Abstract
The vascularity of the implant bed is a very important parameter in both bone formation and maintenance after dental implants insertion. The relationship between bone and vessels network organization is still unknown. The aim of this study was to investigate the three-dimensional bone vascular canals of the peri-implant bone after loading. A total of ten implants with sandblasted and acid-etched surface were placed in the mandible of a beagle dog. Three months later, the implants were connected and loaded. The dog was killed after 12 months. The specimens were embedded and processed for scanning electron microscopy (SEM) analysis. After a 1-year loading period, a very intricate vessel network could be seen around the implants. The vessels, with neighbouring soft tissues, were round in shape and showed a lot of anastomoses with a mesh-like appearance. They ran circularly around the dental implant. In the bone, the majority of the vessels appeared to ran parallel to the mandibular canal. After a 1-year loading period, the peri-implant bone vasculature looked like a mesh that surrounded the implants. Nevertheless, the presence of many thick vessels inside the peri-implant crestal bone indicates a high metabolic need and also a different bone organization, as no osteons were noted. The crater-like bone loss around the marginal part of the implant could be related to the microvasculature “strain”. A high strain level could continuously activate the osteocyte–vessel syncytium, producing a net bone loss.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bone loss around dental implants may result from several factors. As reported in dental literature, implant design, density of bone, surgical trauma, occlusal overload, establishing of an appropriate biological width, development of a pathogenic bacterial biofilm, and, lastly, blood supply interruption are all the factors involved [15, 21, 23, 24, 32, 33, 38, 39]. After implant bed preparation and implant insertion, tissue repair requires the development of a vascular system at the site of injury for the delivery of oxygen and nutrients and to take away cell debris for a complete healing process [5]. Furthermore, after healing, the bone tissue remodeling needs to induce neoangiogenesis. Neoangiogenesis is promoted and regulated through a complex action of molecular signals mediated by, in part, unknown growth factors [37]. Blood vessel growth can be categorized into angiogenesis and arteriogenesis [37]. Angiogenesis is the growth of blood vessels occurring in an adult through migration and proliferation of endothelial cells, while arteriogenesis is the expansion or branching of an existing vessel through arteriolar connections to form larger collateral vessels. These processes produce vessels of different sizes and different functional capabilities. Both arterioles and venules are important components of bone for formation and maintenance of the tissue [13, 26]. Moreover, loss of microvasculature has been implicated in several disorders comprising bone loss [31]. Cortical bone is vascularized through the Haversian canal system as well as by Volkmann’s canals, while trabecular bone is ten times more vascularized through marrow’s vessels which allow nutrients and cytokine signals to reach the osteocytes and osteoblasts cells. Bone tissue is a rich source of angiogenic growth factors such as fibroblast growth factor and transforming growth factor-â, as well as of osteogenic growth factors such as bone morphogenetic proteins. These developmentally important cytokines play a role in osteogenesis and angiogenesis [31, 36]. During bone healing, calcification of the hematoma is the first stage of tissue regeneration and bone is formed by repetitive revascularization and mineralization. To evaluate and study the vascular architecture of the bone tissue, several methods have been used. Albrektsson [3, 4] reported the use of intravital microscopy to assess the vascular architecture and microcirculation of grafted bone tissue in a rabbit model. Berglund et al. [10] used the India ink method to evaluate the vessels in the peri-implant bone, while Kishi and Yakahashi [24] used the microvascular resin cast to asses the three-dimensional vascular architecture. Matsuo and Takahashi [29], in a dog study, reported that, in the cervical region of the machined implants, the vessels were arranged horizontally toward the fixture forming vascular loops. The vessels were flat and the diameters ranged from 30 to 80 μm. The resin cast corrosion technique is able to reproduce very well the endoluminal morphology of the vessels until the nucleus impressions of endothelial cells and also veins valve could be distinguished. A lot of information could be drawn from these procedures after dissolving the peripheral tissue with acid solutions and proteinase as the resin cast network representing the lumen vessels [30]. All these methods of investigation, nevertheless, must be performed in animal models as they need to inject a material into the lumen vessels before killing the animal. The limitation of this technique is due to the necessity of vascular perfusion in living animals and also the loss of information about perivessel tissue. Because the bone vessels that ran inside bone canals surrounded by cells and tissue forms with the osteocyte network a “functional syncytium”, it was argued that this syncytium of cells with pericellular fluid are particularly important for bone maintenance, as the level of bone strain is recognized by canalicular fluid flow through the canaliculi [28, 41]. In concept, bone fluid serves as coupling medium through which energy is transferred from the system to the cells that have the machinery to remodel the tissue. The bone interstitial fluid is provided by transudation from the blood supply following Starling mechanism and is related to the pressure gradients generated by both venous and intramedullary pressures and osmotic gradients. The vascular system through the blood flows is an important component of the mechano-trasduction system. The present study was undertaken to describe the vasculature organization of loaded peri-implant bone using new methods based on fixed specimens infiltrated with resin.
