Abstract
The development of oral cancer proceeds through discrete molecular changes that are acquired from loss of genomic integrity after continued exposure to environmental risk factors. It is preceded in the majority of cases by clinically evident oral potentially malignant disorders, the most common of which is leukoplakia. Early detection of these oral lesions by screening methods using suitable markers is critical as it mirrors molecular alterations, long before cancer phenotypes are manifested. Assessment of salivary interleukin-6 (IL-6) as a marker of malignant progression was undertaken in patients with leukoplakia having coexisting periodontitis (n = 20), periodontitis patients without leukoplakia (n = 20), and healthy controls (n = 20) by competitive enzyme-linked immunosorbent assay. Results showed elevation of IL-6 levels in leukoplakia with coexisting periodontitis and in periodontitis patients when compared to healthy control (P < 0.001). Within the leukoplakia group, IL-6 level was found to be increased with increase in the severity of dysplasia. The use of tobacco was seen to play a significant role in the elevation of salivary IL-6.The importance of IL-6 as a specific marker for leukoplakia with dysplasia and the role of tobacco as an independent risk factor has been highlighted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The pathogenesis of oral squamous cell carcinoma (OSCC) is a result of multiple molecular events triggered by various topical carcinogens such as tobacco use [1], alcohol misuse [2], and possibly viruses against a background of heritable resistance and susceptibility [3]. Tobacco and alcohol misuse patterns have shown to account for nearly all of the observed racial differences in rates of oral cancers [4]. Accumulation of these genetic changes leads to oral cancer in some instances via clinically evident oral potentially malignant disorder (OPMD) [5], which may undergo sequential pathological changes from dysplasia to invasive carcinoma. Although environmental factors may play an important role in the etiology, some patients are susceptible, owing to an inherited trait in their ability or inability to metabolize carcinogens or procarcinogens, possibly along with an impaired ability to repair the DNA damage [4]. Leukoplakia is the most common of the OPMDs, with a risk of malignant transformation varying from 0.6% to 18% [6, 7]. Leukoplakia progressing to squamous cell carcinoma has been accepted to be directly related to the severity of dysplasia [8].
Measurement of suitable biomarkers has provided newer options for early detection and risk assessment of oral cancer. However, majority of these are identified either in serum, cell lines, or biopsy specimens, making it challenging for large-scale screening. Measurement of molecular markers in salivary fluid could potentially aid in development of a practical screening tool. The levels of certain inflammatory, proangiogenic cytokines in saliva, and tissue specimens of patients with oral cancer have been shown to be elevated. Significantly, levels of interleukin-6 (IL-6) and interleukin-8 (IL-8) have been shown to be consistently elevated in cancers of the head and neck with higher nodal stage [9].
In this study, we measured the level of IL-6 in whole unstimulated saliva (WUS) of patients with leukoplakia with dysplasia by competitive enzyme-linked immunosorbent assay (ELISA) and correlated the IL-6 levels with different grades of dysplasia. We hypothesized that salivary IL-6 levels would correlate strongly to level of dysplasia.
Material and methods
The study subjects were classified into three groups of 20 each based on the presence of leukoplakia and periodontitis. Group 1 consisted of patients with oral leukoplakia with histologically confirmed epithelial dysplasia, who presented with coexisting periodontitis. Group 2 were patients who had periodontitis without leukoplakia, and group 3 were healthy volunteers with normal oral mucosa. The saliva collected from group 1 patients constituted the test group, while those from group 2 and group 3 were considered as positive and negative controls, respectively.
Cases which were provisionally diagnosed as leukoplakia with dysplasia were graded by criteria put forth by Lumerman et al. [10]. The grading carried out by two independent observers was statistically analyzed using the Mann–Whitney U test to check for the interobserver variability. Since the interobserver variability was not significant, readings of just one observer were used for further statistical analyses.
