Abstract
This study measured the accuracy and precision of four commercial dental radiometers. The intra-brand accuracy was also determined. The light outputs from 14 different curing lights were measured three times using four brands of dental radiometers and the results were compared to two laboratory-grade power meters that were used as the “gold standard”. To ensure proper representation, three examples of each brand of dental radiometer were used. Data collected was analyzed using ANOVA, with 95% confidence intervals, comparing the laboratory-grade meters to the dental radiometers. Bioequivalence was established where the confidence interval for the irradiance values was within ±20% of the “gold standard” reading. Forest plots were used to highlight bioequivalence values. The two laboratory-grade meters differed by less than 0.6%. Overall, all three examples of the Bluephase and SDI radiometers as well as two examples of the LEDRadiometer and one CureRite meter were bioequivalent to the gold standard. However, the type of curing light measured had a significant effect on the accuracy of the radiometer. There was significant variability of the irradiance readings between radiometer brands, and between irradiance values recorded by the three samples of each brand studied. This made it impossible to definitively rank the radiometer brands for accuracy. Within the ±20% bioequivalence limits of this study, there was a clinically significant difference in the irradiance readings between radiometer brands and the choice of curing light affected the results. There was also significant variation in irradiance readings reported by different examples of the same brand of radiometer. Whether in clinical practice or in research, dental radiometers should not be used when either the irradiance or energy delivered needs to be accurately known.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Light-cured resin composites are routinely used in dental offices as restorative materials and as luting agents [1]. Originally, quartz tungsten halogen (QTH) light-curing units (LCUs) were used to photopolymerize these materials, but now plasma arc (PAC) lights, lasers, and, recently, light-emitting diode (LED) units are also used. The durability of light-cured resin composite restorations and luting agents depends on adequate polymerization of the resin component within these products. However, the LCUs in many dental offices worldwide do not deliver an adequate light output [2–6]. The bulbs, LEDs, reflectors, and internal filters in dental LCUs have all been shown to degrade with use [7, 8]. In addition, autoclaving, disinfectant chemicals, or restorative material adhering to the tip of the LCU can all dramatically reduce the light output [9–11]. Any of these factors may account for substandard polymerization of resins, especially if the user is unaware of the decline in light output.
Previous studies have reported that dental radiometers are unable to accurately measure the light output from dental LCUs. Shortall et al. showed that although relative irradiance values were attained according to the depth of cure of the resin, the absolute irradiance values reported by dental radiometers were not accurate [12]. In addition, Hansen and Asmussen reported that three handheld radiometers were unreliable in ranking 20 curing units on their ability to cure resin [13]. Another study by Rueggeberg et al. on the precision of radiometers found that the absolute irradiance values from two dental radiometers were significantly different [14].
Dental radiometers usually contain silicon photodiodes that convert light into electric current, then an analogue or digital meter displays the output from the curing light. Several factors may be responsible for the inaccuracy of dental radiometers. For example degradation of the radiometer over time and variability in the original calibration of the radiometer may affect the accuracy. Also, it has been reported that differences in the light guide tip diameter can significantly affect dental radiometer readings [15]. In addition, since LCUs deliver different spectral emissions, the type of bandpass filter used within these radiometers will affect the type of curing light (QTH, PAC, or LED) that used on that particular radiometer [16]. In particular measuring QTH curing lights with an LED-oriented radiometer has been reported to yield values higher than expected. This is of clinical concern because it may result in the operator believing that the output is higher and delivering insufficient energy to adequately cure the resin [16].
Despite the reports indicating that there are statistical differences between different radiometers, [13–16] these differences may not be clinically relevant because there is no universal standardization of the information that dental radiometers provide. Additionally, although general guidelines for assessing the substantial equivalence of medical/dental devices, e.g., 510(K), exist [17], no standard methodology is specified by licensing agencies when determining equivalence of dental radiometers, as is the case for pharmaceutical bioequivalence [18]. Consequently, although many dental manufacturers, researchers and clinicians have used dental radiometers to measure the irradiance from curing lights [2, 3, 5, 6, 19–24], the actual irradiance delivered to the specimens may be in question.
The hypotheses of this study are:
-
1.
That four popular brands of commercial dental radiometers will produce irradiance values that are bioequivalent to values from a laboratory-grade power meter;
-
2.
That the accuracy of dental radiometers is the same between commercial brands; and
-
3.
