Abstract
Chipping of the applied veneering ceramic is reported to be a main clinical failure type of computer-aided design/computer-aided manufacturing- or manually copy-milled zirconia restorations. The aim of this in vitro study was to investigate whether different substructure designs and veneering processes done by different dental technicians do significantly influence chipping in zirconia-based all-ceramic fixed dental prostheses during simulated oral service. Five groups (n = 8 per group) of three-unit zirconia substructures were fabricated in three different laboratories using copy-milling technique. Three series were veneered with identical porcelain (groups 1–3) and one with a second different porcelain (group 4). The fifth group was milled to final contour design without veneering. Dimensions of the connector areas were determined. All fixed partial dentures (FPDs) were adhesively boned on human teeth and thermally cycled and mechanically loaded (1.2 × 106 × 50 N; 6,000 × 5°C/55°C) using human antagonists. Restorations were monitored during thermal cycling and mechanical loading (TCML). FPDs which survived were loaded to fracture. FPDs which failed during TCML were investigated with fractographic means. During TCML, chipping took place in groups 1 (two times), 2 (four times) and 3 (five times) (Table 1). Chipping areas varied between 2.3 mm2 (group 3) and 58.7 mm2 (group 2). Groups 4 and 5 provided no failures during TCML. Failure in all cases started from contact points, where superficial wear and disruption of the porcelain were found. No significant correlation could be determined between connector thickness and number of failures. Median fracture results varied between 1,011 N (group 3) and 2,126 N (group 2). The results show the necessity of considering individual design and manufacturing of restorations as well as contact situation. Advanced technical training on zirconia-based restorations is recommended.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Yttria-stabilized zirconia ceramics are available as alternatives for metal-supported restorations. Substructures that are made of partially stabilized zirconia provide high fracture strength, high structural reliability and a small range of strength variation compared to glass ceramics [1, 2]. Zirconia is processed in computer-aided design/computer-aided manufacturing (CAD/CAM) or CAM technologies and has been investigated thoroughly in the past years under in vivo conditions [3–5]. For reducing technological expenditure, manually controlled copy-milling techniques are available.
After milling, zirconia typically has to be veneered with porcelain in layering or press technique. This veneering porcelain shows lower strength compared to high-strength zirconia [6]. Alternatively, full-zirconia restorations can be fabricated with occlusal design without veneering (Prettau, Zirkonzahn, Gais, Italy). When applied, veneering porcelain is directly exposed to chewing, clenching and moisture which might weaken the veneering and result in cracks or chipping [7, 8]. Although chipping has been described with porcelain fused to metal restorations [9, 10], it is especially examined and currently discussed with zirconia restorations [3–5, 11, 12]. Various factors that might influence chipping occurrence have been reported: veneering thickness and occlusal support [13], morphology of the circular finishing line, adhesive forces between substructure and veneering [14], negative effects because of the combined different material layers [15–17] or residual stresses influenced by the cooling protocol during the veneering process [18]. The question arises, whether failure types and pattern may be influenced by the individual design of restorations with its occlusal variations and therefore different effects on loading and force distribution. The design of the restoration strongly depends on the residual dentition as well as on skills and preferences of the individual dental technician. Therefore, the fabrication process of the substructure and the veneering process in the different dental laboratories, especially with individualised copy milling, gains importance.
Chewing simulations [19], which imitate the clinical situation with dynamic loading and thermal cycling, may help to investigate specimen behaviour under clinically approximated conditions [20, 21] Fractographic methods [22, 23] can be used to describe ceramic failures, which appear during the simulation, and to compare the results with the clinical situation. These failures are in most cases initiated by flaws inside the material or defects in marginal or occlusal areas [24]. If no failures occur during simulation, a subsequent static fracture test may help to locate of initiated weak points. It may also allow for comparison of the tested materials with clinically well-known systems. However, these static benchmark tests may reveal different failure patterns in comparison to in vivo situations.
The hypothesis tested in this study was that different substructure design and the veneering process from different dental technicians do significantly influence chipping in zirconia-based all-ceramic fixed dental prostheses (FDPs) during simulated oral service.