Periodontal status (Community Periodontal Index) was recorded according to the criteria set forth by WHO [11] to ascertain uniform parameters for identical comparison. The presence of periodontitis was assessed dichotomously. The same examiner carried out the recordings for all the patients using Community Periodontal Index of Treatment Needs probe. Intra-examiner reliability was assessed by kappa statistics (kappa = 0.85). Only cases with more than three sextants having scores of 3 and 4 were considered as having chronic generalized periodontitis.
Prior to study enrolment, a written informed consent form approved by University Ethics Committee (UEC/9/2009), Manipal was obtained from all the volunteers. The WUS was collected from each of the participants and stored at −70°C till analyzed. The IL-6 level in WUS was estimated by ELISA using a commercially available kit (Immunotech, France). The IL-6 levels measured in leukoplakia patients were subsequently correlated with their corresponding histopathological indicators [12].
Patients included in the study were in their third to sixth decade of life with or without a history of tobacco use. WUS was collected only from male patients to eliminate any gender difference. The following patients were excluded from the study: patients who were on strenuous exercise regimen a day before, those who had caffeine (tea/coffee), chewed gum or drank water just prior to test, consumed dairy products 20 min prior to saliva collection, had sugar or acidic food at the time of test, were alcoholics or had alcohol, addictive drugs, glucocorticoids, estrogens, anticholinergics, antihistamines, antihypertensives, and beta-adrenergic blockers 24 h before sample collection, those who had mucosal lesions other than leukoplakia, and with systemic diseases like Sjögren’s syndrome and diabetes mellitus.
Collection of WUS
WUS was collected by standard techniques for 5 min [13] between 8:00 AM and 11:00 AM to avoid any diurnal variation in IL-6 levels. Patients were advised to rinse the mouth several times with deionized water and allowed to relax for 5 min. To increase the hydration, a waiting period of at least 10 min was necessary after rinsing and before collecting saliva to avoid sample dilution. With the head leaning forward, saliva was collected in wide mouth sterile containers using a funnel, sitting beside the patient by a simple drooling method. Containers were discarded after each use to comply with standard infection control procedures. The samples were stored at −70°C until analysis to minimize the effect of proteases present in saliva. Saliva was not stored longer than 2 months.
Salivary IL-6 calculation
Salivary analysis was done in one go to avoid repeated freeze–thaw cycles and to avoid sample degradation. The thawed salivary sample was centrifuged at 4,500 rpm/5 min and the supernatant collected in 5 ml vial. The concentration of salivary IL-6 in the supernatant was determined by an ELISA assay using A commercial kit [14] (Immunotech, France). Components of the kit were allowed to equilibrate for 30 min at room temperature before use. From the 1,000-pg/ml calibrator solution, a fresh dilution series in plastic tubes was prepared prior to each assay using diluent 1 for IL-6 in saliva (as per manufacturer’s instruction). This dilution series was used immediately and not stored. Briefly, 100 μl of calibrator or sample was added to each well along with 100 μl of IL-6 acetylcholinesterase conjugate and incubated for 2 h 18–25°C while shaking, following which the wells were washed with wash solutions. Two hundred microliters of substrate was added and incubated for 30 min in the dark while shaking. Finally, 50 μl of stop solution was added and absorbance recorded at 405 nm. Pipetting of substrate and stop solution was carried out quickly.
Calibrators and samples were assayed at the same time. A calibrator curve was plotted with each assay (Fig. 1). A calibrator curve was drawn on a semilog paper. The horizontal (X) axis represents the IL-6 concentration of the calibrators obtained by diluting calibrator solution, and the vertical (Y) axis represents the corresponding optical density (OD). Concentration of samples was determined by plotting the OD obtained from ELISA Reader on the Y-axis and drawing a horizontal to intersect the calibrator curve. Dropping a perpendicular from the point of intersect on the graph provided a value in picograms per milliliter on X-axis. The IL-6 level was expressed as a mean ± standard deviation.
Statistical analysis
The Statistical Package for Social Sciences 11.5 for Windows was used for analyzing the results. Analyses by one-/two-way analysis of variance (ANOVA) and Bonferroni correction method were used. A P value of less than 0.05 was considered to be significant. A regression analysis was applied to analyze both the dependent and independent variables.