That there is no significant difference in irradiance values recorded by the same brand of radiometer.
Materials and methods
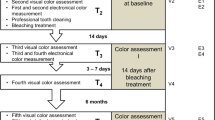
Table 1 and Fig. 1 show the four brands of dental radiometers and two laboratory-grade National Institute of Standards and Technology (NIST, Gaithersburg, MD, USA) referenced thermopiles (10-W PM-10, Coherent, Santa Clara, CA, USA) used in the study. The two thermopiles were used as the “gold standard” and for hypothesis 1; the irradiance results reported by the dental radiometers were compared to the results from this gold standard. To test hypothesis 2, readings from the four different brands of radiometer were compared for inter-brand variability. To test hypothesis 3, the results from the three examples of each brand of radiometer were compared for intra-brand variability.
Table 2 lists the 14 different LCUs that were measured in random order by the radiometers. The LCUs tested varied from a broad spectrum plasma arc curing light and halogen curing light, to single-peak and polywave™ LED units. The exit apertures at the end of the curing lights were often larger than the diameter of the dental radiometer sensor window. To calculate irradiance from the power values (in milliwatts) measured using the thermopiles, the internal diameter of the light tip was measured using ×2.5 magnification. The power output obtained from the thermopile was divided into the area of the light-emitting tip to obtain the average irradiance (milliwatts per square centimeter). The spectral emissions from the LCUs shown in Figs. 2 and 3 were measured with a laboratory-grade USB 4000 spectroradiometer (Ocean Optics, Dunedin, FL, USA) connected to a 6-in. integrating sphere (Labsphere, North Sutton, NH, USA) that had an internal NIST referenced 35-W calibration lamp.
The irradiance results from the PM#1 and PM#2 meters were compared; accuracy was inferred if these two NIST referenced meters gave similar readings. Each light was positioned with the end tip of the light guide parallel to and 1 mm from the surface of the thermopile sensor. The Field Max II TO (Coherent) meters reported the mean power during the last 5 s of a 10-s curing cycle. To record the output of the curing lights on the dental radiometers, the tip of the light guide was positioned flush on a non-sensor surface area of the radiometer for the first 5 s. In a horizontal sliding motion, the tip of the light guide was moved to cover the radiometer sensor for the last 5 s. The maximum radiometer reading obtained with the tip of the curing light in contact with the dental radiometer sensor window was recorded. The battery-operated curing lights were fully charged before their outputs were tested. Each curing light was used for 20 s prior to being measured so that the light source could warm up and the light output would stabilize [24].
To ensure proper representation of each brand of dental radiometer, three examples of each brand of meter were used. The experiment was repeated three times on different days and the lights and meters were used in a random order for each trial. Data collected was analyzed using analysis of variance, with 95% confidence intervals (C.I.), comparing the results from the gold standard thermopiles to those from the dental radiometers. Bioequivalence was established if the confidence interval for the irradiance values were within ±20% of the gold standard thermopile reading [25]. Forest plots were used to highlight the bioequivalence results [26].
Results
On average, when measuring the 14 different lights, the irradiance values from the two laboratory-grade meters differed by less than 0.6%: 1,142.7 vs. 1,148.8 mW/cm2, with an average difference of −6.05 [95% confidence interval: −9.09, –3.01 mW/cm2]. Thus, the results obtained from the two laboratory-grade meters were combined and the mean irradiance value was reported in Table 3.
Table 4 and the Forest plots in Fig. 4 show the average irradiance values produced from all the radiometers compared to the gold standard laboratory-grade power meters. Overall nine radiometers passed the ±20% bioequivalence standard. The CureRite meter #3 followed by the Bluephase meter #3 recorded the irradiance values closest to the gold standard and passed a ±10% bioequivalence standard. In sharp contrast, CureRite meter #1 and CureRite meter #2 performed poorly and were not bioequivalent. Although the irradiance reported by the SDI meter #2 was on average the closest to the gold standard, Table 4 shows that the confidence interval for this meter was wider, indicating less precision in the irradiance values from this radiometer. To account for different types of radiometers potentially responding better to different categories of dental curing light, radiometer ability was analyzed separately using the results just from the single-peak LED, polywave™ LED, QTH, and PAC curing lights.