Materials and methods
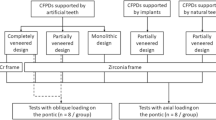
The roots of human maxillary molars (n = 80) were coated with a 1-mm-thick layer of polyether material (Impregum; 3M Espe, Seefeld, Germany) to simulate periodontal mobility and inserted into PMMA resin (Palapress Vario; Kulzer, Wehrheim, Germany) forming a molar oral gap of 10 mm. Loaded with 50 N, the layer allows a maximum mobility of the single tooth in axial and vertical direction of 0.1 mm. All teeth were prepared according to the directives for ceramic restoration techniques, using a 1-mm-deep circular shoulder preparation. Polyether impressions (Permadyne; 3M Espe) and working dyes were made of class IV dental stone (Fuji Rock; GC Corporation, Tokyo, Japan). Models and human antagonists were delivered to three different dental laboratories for the fabrication of three-unit fixed partial dentures (FPDs). In all cases, the substructures were copy milled (Zirkograph; Zirkonzahn). Veneering was applied in layering technique using two different porcelains (A and B) without pre-treatment of the zirconia substructures. Five different examination groups were provided:
-
1)
Laboratory A: zirconia substructures, veneering A
-
2)
Laboratory B: zirconia substructures, veneering A
-
3)
Laboratory C: zirconia substructures, veneering A
-
4)
Laboratory C: zirconia substructures, veneering B
-
5)
Laboratory C: zirconia substructures (Prettau zirconia; Zirkonzahn), no veneering
Substructures in groups 1–4 were fabricated of zirconia (ICE; Zirkonzahn; veneering A: silica based; firing temperature (FT), 780°C; thermal expansion (TE), 8.7 × 1.2 × 10−6/K and veneering B: ICE: silica based; FT, 820°C; TE, 9.6 × 1.2 × 10−6/K). FPDs and human molar antagonists were adjusted in a dental articulator (Artex CN; Amann-Girrbach, Pforzheim, Germany) during fabrication process. Dimensions (height and width) were measured at both abutment teeth at the connectors (A, B) and in the centre of the FDP.
All FPDs were adhesively bonded using dual-curing resin cement (Variolink2) with corresponding primer and bonding system (Syntac classic; both from Ivoclar-Vivadent, Schaan, Liechtenstein). A bite registration was used for transferring FPDs and antagonists into the chewing simulator (EGO; Regensburg, Germany). Thermal cycling (6,000 × 5°/55°; 2 min each cycle) and mechanical loading (1.2 × 106 × 50 N) was performed with parameters based on literature data which are supposed to simulate 5 years of oral service [20, 21]. During simulation time, all FPDs were monitored, appearing failures were documented and failed FDPs were excluded from further simulation process. Location (mesial, distal, buccal or lingual direction) and extension (width, height and area) of the occurring failure modes were determined. Scanning electron microscopy (SEM; magnification, 10–1,000×; working distance, 20.4 mm; voltage, 5 keV; low vacuum; Quanta; FEI-Phillips, Eindhoven, Netherlands) was used to do fractographic failure analysis. Therefore, overview and detailed micrographs were made.
All FPDs, which survived thermally cycled and mechanically loaded ageing without chipping, were loaded until failure using a testing machine (Zwick, Ulm, Germany, v = 1 mm/min). The force was applied using a steel ball (d = 12 mm), while a tin foil (1 mm) between pontic and antagonist prevented force peaks. FPDs which failed during thermal cycling and mechanical loading (TCML) were excluded from the fracture test. The FPDs were optically examined before and after fracture testing. Failure mode was divided into fracture of veneering, crown or core. Medians and 25%/75% of the fracture resistance [newton] were calculated. Statistical analysis was performed using Mann–Whitney U test (Kolmogorov–Smirnov test; Chi-square; α = 0.05).
Results
During TCML, chipping of the veneering took place in groups 1 (two times), 2 (four times) and 3 (five times) (Table 1). Most chippings were located in lingual directions. One chipping in groups 1 and 2 was found in buccal direction. Chipping areas were 29.7 mm2 (group 1) and 28.5 mm2 (group 2) in buccal direction. Areas varied between 2.3 mm2 (group 3) and 58.7 mm2 (group 2) in lingual direction. Groups 4 and 5 provided no failures during TCML (Table 1). No significant (p = 0.168) correlation was found between thickness of the connector and number of failures (Table 2). Failure in all cases started from a contact point, where superficial wear and disruption of the porcelain were found. Exemplary SEM micrographs are provided as detailed figures (Figs. 1–5).
No significant differences in fracture resistance were found between the individual groups (p > 0.055), with the exception of groups 2 (2,126 N) and 4 (1,141 N; p = 0.042). Median fracture results varied between 1,011 N (group 3) and 2,126 N (group 2). Failures in the fracture test were chipping (two times), core fracture (eight times) and fracture at the crown coping (19 times). The dimensions of the connector had no significant influence on the fracture results (0.9 > p > 0.054). (Table 1).
Discussion
The hypothesis of this study that chipping in zirconia FDPs, which are delivered by different dental laboratories, is influenced by the individual substructure design and veneering process had to be confirmed. In contrast to expectations, no significant correlation was found between chipping and the final dimensions of the connectors, although the dimensions varied between the individual groups.