Results
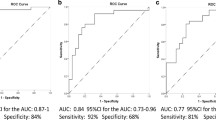
A detailed history was recorded and clinical examination carried out, and the characteristics of the different groups are described (Table 1). Salivary IL-6 in leukoplakia with coexisting periodontitis had a mean of 414.95 ± 36.69 pg/ml, while the periodontitis cases without leukoplakia had a mean of 311.35 ± 11.51 pg/ml. The control subjects had a mean of 17.15 ± 8.44 pg/ml (Fig. 2). One-way ANOVA for IL-6 levels with regard to the three study groups was statistically significant (Table 1). Multiple comparisons by post hoc Bonferroni analysis between the three study groups showed that each group was different with respect to each other (P < 0.001).
Further, two-way ANOVA for IL-6 level with respect to habits showed that group 1 patients with a positive history of tobacco habits had higher IL-6 levels (420.94 ± 36.67 pg/ml) compared to those without tobacco habits (381.00 ± 1.00 pg/ml). Similar observations were also noted in the group 2, where a higher level of IL-6 was noted in patients with tobacco habits (320.90 ± 7.02 pg/ml) as compared to those without the habit (301.80 ± 5.27 pg/ml). The healthy group 3 individuals also yielded similar findings, with IL-6 levels being higher in those with tobacco habits (24.90 ± 2.60 pg/ml) than those without its use (9.40 ± 3.17 pg/ml; Fig. 3). Every group was significantly different with respect to each other as demonstrated by Bonferroni analysis. IL-6 was significantly higher in all the three groups with a positive tobacco habit history than those without tobacco habits (P < 0.001).
One-way ANOVA for IL-6 levels with regard to different grades of dysplasia was statistically significant (P < 0.001). Eight individuals with mild dysplasia presented with a mean value of 385.63 ± 4.17 pg/ml. 7 individuals with moderate dysplasia yielded a mean value of 405.86 ± 5.01 pg/ml, while five individuals with severe dysplasia gave a mean value 474.60 ± 3.85 pg/ml (Tables 2 and 3). Regression analysis of the different groups showed that 98.6% of IL-6 variation was explainable by patient grouping and association with tobacco use (Table 4).
Discussion
Molecular markers which are identified and characterized in saliva have distinct advantages in pathological diagnosis as they reflect the overall health and disease states in an individual. Because of the anatomical proximity of saliva to the oral cavity, salivary testing would be ideal for evaluating potentially malignant and malignant oral lesions [15–17]. IL-6 is an NF-κB dependent cytokine produced by inflammatory cells as well as tumor cells [18]. The serum levels of IL-6 have been shown to be consistently elevated in patients with cancers of the head and neck and in patients with higher nodal stages [19]. It has also been shown to be an important serum biomarker for predicting therapeutic responses and survival in advanced-stage, head and neck cancer [20].
As NF-κB-dependent cytokine levels are shown to be significantly elevated in saliva of patients with preneoplastic lesions and OSCC [21], the potential value of IL-6 as a diagnostic marker of malignant transformation was considered keeping tobacco associated and degree of dysplasia into consideration. A significant correlation has been demonstrated between the IL-8 and IL-6 levels in serum and saliva [22]. In this context, it has been found that the IL-6 level in saliva was three to four times more than that in serum.
The saliva-based evaluation of IL-6 in our series showed that all the leukoplakia patients with coexisting periodontitis had higher IL-6 levels when compared with saliva of patients with periodontitis alone. This finding of elevated IL-6 in saliva is supported by a similar study carried out by Brailo et al. [12]. The elevated salivary IL-6 level in their observations was independent of any tobacco habit, unlike our findings where we noted a direct correlation between IL-6 and tobacco habits, implying that tobacco did play a significant role in IL-6 elevation. The NF-κB-dependent cytokines are elevated as a result of localized production from at least two sources, either by the lesional epithelium itself or by the activated T lymphocytes present in the connective tissue affected with leukoplakia. Besides that, it is also known that oral epithelial cells are able to secrete IL-6 as a response to various microbial and chemical stimuli [23, 24].