Comparison of mean irradiance values from the dental radiometers measuring all of the lights. Vertical line in the center of the graph indicates an average of the laboratory-grade meter values. Square points indicate mean irradiance values, lines indicate lower to upper 95% confidence limits for the mean. CureRite meter #3 and Bluephase #3 performed best at ±10% bioequivalence [C.I. −57.4, 77.0 mW/cm2, and C.I. −82.0, 61.7 mW/cm2, respectively] and CureRite meters #1 and #2 performed the worst at ±40% bioequivalence [C.I. −374.6, −219.5 mW/cm2 and C.I. −454.7, −300.7 mW/cm2, respectively]. SDI meter #2 had the closest readings to the thermopile, but had a large confidence interval [C.I. −116.8, 117.6 mW/cm2] indicating less precision
The performance of dental radiometers with single-peak LED lights is shown in Fig. 5 and Table 5. Here, eight of the radiometers passed the ±20% bioequivalence standard and the CureRite #3 passed a ±10% bioequivalence standard. The CureRite meter #3 and Bluephase meters #1 and #3 were the best, but the CureRite meters #1 and #2 performed poorly and were not bioequivalent. The ability of radiometers to measure polywave™ LED lights is shown in Fig. 6 and Table 6. The Bluephase meters #1 and #3 tested as most accurate and the most precise. These two meters passed a ±10% bioequivalence standard. Although the CureRite #3 passed the ±20% bioequivalence standard, it was slightly less accurate and less precise having a wider confidence interval than the Bluephase meters #1 and #3. In general, the confidence intervals for polywave™ measurements were very wide and thus very imprecise. Although six meters passed the ±20% bioequivalence standard, most radiometers were imprecise and thus unreliable. CureRite meters # 1 and #2 were not bioequivalent and were the least accurate meters.
Comparison of mean irradiance values from the dental radiometers tested with single-peak LED curing lights. Vertical line in the center of the graph indicates an average of the laboratory-grade meter values. Square points indicate mean irradiance values, lines indicate lower to upper 95% confidence limits for the mean. The majority of lights passed the ±20% bioequivalence standard. CureRite meter #3 performed best at ±10% bioequivalence [C.I. −102.3, 70.2 mW/cm2], Bluephase meters #1 and #3 were at ±20% bioequivalence [C.I. −117.3, 111.36 mW/cm2 and C.I. −99.2, 122.8 mW/cm2, respectively]. CureRite meters #1 and #2 performed most poorly at ±40% [C.I. −451.1, −343.7 mW/cm2] and ±50% [C.I. −523.1, −410.6 mW/cm2] bioequivalence, respectively
Comparison of mean irradiance values from the dental radiometers tested with polywave™ LED curing lights. Vertical line in the center of the graph indicates an average of the laboratory-grade meter values. Square points indicate mean irradiance values, lines indicate lower to upper 95% confidence limits for the mean. Although the majority of lights tested passed the ±20 bioequivalence standard, the large confidence intervals involved render these readings highly imprecise. Bluephase meters #1 and #3 performed best at ±10% bioequivalence [C.I. −80.0, 57.0 mW/cm2 and C.I. −47.9, 29.3 mW/cm2, respectively]; CureRite meter #3 was ±20% bioequivalence [C.I. −107.6, 145.7 mW/cm2]. CureRite meter #1 and #2 performed poorest at ±40% [C.I. −383.6, −23.4 mW/cm2] and ±50% [C.I. −476, −120 mW/cm2] bioequivalence, respectively
The ability of the radiometers to measure QTH units is shown in Fig. 7 and Table 7. Eight radiometers passed the ±20% bioequivalence standard. The LEDRadiometer #3 and SDI meters # 1 and #2 measured closest to the gold standard. CureRite meters #1 and #2 were again the least accurate radiometers, and together with Bluephase meter #1 had a very wide confidence interval. This indicated a lack of precision when measuring QTH curing lights.
Comparison of mean irradiance values from the dental radiometers tested with a halogen curing light. Vertical line in the center of the graph indicates an average of the laboratory-grade meter values. Square points indicate mean irradiance values, lines indicate lower to upper 95% confidence limits for the mean. Most radiometers passed the ±20% bioequivalence. LEDemetron meter #3 [C.I. −476.0, −120.0 mW/cm2] and SDI meter # 1 and #2 measured at ±10% bioequivalence [C.I. 19.5, 91.7 mW/cm2 and C.I. 22.9, 81.6 mW/cm2 respectively]. CureRite meter #1 and #2 were the least accurate [C.I. −409.1, −240.2 mW/cm2 and C.I. −492.7, −428.1 mW/cm2 respectively], and Bluephase meter #1 also had a very wide, inaccurate confidence interval [C.I. −462.1, 43.3 mW/cm2]
The ability of the radiometers to measure the PAC unit is shown in Fig. 8 and Table 8. The Bluephase meter #3 was the only radiometer that passed the ±20% bioequivalence standard. All the other radiometers gave highly inaccurate and imprecise readings.