Materials and methods
Sandblasted and acid-etched titanium dental implants (Bone System, Milano, Italy) 4.0×10 mm were placed in the mandible of a male beagle dog 18 months of age. The protocol was approved by the Ethics Committee of the University of Madrid, Spain. The two premolars and the first molars had been extracted 3 months previously. The dog received ten implants in the mandible (five on the right side and five on the left side); the interimplant distance was 3 mm. All surgical procedures were performed under general anesthesia (premedication with acepromazine 0.5 mg/kg administered subcutaneously; anesthesia with nembutal at 15 mg/kg administered intravenously) and antibiotic prophylaxis. The implant sites were prepared with drills under generously chilled saline irrigation. The implants were then inserted with a tapping instrument. The mucosal tissues were sutured with 30 silk sutures. In the first two postsurgical weeks, the oral cavities were rinsed daily with chlorexidinedigluconate 0.2% (Peridex, Procter & Gamble, Cincinnati, OH, USA). In addition, the dog was fed a soft diet. The sutures were removed after 1 week. An oral hygiene regimen was instituted consisting of plaque removal three times a week with a soft toothbrush and 0.12% chlorexidine. Three months after implantation, second-stage surgery was performed for abutment connection and prosthetic application. The dog was killed after 12 months.
Special processing for specimens
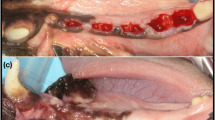
After retrieval, all the specimens were immediately fixed using a 10% buffered formalin solution. The specimens were dehydrated in an ascending series of alcohol rinses and embedded in a glycolmethacrylate resin (Technovit 7200 VLC, Kulzer, Wehrheim, Germany). After polymerization, each infiltrated block containing one osseointegrated implant was cut into two halves longitudinally along the major axis of the implant in vestibule–buccal direction using the Precise 1 Automated System (Assing, Rome, Italy) [34]. All the samples were etched with 0.1 N HCL for 24 h, treated with trypsin (80 U/ml, pH 7.4 at 39°C for 48 h. By this way, the mineralized matrix was degraded and the vessels, the cells, and the tissue around vessels remained as these structures were infiltrated by resin so they did not dissolve and could be seen. The method was particularly useful because, by this technique, all the vessels could be seen also in human samples while, using the classical resin cast method, only an evaluation of the internal structure of the vessels in animal models could be made [14, 17]. The prepared specimens were than coated with a thin layer of gold by vacuum evaporation Emitech K 550 (Emitech, Ashford, Kent, UK) and placed on the storage of a SEM (LEO 435 Vp, LEO Electron Microscopy Ltd, Cambridge, UK) for evaluation.
Results
The implants showed a high level of bone-to-implant contact percentage (BIC=80.4±2.6%) (Fig. 1). No connective soft tissue was detected at the bone-to-implant interface. The majority of the bone contacting the implants appeared mature. Several Haversian systems were identified in the compact bone that was the most vascular area. In general, the alveolar crest was rounded and separated from the implant surface by a shallow groove rich in 70- to 120-μm blood vessels (Fig. 2). Apical to the groove, the bone appeared to be in direct contact with the implant surface with a large amount of network of bone canals of 10- to 70-μm in diameter (Figs. 3, 4, 5, 6, and 7). When the implant fragment was removed, an intricate vessel network looking like a mesh appeared to run circularly around the implant body (Fig. 8). At higher magnification, the network vessels appeared to be composed of thick vessels connected to same marrow space (Fig. 9). The bone, at a distance of 7 mm from the implant surface, showed only a few thick vessels embedded in marrow tissue with a large number of thin-vessels anastomoses (Fig. 10). The blood canal structures inside the bone tissue were always associated with the osteocytic syncytium (Fig. 11).