Our study showed a sequential increase in IL-6 level from mild to severe dysplasia. These findings are in agreement with another report by Rhodus et al. [21] who demonstrated that IL-6 was increased in mild, moderate, and severe dysplasia compared to controls but not as much when compared with OSCC. It has also been suggested that an increase in both the systemic and local IL-6 level correlates with the growth of oral carcinomas [25]. The increased levels related to the clinical stage of the disease seemed to be the most sensitive parameter, particularly in the early stages of oral cancer. These cytokines and their transcripts were localized in stromal macrophages and in the tumor cells, particularly in the tumor front, indicating active synthesis of these cytokines by tumor cells [26].
All the patients with leukoplakia in our study had coexisting periodontitis as it was not possible to exclude this feature due to the demographic profile of our patients. This inclusion was distinct, in contrast to Brailo et al. [12] who excluded patients with periodontitis. It is perhaps because of this inflammatory component in periodontitis, in addition to the dysplastic epithelium of leukoplakia, that the IL-6 level noted in our series was greater than that previously reported in literature.
IL-6 as a multifunctional cytokine binds to a heterodimeric receptor, which contains the ligand-binding IL-6α chain and the common cytokine receptor signal-transducing subunit gp130 [27]. IL-6 receptor engagement leads to activation of the JAK family of tyrosine kinases, which then stimulate multiple pathways involving MAPKs, PI3Ks, STATs, and other signaling proteins [28]. Various subcomponents of these pathways have been implicated in influencing the carcinogenic cascade in various cancers including OSCC and premalignant oral lesions [29–31].
IL-6 expression has shown to be induced by the transcription factor NF-κB under hypoxic conditions [32]. It has been shown that the presence of hypoxia is correlated with aggressive tumor growth and poor patient prognosis [33]. This detrimental effect of hypoxia has been attributed to an increase in the level of hypoxia inducible factor-1α. The latter one is mediated through the downstream signaling element of IL-6 pathway—the STAT3 [34]. STAT3 regulates G1 to S cell-cycle progression as well as the prevention of apoptosis through c-Myc, Pim-family proteins, valosine containing protein, and Bcl-family proteins [35]. Thus, the IL-6/gp130/STAT3 axis has been implicated in playing a crucial role in the sequential change from hyperplasia to neoplasia [36, 37].
The change from a paracrine to an autocrine mode of IL-6 signaling is believed to be a key contributing factor in the progression from benign hyperplasia to neoplasia and cancer as reported in several studies [29, 37–40]. Perhaps, increasingly amplified amounts of IL-6, produced by autocrine stimulation, is able to overcome p53 inhibition through the hypermethylation of its promoter [41], and this may well be the point in discussion for elevated IL-6 seen in our series of patients with leukoplakia.
It has been reported that wild-type p53 and Rb repress the promoter of the IL-6 gene [42]. The reciprocal is also true, namely that IL-6 suppresses the activation of p53 [43] and Rb genes. Thus, the balance that is tilted in favor of the p53 and Rb probably keeps tabs on the uncontrolled proliferation of keratinocytes. While autocrine IL-6 production by tumor cells maintains this hypermethylation, withdrawal of IL-6 leads to reversal of methylation of p53 promoter and its subsequent reactivation, with resultant suppression of keratinocyte proliferation [41]. Autocrine IL-6 signaling has thus been implicated as a key event in carcinogenesis [44] and also drug resistance [45].
As expected, elevated IL-6 levels were found in patients with periodontitis alone without leukoplakia, although it was increased to a lesser extent when compared to patients with both leukoplakia and periodontitis. Large numbers of gram-negative periodontopathic bacteria present in the subgingival plaque may seem to be the most obvious cause for this increase. As these bacteria do not invade the periodontium in appreciable numbers, their solubilized components diffuse into periodontal tissues including the epithelium, thereby providing the stimulus for cytokine production. These soluble bacterial components act on a family of membrane bound receptors called toll-like receptors leading to subsequent activation of the NF-κB pathway, which results in inflammatory cytokine gene transcription and leads to the production of IL-6 and other cytokines [46].