Comparison of mean irradiance values from the dental radiometers tested with a plasma arc curing light. Vertical line in the center of the graph indicates a confidence limit of the laboratory-grade meter. Square points indicate mean irradiance values, lines indicate lower to upper 95% confidence limits for the mean. Bluephase meter #3 was the most accurate radiometer, at 20% bioequivalence [C.I. −182.7, 113.8 mW/cm2]. All other meters gave highly inaccurate readings with five of the radiometers off the chart
Discussion
In this study, there was a bioequivalent difference between the irradiance values reported by the four brands of dental radiometers and the gold standard laboratory-grade power meters. As a group, the meters failed to meet the ±20% bioequivalence standard we used, thus hypothesis 1 was rejected. However, individually, the three examples of the Bluephase and SDI radiometers as well as two examples of the LEDRadiometer and one CureRite meter passed the ±20% bioequivalence standard. Hypothesis 2 was rejected, as there was a significant variability of the irradiance readings between brands. Finally, hypothesis 3 was rejected as there was a significant variation between irradiance values found in the three samples of each brand studied, making it impossible to definitively rank brands for accuracy.
Equivalence testing was possible because the readings from the two laboratory meters differed by less than 0.5%, with an average difference of 6 mW/cm2 (95% CI −9, −3 mW/cm2). Instead of using statistically significant differences that are often quoted as p < 0.05, this study used a 95% confidence interval for the mean irradiance values lying within ±20% of the gold standard (laboratory meters) as the equivalence standard. This standard is analogous to the method for comparing the pharmacokinetic parameter between a generic drug see\king approval and its brand-name counterpart. The American Food and Drug Administration considers two products bioequivalent if the 90% confidence intervals (90% CI) of the results obtained using a generic formulation are within 80.00% to 125.00% of the reference formulation [18]. Although other metrics are possible, this one is used widely in other areas and may be more clinically relevant [25]. Table 4 and Fig. 4 show that measuring all the lights, overall, all three examples of the Bluephase and SDI radiometers were found to be ±20% bioequivalent to the gold standard, as well as LEDRadiometer #2 and #3, and CureRite meter #3. In fact, CureRite meter #3 met a more stringent bioequivalence standard of ±10%. Table 5 and Fig. 5 show that when tested with single-peak LED units, again, all the Bluephase radiometers were bioequivalent, as were LEDRadiometer #2 and #3 as well as the SDI #2 and 3 meters. The CureRite meter #3 was bioequivalent at ±10%. As anticipated, all the Bluephase radiometers were bioequivalent when tested on the polywave™ LED units, as were the LEDRadiometer #2 and #3, and the CureRite meter #3. In particular, the Bluephase meters #1 and #3 were the most accurate at ±10% bioequivalence when testing the polywave™ LED units. As shown in Fig. 7 and Table 7, when tested on the QTH units, the LEDRadiometer and SDI radiometers along with the Bluephase meter #2 and CureRite #3 passed the ±20% bioequivalence standard. Overall, the radiometers had the best results when tested on the QTH units with six of the radiometers meeting a ±10% standard of bioequivalence. Table 8 and Fig. 8 show readings taken from the PAC unit were generally beyond the limits of the Forest plot and were thus both highly inaccurate and imprecise with only the Bluephase meter #3 meeting the ±20% bioequivalence standard.
The different LCUs tested in this study represent the range of QTH, LED, and PAC units commonly used in dental offices. Figures 2 and 3 show that there is a wide range in the spectral emission from the LCUs used in this study. Figure 1 illustrates the different designs of dental radiometers used in this study and it was expected that the company’s corresponding brand of radiometer would function most accurately with their own brand of light [14, 15]. For instance, Ivoclar-Vivadent manufactures both single-peak and polywave™ curing lights and, as expected, the Ivoclar-Vivadent Bluephase radiometers performed best, with these lights meeting the ±20% bioequivalence standard. However, the other brands of radiometer did not function as expected. The Dentsply CureRite radiometers were designed for QTH units [27], but they performed the most poorly on the QTH light. SDI & Kerr make single-peak type LED curing lights, but in this study the SDI & Kerr radiometers [28, 29] gave the most accurate readings for the QTH unit, and were least accurate when measuring single-peak LED curing lights.