Discussion
It is evident that implants that are properly installed and loaded can function for periods of up to 20 years or more as abutments for fixed restorations or as fixed supports for removable prosthetic restorations [27]. In the mandible between the mental foramina, more than a 95% 5-year success rate could be expected with modern oral implant devices [2]. The long-term success of oral implants is certainly dependent on a direct bone-to-implant contact in sufficient portions of the implant to achieve the so-called ossoeintegration. Adell et al. [1] proposed a concept that bone loss after loading was related to the transition ‘bone strain ∅ remodeling of bone’ until an equilibrium was obtained one to several years after loading. A more intensive remodeling in the early period of loading was also reported in an animal study using IMZ implants [7]. A long-term stable bone level has been reported for the Branemark animal models [20]; furthermore, analytical models and finite element analysis were also used to investigate the correlation between overload and bone breakdown, eventually leading to implant failure, and a possible mechanism of overload by positive feedback was suggested [11, 12]. Dynamic excessive loads perpendicular to the implant axis were shown to cause crater-like bone loss around the marginal part of the implant, while moderate static loads did not result in bone change [18]. Higher remodeling activity under uniaxial than axial loads was reported in animal models [14, 40]. All the reported studies have correlated bone response to a simple reaction to loading state without considering vasculature. The study by Matsuo et al. [30] in an animal model reported only developmental considerations about microvasculature architecture near dental implants with different surfaces. Barou et al. [8], in a rat study, suggested a functional link between bone remodeling rate and vessel area. The authors suggested also a functional link between vessel osteoblastic and osteoclastic activities. Osteoblasts are metabolically demanding cells with high levels of energy consumption and, therefore, require an adequate blood supply. Osteoclasts, on the other hand, when actively resorbing bone are influenced by local blood flow. Hypoxia is a strong stimulus for the formation of new capillaries and the recruitment of endothelial progenitors, as oxygen was considered a repellent of vascular patterning [16]. Hypoxia also induces the transcription of several factors that turn on the expression of angiogenic genes such as vascular endothelial growth factor (VEGF), inducing vessels to branch towards the hypoxic tissue [35]. There was evidence that bone vascularization and vascular-derived factors may play an important role in coordinating the activities of bone cells, which in turn could influence vessel cells behavior [17]. Bone sialoprotein synthesized by osteoblast mediates human endothelial cell attachment and migration and promotes angiogenesis in vitro [9]. In the growing bone site, both osteoblast and osteoclast cells expressed VEGF [22]. Intraosseous blood flow gives life to bone [25]. The intracortical vessels travel in canals located within the cortex, mainly Havers canals and secondarily Volkmann’s canals while, into the cancellous bone, the vessels mainly ran inside the medullary spaces. Bone should be considered a porous tissue containing a solid matrix, cells, and a fluid phase. The solid matrix contributes to determine the biomechanical properties of bone. The cells provide the machinery for modeling and remodeling, allowing for adaptation of bone structure to functional demands. The fluid phase within lacunocanalicular system appear to be able to interconnect the cellular “syncytium” to the load–strain level of the bone. The development and the maintenance of good level of osseointegration for dental implants are certainly related to a well-developed bone vascular network in the peri-implant bone. Several factors may influence the peri-implant vasculature. These could be divided into the following: surgery-, host-, implant-, and occlusion-related factors. Surgery-related factors are involved for: the primary stability that is important to elude the fibrous encapsulation which is rich of vessels, the surgical technique that must be “gentle” to avoid bone necrosis or micro-fracture which is able to stimulate neoangiogenesis. Host-related factors are involved for: the bone quality and quantity that influence the extension of the vessel supply due to cortical and medullary bone, the wound healing that is directly affected by metabolic diseases. Implant-related factors are involved for: implant design, implant surface. Occlusion-related factors are involved for: quality and quantity of the load, prosthetic design. In the present study, to standardize all the variables related to bone quantity and quality, we considered an animal model (dog). The implants were placed only in the bone mandible as it is osteonal. This specific environment let us to consider the results interesting in terms of relation between implant placement, loading, and bone adaptation. In fact, near the implant surface, at the crestal level, the high number of vessels and the paucity of space among them demonstrate a high metabolic demand and also a scarce microstructural bone organization. To have a highly organized osteonal bone, the vessels should be far from each other by at least 200 μm as the osteons have a diameter of 200–300 μm. Blood supply in the peri-implant bone is entirely dependent on the arterioles and venules housed within the mineralized tissue; this aspect places the bone blood supply network in a low compliance environment. During inflammation, the microvasculature dilates and becomes filled with blood. This process is known as active hyperemia and, when this happens in a soft tissue, swelling can occur to accommodate the blood flow by both vasodilatation and eventually tissue edema. The bone vessels are unable to completely swell, producing an increase of vascular resistance, and ischemic necrosis could be produced either by occlusion of the arterial supply or venous drainage [6]. Ficat and Arlet [19] found convincing evidence that intraosseous circulation was abnormal in hip osteonecrosis. In the present study, the anatomical aspects of bone vascular canals were correlated to the loading state. The results obtained showed a peri-implant microvasculature as well developed after 1 year of loading. The peri-implant crestal bone loss certainly is not only associated to the microvasculature for cells and metabolic supply but should be also related to the ability of strain detection as the bone in these areas was not organized to best resist to stress concentration. A high strain level could continuously activate the osteocyte vessel syncytium, producing a net bone loss.