Various studies have shown that the cytokine-rich oral cavity in periodontal disease may contribute to accelerated carcinogenesis [47, 48]. These studies suggest that chronic periodontitis is an independent risk factor for HNSCC and smoking modifies this association [49]. This association was particularly significant in our study, considering the demographics and the increased incidence of oral cancer in the subcontinent.
Significant differences in the concentration of salivary IL-6 between tobacco users and non users in both the study group as well as in control group have been demonstrated by Zhang et al. [50], who reported higher systemic level of IL-6 as a consequence of passive smoking in animal models. Erdemir et al. [51] on the other hand have reported no influence of smoking on IL-6 level in gingival crevicular fluid. The influence of tobacco on IL-6 is attributed to an interaction of the released tobacco products with keratinocytes [23, 52]. Nicotine from tobacco smoke and lipopolysaccharide from bacterial infection may also synergistically enhance IL-6 production in patients with periodontitis [53].
In our study, we found that leukoplakia, periodontitis, and tobacco habits contributed to an elevated IL-6 level. Our observation thus confirms and extends the previous findings that IL-6 expression could be used as a specific marker for lesions that are at high risk of malignant transformation. Our findings also support the recently proposed hypothesis that periodontitis may be a significant contributing risk factor for oral cancer. The study, however, has the limitation of not including female subjects and diet being a confounder. Large multicenter trials are deemed necessary to establish the role of interleukin in the pathogenesis of tobacco associated OPMD.
References
Amarasinghe HK, Usgodaarachchi US, Johnson NW, Lalloo R, Warnakulasuriya S (2010) Betel-quid chewing with or without tobacco is a major risk factor for oral potentially malignant disorders in Sri Lanka: a case-control study. Oral Oncol 46:297–301
Harris CK, Warnakulasuriya KA, Cooper DJ, Peters TJ, Gelbier S (2004) Prevalence of oral mucosal lesions in alcohol misusers in south London. J Oral Pathol Med 33:253–259
Scully C, Field JK, Tanzawa H (2000) Genetic aberrations in oral or head and neck squamous cell carcinoma (SCCHN): 1. Carcinogen metabolism, DNA repair and cell cycle control. Oral Oncol 36:256–263
Day GL, Blot WJ, Austin DF, Bernstein L, Greenberg RS, Preston-Martin S, Schoenberg JB, Winn DM, McLaughlin JK, Fraumeni JF Jr (1993) Racial differences in risk of oral and pharyngeal cancer: alcohol, tobacco, and other determinants. J Natl Cancer Inst 85:465
Warnakulasuriya S, Johnson NW, van der Waal I (2007) Nomenclature and classification of potentially malignant disorders of the oral mucosa. J Oral Pathol Med 36:575–580
Banoczy J, Csiba A (1976) Occurrence of epithelial dysplasia in oral leukoplakia. Oral Surg Oral Med Oral Pathol 42:766–774
Gupta PC, Mehta FS, Daftary DK, Pindborg JJ, Bhonsle RB, Jalnawalla PN, Sinor PN, Pitkar VK, Murti PR, Irani RR, Shah HT, Kadam PM, Iyer KS, Iyer HM, Hegde AK, Chandrashekar GK, Shiroff BC, Sahiar BE, Mehta MN (1980) Incidence rates of oral cancer and natural history of oral precancerous lesions in a 10-year follow-up study of Indian villagers. Community Dent Oral Epidemiol 8:283–333