This study found a wide variation in the results from the three radiometer samples within the same brand, making it impossible to definitively rank brands for accuracy. Overall, testing the 14 curing lights, the CureRite #1 and #2 radiometers were the least accurate radiometers, but the CureRite meter #3 performed best overall. This illustrates the large variation that can occur within the same brand of dental radiometer. The time when each sample was manufactured may explain some of these differences (Table 1). For instance, serial numbers from the Bluephase meters #1 and #2 (serial #49, 32) suggest that these meters were manufactured at a different time period than the Bluephase meter #3 (serial #1431) and Bluephase #3 was a more accurate meter achieving a ±10% bioequivalence standard. The same inconsistency within a brand of radiometer is seen in CureRite meters #1, #2, and #3, but here the serial numbers appear to be unrelated to radiometer performance. Although meters #1 and #3 have relatively similar serial numbers (serial #7213, 7614) compared to meter #2 (serial #5615), the CureRite meter #3 was more accurate achieving a ±10% bioequivalence standard compared to meters #1 or #2.
None of these dental radiometers could be relied upon to accurately report the irradiance from a range of dental LCUs and thus should not be used in research studies that require the irradiance or energy delivered to the specimens to be known. Clinicians should not try to compare the irradiance values from different curing lights using dental radiometers because the results may or may not be accurate. Additionally, the different brands of dental radiometers cannot be relied upon to always provide a higher or lower irradiance value than the gold standard. However, dental radiometers such as those used in this study can be useful in dental offices as a means to measure the change in the irradiance from a single light over time. Future studies are planned to assess the variation in the accuracy of these radiometers over a period of several years.
Conclusions
Within the ±20% bioequivalence standard used in this study, it was concluded that:
-
1.
Overall, as a group, the dental radiometers were not bioequivalent to the gold standard laboratory-grade meters. However, individually, all three examples of the Bluephase and SDI radiometers as well as two examples of the LEDRadiometer and one CureRite meter were bioequivalent to the gold standard.
-
2.
There was a clinically significant difference in the irradiance readings recorded by the four brands of radiometer tested in the study.
-
3.
There can be a significant and wide variation in the irradiance readings within different examples of the same brand of dental radiometer and the clinician cannot tell which radiometer is accurate.
References
Rueggeberg FA (2002) From vulcanite to vinyl, a history of resins in restorative dentistry. J Prosthet Dent 87(4):364–379
Hegde V, Jadhav S, Aher GB (2009) A clinical survey of the output intensity of 200 light curing units in dental offices across Maharashtra. J Conserv Dent 12(3):105–108
Barghi N, Fischer DE, Pham T (2007) Revisiting the intensity output of curing lights in private dental offices. Compend Contin Educ Dent 28(7):380–384, quiz 385–386
Pilo R, Oelgiesser D, Cardash HS (1999) A survey of output intensity and potential for depth of cure among light-curing units in clinical use. J Dent 27(3):235–241
El-Mowafy O, El-Badrawy W, Lewis DW, Shokati B, Kermalli J, Soliman O, Encioiu A, Zawi R, Rajwani F (2005) Intensity of quartz–tungsten–halogen light-curing units used in private practice in Toronto. J Am Dent Assoc 136(6):766–773, quiz 806–767
El-Mowafy O, El-Badrawy W, Lewis DW, Shokati B, Soliman O, Kermalli J, Encioiu A, Rajwani F, Zawi R (2005) Efficacy of halogen photopolymerization units in private dental offices in Toronto. J Can Dent Assoc 71(8):587
Friedman J (1989) Variability of lamp characteristics in dental curing lights. J Esthet Dent 1(6):189–190
Ernst CP, Busemann I, Kern T, Willershausen B (2006) Feldtest zur Lichtemissionsleistung von Polymerisationsgeräten in zahnärztlichen Praxen. Dtsch Zahnärztl Z 61(9):466–471
