statement: revised recommendations for improving the quality of reports of parallel-group randomized trials. Ann Int Med 134:657–662
Thompson KS, Seale NS, Nunn ME, Huff G (2001) Alternative method of haemorrhage control in full strength formocresol pulpotomy. Pediatr Dent 23:217–222
Mielke CH, Kaneshiro MM, Maher IA, Weiner JM, Rapaport SI (1969) The standardized normal Ivy bleeding time and its prolongation by aspirin. Blood 34:204–215
Keller U, Hibst R (1991) Tooth pulp reaction following Er:YAG laser application. Proceedings of Lasers in Orthopedic, Dental, and Veterinary Medicine, Jan 23–24, Los Angeles, California. O'Brien SJ, Dederich DN, Wigdor H, Trent A, editors. Proc SPIE 1424:127–133
Altman DG (1991) Practical statistics for medical research. Chapman & Hall, London
Dupont WD, Plummer WD (1990) Power and sample size calculations: a review and computer program. Control Clin Trials 11:116–128
Benz C, Reeka A, Stroinj A, Hickel R (1998) Comparison of two pulpotomy techniques in deciduous dentition: a clinical study. Ital J Paediatr Dent 1:38–39
Fei AL, Udin R, Johnson R (1991) A clinical study of ferric sulfate as a pulpotomy agent in primary teeth. Pediatr Dent 13:327–331
Liang K-Y, Zeger S (1986) Longitudinal data analysis using generalized linear models. Biometrika 73:13–22
Huth KC, Paschos E, Hajek-Al-Khatar N, Hollweck R, Crispin A, Hickel R, Folwaczny M (2005) Effectiveness of 4 pulpotomy techniques—randomized controlled trial. J Dent Res 84:1144–1148
Moretti AB, Sakai VT, Oliveira TM, Fornetti AP, Santos CF, Machado MA, Abdo RC (2008) The effectiveness of mineral trioxide aggregate, calcium hydroxide and formocresol for pulpotomies in primary teeth. Int Endod J 41:547–555
Zurn D, Seale NS (2008) Light-cured calcium hydroxide vs formocresol in human primary molar pulpotomies: a randomized controlled trial. Pediatr Dent 30:34–41
Sonmez D, Sari S, Cetinbas T (2008) A comparison of four pulpotomy techniques in primary molars: a long-term follow-up. J Endod 34:950–955
Alacam A, Odabas ME, Tuzuner T, Sillelioglu H, Baygin O (2009) Clinical and radiographic outcomes of calcium hydroxide and formocresol pulpotomies performed by dental students. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 108:127–133
Waterhouse PJ, Nunn JH, Whitworth JM (2000) An investigation of the relative efficacy of Buckley's formocresol and calcium hydroxide in primary molar vital pulp therapy. Br Dent J 188:32–36
Peng L, Ye L, Guo X, Tan H, Zhou X, Wang C, Li R (2007) Evaluation of formocresol versus ferric sulphate primary molar pulpotomy: a systematic review and meta-analysis. Int Endod J 40:751–757
Casas MJ, Layug MA, Kenny DJ, Johnston DH, Judd PL (2003) Two-year outcomes of primary molar ferric sulphate pulpotomy and root canal therapy. Pediatr Dent 25:97–102
Sonmez D, Duruturk L (2010) Success rate of calcium hydroxide pulpotomy in primary molars restored with amalgam and stainless steel crowns. Br Dent J 208:E18, discussion 408–409
Guelmann M, McIlwain MF, Primosch RE (2005) Radiographic assessment of primary molar pulpotomies restored with resin-based materials. Pediatr Dent 27:24–27
Lemon RR, Steele PJ, Jeansonne BG (1993) Ferric sulphate hemostasis: effect on osseous wound healing. Left in situ for maximum exposure. J Endod 19:170–173
Acknowledgements
The authors would like to express their gratitude towards Željka Maruniza, Kathrin Braunmüller, Kerstin Weidlich and Prof. Dr. Dr. Matthias Folwaczny for their participation in this clinical study and valuable discussion. The study was completely financed by departmental funding.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 75 kb)
Rights and permissions
About this article
Cite this article
Huth, K.C., Hajek-Al-Khatar, N., Wolf, P. et al. Long-term effectiveness of four pulpotomy techniques: 3-year randomised controlled trial. Clin Oral Invest 16, 1243–1250 (2012). https://doi.org/10.1007/s00784-011-0602-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-011-0602-3