Silverman S Jr, Gorsky M, Lozada F (1984) Oral leukoplakia and malignant transformation. A follow-up study of 257 patients. Cancer 53:563–568
De Schutter H, Landuyt W, Verbeken E, Goethals L, Hermans R, Nuyts S (2005) The prognostic value of the hypoxia markers CA IX and GLUT 1 and the cytokines VEGF and IL 6 in head and neck squamous cell carcinoma treated by radiotherapy ± chemotherapy. BMC Cancer 5:42
Lumerman H, Freedman P, Kerpel S (1995) Oral epithelial dysplasia and the development of invasive squamous cell carcinoma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 79:321–329
World Health Organization (1997) Oral health surveys. Basic methods. World Health Organization, Geneva
Brailo V, Vucićević-Boras V, Cekić-Arambasin A, Alajbeg IZ, Milenović A, Lukac J (2006) The significance of salivary interleukin 6 and tumor necrosis factor alpha in patients with oral leukoplakia. Oral Oncol 42:370–373
Navazesh M, Kumar SK, University of Southern California School of Dentistry (2008) Measuring salivary flow: challenges and opportunities. J Am Dent Assoc 139(Suppl):35S–40S
Ng PY, Donley M, Hausmann E, Hutson AD, Rossomando EF, Scannapieco FA (2007) Candidate salivary biomarkers associated with alveolar bone loss: cross-sectional and in vitro studies. FEMS Immunol Med Microbiol 49:252–260
Ferguson DB (1987) Current diagnostic uses of saliva. J Dent Res 66:420–424
Streckfus CF, Bigler LR (2002) Saliva as a diagnostic fluid. Oral Dis 8:69–76
Zimmermann BG, Wong DT (2008) Salivary mRNA targets for cancer diagnostics. Oral Oncol 44:425–429
Wang PL, Ohura K, Fujii T, Oido-Mori M, Kowashi Y, Kikuchi M, Suetsugu Y, Tanaka J (2003) DNA microarray analysis of human gingival fibroblasts from healthy and inflammatory gingival tissues. Biochem Biophys Res Commun 305:970–973
Liao WC, Lin JT, Wu CY, Huang SP, Lin MT, Wu AS, Huang YJ, Wu MS (2008) Serum interleukin-6 level but not genotype predicts survival after resection in stages II and III gastric carcinoma. Clin Cancer Res 14:428–434
Bigbee WL, Grandis JR, Siegfried JM (2007) Multiple cytokine and growth factor serum biomarkers predict therapeutic response and survival in advanced-stage head and neck cancer patients. Clin Cancer Res 13:3107–3108
Rhodus NL, Ho V, Miller CS, Myers S, Ondrey F (2005) NF-kappa B dependent cytokine levels in saliva of patients with oral preneoplastic lesions and oral squamous cell carcinoma. Cancer Detect Prev 29:42–45
St John MA, Li Y, Zhou X, Denny P, Ho CM, Montemagno C, Shi W, Qi F, Wu B, Sinha U, Jordan R, Wolinsky L, Park NH, Liu H, Abemayor E, Wong DT (2004) Interleukin 6 and interleukin 8 as potential biomarkers for oral cavity and oropharyngeal squamous cell carcinoma. Arch Otolaryngol Head Neck Surg 130:929–935
Chang MC, Wu HL, Lee JJ, Lee PH, Chang HH, Hahn LJ, Lin BR, Chen YJ, Jeng JH (2004) The induction of prostaglandin E2 production, interleukin-6 production, cell cycle arrest, and cytotoxicity in primary oral keratinocytes and KB cancer cells by areca nut ingredients is differentially regulated by MEK/ERK activation. J Biol Chem 279:50676–50683
Johnson GK, Poore TK, Squier CA, Wertz PW, Reinhardt RA, Vincent SD (1994) Prostaglandin E2 and interleukin 1 levels in smokeless tobacco-induced oral mucosal lesions. J Periodontal Res 29:430–438
Jablonska E, Piotrowski L, Grabowska Z (1997) Serum levels of IL-1β, IL-6, TNF-α, TNF-R1 and CRP in patients with oral cavity cancer. Pathol Oncol Res 3:126–129