Dugan WT, Hartleb JH (1989) Influence of a glutaraldehyde disinfecting solution on curing light effectiveness. Gen Dent 37(1):40–43
Strydom C (2002) Dental curing lights—maintenance of visible light curing units. SADJ 57(6):227–233
Rueggeberg FA, Caughman WF, Comer RW (1996) The effect of autoclaving on energy transmission through light-curing tips. J Am Dent Assoc 127(8):1183–1187
Shortall AC, Harrington E, Wilson HJ (1995) Light curing unit effectiveness assessed by dental radiometers. J Dent 23(4):227–232
Peutzfeldt A (1994) Correlation between recordings obtained with a light-intensity tester and degree of conversion of a light-curing resin. Scand J Dent Res 102(1):73–75
Rueggeberg FA (1993) Precision of hand-held dental radiometers. Quintessence Int 24(6):391–396
Leonard DL, Charlton DG, Hilton TJ (1999) Effect of curing-tip diameter on the accuracy of dental radiometers. Oper Dent 24(1):31–37
Roberts HW, Vandewalle KS, Berzins DW, Charlton DG (2006) Accuracy of LED and halogen radiometers using different light sources. J Esthet Restor Dent 18(4):214–222, discussion 223–214
Food and Drug Administration (2010) Medical Devices: Premarket Notification (510K): http://www.fda.gov/medicaldevices/deviceregulationandguidance/howtomarketyourdevice/premarketsubmissions/premarketnotification510k/default.htm. Accessed March 23 2011
U.S. Department of Health and Human Services Food and Drug Administration Center for Veterinary Medicine (CVM) (2003) Guidance for Industry. Bioavailability and Bioequivalence Studies for Orally Administered Drug Products—General Considerations: http://www.fda.gov/downloads/AnimalVeterinary/GuidanceComplianceEnforcement/GuidanceforIndustry/UCM052363.pdf. Accessed March 23 2011
Takubo C, Yasuda G, Murayama R, Ogura Y, Tonegawa M, Kurokawa H, Miyazaki M (2010) Influence of power density and primer application on polymerization of dual-cured resin cements monitored by ultrasonic measurement. Eur J Oral Sci 118(4):417–422
Cadenaro M, Navarra CO, Antoniolli F, Mazzoni A, Di Lenarda R, Rueggeberg FA, Breschi L (2010) The effect of curing mode on extent of polymerization and microhardness of dual-cured, self-adhesive resin cements. Am J Dent 23(1):14–18
Retamoso LB, Onofre NM, Hann L, Marchioro EM (2010) Effect of light-curing units in shear bond strength of metallic brackets: an in vitro study. J Appl Oral Sci 18(1):68–74
Topcu FT, Erdemir U, Sahinkesen G, Yildiz E, Uslan I, Acikel C (2010) Evaluation of microhardness, surface roughness, and wear behavior of different types of resin composites polymerized with two different light sources. J Biomed Mater Res B Appl Biomater 92(2):470–478
Rahiotis C, Patsouri K, Silikas N, Kakaboura A (2010) Curing efficiency of high-intensity light-emitting diode (LED) devices. J Oral Sci 52(2):187–195
Felix CA, Price RB (2003) The effect of distance from light source on light intensity from curing lights. J Adhes Dent 5(4):283–291
Guidance for industry: statistical approaches to establishing bioequivalence (January 2001). U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research, Rockville MD
Lewis S, Clarke M (2001) Forest plots: trying to see the wood and the trees. Br Med J 322(7300):1479–1480
Dentsply (2003) CURE RITE: Visible Light Curing Meter. DENTSPLY, Milford
SDI (2001) LED Light Curing Meter: product information. SDI, Bayswater
Kerr (2001) LED Radiometer by Demetron—Operator manual. http://www.kerrdental.com/index/cms-filesystem-action?file=KerrDental-Products-DFU/dfu-ledradiometer-960764.pdf. Accessed June 29, 2010
Acknowledgment
The assistance of Thomas Lumley, Professor of BioStatistics, The University of Auckland, New Zealand is gratefully acknowledged. The research was partially funded by Ivoclar-Vivadent who provided an unrestricted research grant to Dalhousie University and by a NSERC Discovery Grant # 298326.
Conflict of interest
The authors declare that they have no conflict of interest with any of the manufacturers of the products used in this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Price, R.B., Labrie, D., Kazmi, S. et al. Intra- and inter-brand accuracy of four dental radiometers. Clin Oral Invest 16, 707–717 (2012). https://doi.org/10.1007/s00784-011-0562-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-011-0562-7