The search for the reason of the individual chipping differences is strongly characterized by the basic idea to investigate no standardized, but individually shaped, FPDs. The design of the FPDs was strongly influenced by shape and size of the individual teeth and the individual fabrication process by the different dental laboratories. Human molars were used to ensure a clinical relevant modulus of elasticity of the abutments and to simulate a relevant bonding between FPDs and teeth. Human antagonists create a clinically relevant loading and wear at the occlusal surface of the examined restorations. Direct comparability of loading situations and fracture results of the individual FPDs is therefore limited. TCML parameters have been chosen congruent to numerous other in vitro studies. They are known to simulate restoration stress according to a 5-year period of intraoral use [20, 21]. Under oral conditions the contact between antagonist and tooth is sensory regulated, therefore pneumatically controlled TCML may cause impact conditions on the crown surface, which might only be comparable to the clinical situation with limitations.
As cracks and chipping occurred in most of the tested groups, it seems to stay as a problem in zirconia-based FPDs. Failure reasons are supposed to be occlusal overload, stress corrosion, fatigue or improper structure design [25]. Antagonists cause occlusal wear (see Figs. 1, 2, 3, 4, 5) by means of chewing impact and clenching and roughening of the porcelain surface. These flaws or superficial ruptures cause crack initiation, and flaws can propagate through the veneering without being stopped or deflected. As described earlier for crowns [22], a worst case scenario may be produced if the FPDs are fabricated in a simple shape-reduced design without occlusal support for the veneering porcelain. The high strength of zirconia and the individual copy-milling process even allow for the fabrication of a small substructure thickness, reduced connector areas or thin crown copings. Therefore, the high number of chippings may be influenced by a low support by the substructure and high thickness of the veneering. This would conform to the crack initiation in two and three layer systems [15–17] and the description of cone cracking and radial cracking of the veneering. It is also in accordance with the failure type, where no interfacial failures between substructure and veneering were found, but solely chipping in the veneering.
There were obvious differences in the individual design of the restorations concerning the shape of the cusps. Rounded cusps and flat angles were found in groups 4 and 5 where no chipping occurred. In contrast, steep angled and edged cusps (groups 1–3) improve the optical appearance but were shown to influence chipping rates negatively. The force distribution during clenching and mastication [26] claims for a rounded cusp design for reducing chipping numbers. The location of the chipping in buccal and lingual directions may underline this theory: on the tested mandibular FPDs, main chewing forces occur in the central lingual areas. The non-load-bearing lingual cusps have to bear the side shift chewing forces. Thus, shearing forces produced by sliding and clenching mainly occur on distal and lingual directions and cause chipping failures. This theory would also conform to FEA [13] investigations showing the importance of a constant veneering thickness. Otherwise, in the mid-layer of the glass ceramic, a steady propagation of partial cones in the veneering may occur [7].
Different chipping rates between groups 3 and 4 may be related to the type of veneering porcelain or presumably its customization. Small differences were found between properties of varying veneering ceramics (flexural strength ∼ 90 MPa) [6] or the cooling protocol during the veneering process [18]. Both are supposed to be the reason for chipping. Therefore, the manufacturing process and handling are assumed to influence chipping performance, but fractography revealed no chipping origins due to layering failures. Chipping usually starts from wear and superficial deterioration. On a smooth round surface, the antagonist slides easily into the final situation with an optimal cusp–fossa relation. This might be a reason why crowns should be polished after occlusal adaptation, and polishing of porcelain crowns is recommended every now and then [27].
Fracture tests revealed significant differences only between individual groups. The type of fracture pattern (mainly fracture of the core or the crown) strongly varied from failures during TCML (chipping) and may indicate the high strength of the core along with a small influence of the individual core design on the strength of the FPDs. It had to be supposed that fracture tests did not allow for the interpretation of the influence of individual design of veneering porcelain on chipping of the FPDs.
The results of TCML show the necessity of looking at the occlusal design of restorations and the contact situation between antagonist and tooth: with increasing angle and edging of the cusps, shear loading and clenching increase, forcing wear and destruction of the loading points, fostering flaws, cracks and the chance of chipping. Further investigations on standardized specimens are necessary to improve the knowledge on the influence of the design (cusp rounding and angle, e.g.) of the restoration on chipping rates of fixed partial dentures.