Nakano Y, Kobayashi W, Sugai S, Kimura H, Yagihashi S (1999) Expression of tumor necrosis factor-α and interleukin 6 in oral squamous cell carcinoma. Jpn J Cancer Res 90:858–866
Schafer ZT, Brugge JS (2007) IL-6 involvement in epithelial cancers. J Clin Invest 117:3660–3663
Hong DS, Angelo LS, Kurzrock R (2007) Interleukin-6 and its receptor in cancer: implications for translational therapeutics. Cancer 110:1911–1928
Sansone P, Storci G, Tavolari S, Guarnieri T, Giovannini C, Taffurelli M, Ceccarelli C, Santini D, Paterini P, Marcu KB, Chieco P, Bonafè M (2007) IL-6 triggers malignant features in mammospheres from human ductal breast carcinoma and normal mammary gland. J Clin Invest 117:3988–4002
Wu HT, Ko SY, Fong JH, Chang KW, Liu TY, Kao SY (2009) Expression of phosphorylated Akt in oral carcinogenesis and its induction by nicotine and alkaline stimulation. J Oral Pathol Med 38:206–213
Søland TM, Husvik C, Koppang HS, Boysen M, Sandvik L, Clausen OP, Christoffersen T, Bryne M (2008) A study of phosphorylated ERK1/2 and COX-2 in early stage (T1–T2) oral squamous cell carcinomas. J Oral Pathol Med 37:535–542
Muraoka K, Shimizu K, Sun X, Zhang YK, Tani T, Hashimoto T, Yagi M, Miyazaki I, Yamamoto K (1997) Hypoxia, but not reoxygenation, induces interleukin 6 gene expression through NF-kappa B activation. Transplantation 63:466–470
Powis G, Kirkpatrick L (2004) Hypoxia inducible factor-1alpha as a cancer drug target. Mol Cancer Ther 3:647–654
Niu G, Briggs J, Deng J, Ma Y, Lee H, Kortylewski M, Kujawski M, Kay H, Cress WD, Jove R, Yu H (2008) Signal transducer and activator of transcription 3 is required for hypoxia-inducible factor-1alpha RNA expression in both tumor cells and tumor-associated myeloid cells. Mol Cancer Res 6:1099–1105
Shirogane T, Fukada T, Muller JM, Shima DT, Hibi M, Hirano T (1999) Synergistic roles for Pim-1 and c-Myc in STAT3-mediated cell cycle progression and antiapoptosis. Immunity 11:709–719
Hirano T, Ishihara K, Hibi M (2000) Roles of STAT3 in mediating the cell growth, differentiation and survival signals relayed through the IL-6 family of cytokine receptors. Oncogene 19:2548–2556
Barton BE, Murphy TF, Adem P, Watson RA, Irwin RJ, Huang HF (2001) IL-6 signalling by STAT3 participates in the change from hyperplasia to neoplasia in NRP-152 and NRP-154 rat prostatic epithelial cells. BMC Cancer 1:19
Grivennikov S, Karin M (2008) Autocrine IL-6 signaling: a key event in tumorigenesis? Cancer Cell 13:7–9
Gao SP, Mark KG, Leslie K, Pao W, Motoi N, Gerald WL, Travis WD, Bornmann W, Veach D, Clarkson B, Bromberg JF (2007) Mutations in the EGFR kinase domain mediate STAT3 activation via IL-6 production in human lung adenocarcinomas. J Clin Invest 117:3846–3856
Sriuranpong V, Park JI, Amornphimoltham P, Patel V, Nelkin BD, Gutkind JS (2003) Epidermal growth factor receptor-independent constitutive activation of STAT3 in head and neck squamous cell carcinoma is mediated by the autocrine/paracrine stimulation of the interleukin 6/gp130 cytokine system. Cancer Res 63:2948–2956
Hodge DR, Peng B, Cherry JC, Hurt EM, Fox SD, Kelley JA, Munroe DJ, Farrar WL (2005) Interleukin 6 supports the maintenance of p53 tumor suppressor gene promoter methylation. Cancer Res 65:4673–4682