References
Adell R, Lekholm U, Rockler B, Branemark PI, Lindhe J, Eriksson B, Sbordone L (1986) Marginal tissue reactions at osseointegrated titanium fixtures (I). A 3-year longitudinal prospective study. Int J Oral Maxillofac Surg 15:39–52
Albrektsson T, Sennerby L (1991) State of the art in oral implants. J Clin Periodontol 18:474–481
Albrektsson T (1980) Repair of bone grafts. A vital microscopic and histological investigation in the rabbit. Scand J Plast Reconstr Surg 14:1–12
Albrektsson T, Albrektsson B (1978) Microcirculation in grafted bone. A chamber technique for vital microscopy of rabbit bone transplants. Acta Orthop Scand 49:1–7
Arnold F, West DC (1991) Angiogenesis in wound healing. Pharmacol Ther 52:407–422
Atsumi T, Kuroki Y (1987) Vascular changes of idiopathic necrosis of the femoral head. In: Arlet J, Mazieres B (eds) Bone circulation and bone necrosis. Springer, Berlin Heidelberg New York, pp 311–317
Barbier L, Schepers E (1997) Adaptive bone remodeling around oral implants under axial and nonaxial loading conditions in the dog mandible. Int J Oral Maxillofac Implants 12:215–223
Barou O, Mekraldi S, Vico L, Boivin G, Alexandre C, Lafage Proust MH (2002) Relationships between trabecular bone remodeling and bone vascularization: a quantitative study. Bone 30:604–612
Bellahcene A, Bonjean K, Fhor B, Fedarkon S, Robey FA, Young MF, Fisher LW, Castronovo V (2000) Bone sialoprotein mediates human endothelial cell attachment and migration and promotes angiogenesis. Circ Res 86:885–891
Berglund T, Lindhe J, Jonsson K, Ericsson I (1994) The topology of the vascular systems in the periodontal and periimplant tissues in the dog. J Clin Periodontol 21:189–193
Brunski JB (1999) In vivo bone response to biomechanical loading at the bone/dental implant interface. Adv Dent Res 13:99–119
Brunski JB (2003) Biomechanical aspects of oral/maxillofacial implants. Int J Prosthodont 16:30–32
Burgess EA, Hollinger JO (1998) Options for engineering bone. In: Patrick CW Jr, Mikos AG, McIntire LV (eds) Frontiers in tissue engineering. Elsevier, New York, pp 369–399
Buser D, Belser UC, Lang NP (1998) The original one-stage dental implant system and its clinical application. Periodontol 2000 17:106–118
Callan D, O’Mahony A, Cobb CM (1998) Loss of crestal bone around dental implants: a retrospective study. Implant Dent 7:258–266
Carmeliet P (2004) Manipulating angiogenesis in medicine. J Intern Med 255:538–561
Collin Osbody P (1994) Role of vascular endothelial cells in bone biology. J Cell Biochem 55:304–309
Duyck J, Ronold HJ, Van Oosterwyck H, Naert I, Vander Sloten J, Ellingsen JE (2001) The influence of static and dynamic loading on marginal bone reactions around osseointegrated implants: an animal experimental study. Clin Oral Implants Res 12:207–218
Ficat P Arlet J (1977) Pathogenies des osteonecroses in ischemie et necroses. Masson, Paris, pp 190–195
Goodacre CJ, Kan JYK, Rungcharassaeng K (1999) Clinical complications of osseointegrated implants. J Prosthet Dent 81:537–552
Hermann JS, Cochran DL, Nummikoski PV, Buser D (1997) Crestal bone changes around titanium implants: a radiographic evaluation of unloaded nonsubmerged and submerged implants in the canine mandible. J Periodontol 68:1117–1130
Horner A, Bord S, Kelsall AW, Coleman N, Compston JE (2001) Tie 2 ligands angioprotein1 and angioprotein2 are coexpressed with vascular endothelial cell growth factor in growing human bone. Bone 28:65–71
Hoshaw SJ, Brunski JB, Cochran GVB (1994) Mechanical loading of Branemark implants affects interfacial modeling and remodeling. Int J Oral Maxillofac Implants 9:345–360