References
Tinschert J, Natt G, Mautsch W, Augthun M, Spiekermann H (2001) Fracture resistance of lithium disilicate-, alumina-, and zirconia-based three-unit fixed partial dentures: a laboratory study. Int J Prosthodont 14:231–238
Guazzato M, Albakry M, Ringer SP, Swain MV (2004) Strength, fracture toughness and microstructure of a selection of all-ceramic materials. Part II. Zirconia-based dental ceramics. Dent Mater 20:449–456
Beuer F, Edelhoff D, Gernet W, Sorensen JA (2009) Three-year clinical prospective evaluation of zirconia-based posterior fixed dental prostheses (FDPs). Clin Oral Investig 13(4):445–451
Tinschert J, Schulze KA, Natt G, Latzke P, Heussen N, Spiekermann H (2008) Clinical behavior of zirconia-based fixed partial dentures made of DC-Zirkon: 3-year results. Int J Prosthodont 21:217–222
Sailer I, Feher A, Filser F, Gauckler LJ, Luthy H, Hammerle CH (2007) Five-year clinical results of zirconia frameworks for posterior fixed partial dentures. Int J Prosthodont 20:383–388
Fischer J, Stawarczyk B, Hammerle CH (2008) Flexural strength of veneering ceramics for zirconia. J Dent 36:316–321
Kim JW, Kim JH, Janal MN, Zhang Y (2008) Damage maps of veneered zirconia under simulated mastication. J Dent Res 87:1127–1132
Rekow ED, Zhang G, Thompson V, Kim JW, Coehlo P, Zhang Y (2009) Effects of geometry on fracture initiation and propagation in all-ceramic crowns. J Biomed Mater Res B Appl Biomater 88:436–446
Walton TR (2003) An up to 15-year longitudinal study of 515 metal-ceramic FPDs: Part 2: modes of failure and influence of various clinical characteristics. Int J Prosthodont 16:177–182
Tan K, Pjetursson BE, Lang N, Chan ESY (2004) A systematic review of the survival and complication rates of fixed partiel dentures (FPDs) after an observation period of at least 5 years. Clin Oral Implants Res 15:654–666
Reich S, Petschelt A, Lohbauer U (2008) The effect of finish line preparation and layer thickness on the failure load and fractography of ZrO2 copings. J Prosthet Dent 99:369–376
Al-Amleh B, Lyons K, Swain M (2010) Clinical trials in zirconia: a systematic review. J Oral Rehabil 37:641–652
De Jager N, Pallav P, Feilzer AJ (2005) The influence of design parameters on the FEA-determined stress distribution in CAD–CAM produced all-ceramic dental crowns. Dent Mater 21:242–251
Aboushelib MN, Kleverlaan CJ, Feilzer AJ (2006) Microtensile bond strength of different components of core veneered all-ceramic restorations. Part II: Zirconia veneering ceramics. Dent Mater 22:857–863
Lawn BR, Deng Y, Lloyd IK, Janal MN, Rekow ED, Thompson VP (2002) Materials design of ceramic-based layer structures for crowns. J Dent Res 81:433–438
Lawn BR, Pajares A, Zhang Y, Deng Y, Polack MA, Lloyd IK (2004) Materials design in the performance of all-ceramic crowns. Biomaterials 25:2885–2892
Thompson GA, Rekow DE (2004) Dental ceramics and the molar crown testing. J Appl Oral Sci 12:26–36
Swain MV (2009) Unstable cracking (chipping) of veneering porcelain on all-ceramic dental crowns and fixed partial dentures. Acta Biomater 5:1668–1677
Rosentritt M, Behr M, Gebhard R, Handel G (2006) Influence of stress simulation parameters on the fracture strength of all-ceramic fixed-partial dentures. Dent Mater 22:176–182
Rosentritt M, Siavikis G, Behr M, Kolbeck C, Handel G (2008) Approach for valuating the significance of laboratory simulation. J Dent 36:1048–1053
Rosentritt M, Steiger D, Behr M, Handel G, Kolbeck C (2009) Influence of substructure design and spacer settings on the in vitro performance of molar zirconia crowns. J Dent 37:978–983
Quinn JB, Quinn GD, Kelly JR, Scherrer SS (2005) Fractographic analyses of three ceramic whole crown restoration failures. Dent Mater 21:920–929
Scherrer SS, Quinn JB, Quinn GD, Kelly JR (2006) Failure analysis of ceramic clinical cases using qualitative fractography. Int J Prosthodont 19:185–192
Kelly JR (1999) Clinically relevant approach to failure testing of all-ceramic restorations. J Prosthet Dent 81:652–661
Bulpakdi P, Taskonak B, Yan J, Mecholsky JJJ (2009) Failure analysis of clinically failed all-ceramic fixed partial dentures using fractal geometry. Dent Mater 25:634–640
Dejak B, Mlotkowski A, Romanowicz M (2003) Finite element analysis of stresses in molars during clenching and mastication. J Prosthet Dent 90:591–597
Rosentritt M, Behr M, Thaller C, Rudolph H, Feilzer AJ (2009) Fracture performance of computer-aided manufactured ceramic and alloy crowns. Quint Inter 40(8):655–662
Acknowledgements
We would like to thank the dental laboratories for providing the restorations.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rosentritt, M., Kolbeck, C., Handel, G. et al. Influence of the fabrication process on the in vitro performance of fixed dental prostheses with zirconia substructures. Clin Oral Invest 15, 1007–1012 (2011). https://doi.org/10.1007/s00784-010-0469-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-010-0469-8