Resnitzky D, Tiefenbrun N, Berissi H, Kimchi A (1992) Interferons and interleukin-6 suppress phosphorylation of the retinoblastoma protein in growth-sensitive hematopoietic cells. Proc Natl Acad Sci U S A 89:402–406
Santhanam U, Ray A, Sehgal PB (1991) Repression of the interleukin 6 gene promoter by p53 and the retinoblastoma susceptibility gene product. Proc Natl Acad Sci U S A 88:7605–7609
Angelo LS, Talpaz M, Kurzrock R (2002) Autocrine interleukin-6 production in renal cell carcinoma: evidence for the involvement of p53. Cancer Res 62:932–940
Conze D, Weiss L, Regen PS, Bhushan A, Weaver D, Johnson P, Rincón M (2001) Autocrine production of interleukin 6 causes multidrug resistance in breast cancer cells. Cancer Res 61:8851–8858
Beklen A, Hukkanen M, Richardson R, Konttinen YT (2008) Immunohistochemical localization of Toll-like receptors 1–10 in periodontitis. Oral Microbiol Immunol 23:425–431
Hong SH, Ondrey FG, Avis IM, Chen Z, Loukinova E, Cavanaugh PF Jr, Van Waes C, Mulshine JL (2000) Cyclooxygenase regulates human oropharyngeal carcinomas via the proinflammatory cytokine IL-6: a general role for inflammation? FASEB J 14:1499–1507
Tezal M, Sullivan MA, Reid ME, Marshall JR, Hyland A, Loree T, Lillis C, Hauck L, Wactawski-Wende J, Scannapieco FA (2007) Chronic periodontitis and the risk of tongue cancer. Arch Otolaryngol Head Neck Surg 133:450–454
Tezal M, Sullivan MA, Hyland A, Marshall JR, Stoler D, Reid ME, Loree TR, Rigual NR, Merzianu M, Hauck L, Lillis C, Wactawski-Wende J, Scannapieco FA (2009) Chronic periodontitis and the incidence of head and neck squamous cell carcinoma. Cancer Epidemiol Biomarkers Prev 18:2406–2412
Zhang J, Liu Y, Shi J, Larson DF, Watson RR (2002) Side stream cigarette smoke induces dose response in systemic inflammatory cytokine production and oxidative stress. Exp Biol Med (Maywood) 227:823–829
Erdemir EO, Duran I, Haliloglu S (2004) Effects of smoking on clinical parameters and the gingival crevicular fluid levels of IL-6 and TNF-α in patients with chronic periodontitis. J Clin Periodontol 31:99–104
Jeng JH, Wang YJ, Chiang BL, Lee PH, Chan CP, Ho YS, Wang TM, Lee JJ, Hahn LJ, Chang MC (2003) Roles of keratinocyte inflammation in oral cancer: regulating the prostaglandin E2, interleukin-6 and TNF-alpha production of oral epithelial cells by areca nut extract and arecoline. Carcinogenesis 24:1301–1315
Wendell KJ, Stein SH (2001) Regulation of cytokine production in human gingival fibroblasts following treatment with nicotine and lipopolysaccharide. J Periodontol 72:1038–1044
Acknowledgment
This work was supported by a grant from Manipal University, Manipal and generous support from the Department of Microbiology, Kasturba Manipal for the use of laboratory consumables.
Conflict of interest statement
The authors of the manuscript titled “Salivary IL-6 levels in oral leukoplakia with dysplasia and its clinical relevance to tobacco habits and periodontitis” hereby declare that no financial or any personal relationship with other individuals or organization has influenced the outcome of this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sharma, M., Bairy, I., Pai, K. et al. Salivary IL-6 levels in oral leukoplakia with dysplasia and its clinical relevance to tobacco habits and periodontitis. Clin Oral Invest 15, 705–714 (2011). https://doi.org/10.1007/s00784-010-0435-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-010-0435-5