Kishi Y, Yakahashi K (1977) A scanning electron microscopic study of the vascular architecture of the periodontal membrane. Shika Kiso Igakkai Zasshi 19:192–207
Laroche M (2002) Intraosseous circulation from physiology to disease. Jt Bone Spine 69:262–269
Leunig M, Yuan F, Berk DA, Gerweck LE, Jain RK (1994) Angiogenesis and growth of isografted bone: quantitative in vivo assay in nude mice. Lab Invest 71:300–307
Listgarten MA, Lang NP, Schroeder HE, Schroeder A (1991) Periodontal tissues and their counterparts around endosseous implants. Clin Oral Implants Res 2:1–19
Mak AFT, Huang DT, Zhang JD, Tong P (1997) Deformation induced hierarchical flows and drag forces in bone canaliculi and matrix porosity. J Biomech 30:11–18
Matsuo M, Takahashi K (2002) Scanning electron microscopic observation of microvasculature in periodontium. Microsc Res Tech 56:3–14
Matsuo M, NakamuraT, KishiY, Takahashi K (1999) Microvascular changes after placement of titanium implants: scaning electron microscopy observations of machined and titanium plasma-sprayed implants in dogs. J Periodontol 70:1330–1338
Meyer M, Clauss M, Lepple Wienhues A, Waltenberger J, Augustin HG, Ziche M, Lanz C, Buttner M, Rziha HJ, Dehio C (1999) A novel vascular endothelial growth factor encoded by ORF virus, VEGFE mediates angiogenesis via signalling through VEGFR2 (KDR) but not VEGF1 (FLT1) receptor tyrosine kinases. EMBO J 18:363–374
Misch CE, Bidez MW, Sharawy M (2001) A bioengineered implant for a predetermined bone cellular response to loading forces. A literature review. J Periodontol 72:1276–1286
O’Mahony A, Bowles Q, Woolsey G, Robinson SJ, Spencer P (2000) Stress distribution in the single unit osseointegrated dental implant: finite element analyses of axial and nonaxial loading. Implant Dent 9:207–218
Piattelli A, Scarano A, Quaranta M (1997) High-precision cost-effective system for producing thin sections of oral tissues containing dental implants. Biomaterials 18:577–579
Pugh CW, Ratcliffe PJ (2003) Regulation of angiogenesis by hypoxia: role of the HIF system. Nat Med 9:677–684
Radomsky ML, Thompson AY, Spiro RC, Poser JW (1998) Potential role of fibroblast growth factor in enhancement of fracture healing. Clin Orthop 355:283–293 (Suppl)
Risau W (1997) Mechanisms of angiogenesis. Nature 386:671–674
Vaillancourt H, Pilliar RM, McCammond D (1995) Finite element analysis of crestal bone loss around porous-coated dental implants. J Appl Biomater 6:267–282
Vaillaincourt H, Pilliar RM, McCammond D (1996) Factors affecting crestal bone loss with dental implants partially covered with a porous coating: a finite element analysis. Int J Oral Maxillofac Implants 11:351–359
Weber HP, Crohin CC, Fiorellini JP (2000) A 5-year prospective clinical and radiographic study of nonsubmerged dental implants. Clin Oral Implants Res 11:144–153
Weinbaum S, Guo P, You L (2001) A new view of mechanotrasduction and strain amplification in cells with microvilli and cells process. Biorheology 38:119–142
Acknowledgements
The authors thank Dr. Donato Di Iorio for his technical assistance. This work was partially supported by the National Research Council (C.N.R.), Rome, Italy, by the Ministry of Education, University, Research (M.I.U.R.), Rome, Italy, and by AROD (Research Association for Dentistry and Dermatology), Chieti, Italy.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Traini, T., Assenza, B., Roman, F.S. et al. Bone microvascular pattern around loaded dental implants in a canine model. Clin Oral Invest 10, 151–156 (2006). https://doi.org/10.1007/s00784-006-0043-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-006-0043-6