Abstract
The purpose of the present study was to histologically evaluate the healing of human intrabony defects following treatment with either a bovine-derived xenograft (BDX) and guided tissue regeneration (GTR) [BDX + GTR] or a bovine-derived xenograft mixed with collagen (BDX Coll) and GTR [BDX Coll + GTR]. Eight patients with chronic periodontitis and each with one very deep intrabony defect around a tooth scheduled for extraction were treated with either a combination of BDX + GTR (five patients) or with BDX Coll + GTR (three patients). The postoperative healing was uneventful in all eight cases. After a healing period of 6 months, the teeth or roots were extracted together with some of their surrounding soft and hard tissues and subsequently fixed in 10% buffered formalin. Following decalcification in EDTA, the specimens were embedded in paraffin and 8-µm histological sections were cut in the mesio-distal direction, parallel to the long axes of the teeth. The sections were alternatively stained with hematoxylin and eosin, van Giesson’s connective tissue stain or with the Ladevig’s connective tissue staining method and examined under the light microscope. Generally, formation of new cementum with inserting collagen fibers was found in seven out of the eight treated cases, whereas in the remaining case (treated with BDX + GTR) the healing was characterized by formation of a long junctional epithelium along the debrided root surface and no formation of cementum or bone. In the specimens demonstrating periodontal regeneration the new cementum was always of a cellular type. In most cases, the graft particles were surrounded by bone. In some areas, the bone tissue around the graft particles was connected by perpendicularly inserting collagen fibers to the newly formed cementum on the root surface. The epithelium downgrowth stopped always at the most coronal part of the newly formed cementum. No remnants of the membrane material were observed in any of the biopsies. Connective tissue encapsulation of the graft particles was rarely observed and was limited to the most coronal part of the defects. The findings of the present study provide evidence that treatment of intrabony defects with both BDX + GTR and BDX Coll + GTR may enhance periodontal regeneration in humans.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Regenerative periodontal therapy aims at restoring the tooth’s supporting structures which have been lost following inflammatory periodontal disease or trauma [8]. In humans, periodontal regeneration has been shown to be accomplished following the use of intraoral or extraoral autografts, demineralized freeze-dried bone allograft (DFDBA), guided tissue regeneration (GTR) and enamel matrix protein derivative (EMD) [1, 2, 5, 6, 7, 9, 10, 15, 16, 17, 18, 24]. Since the use of autografts for regenerative periodontal therapy is limited by its source and the increase in patient morbidity, different types of alloplastic grafts have been developed [12]. The use of different types of alloplastic grafts for regenerative periodontal treatment has been shown to improve the clinical parameters significantly, but histologically, no or only unpredictable periodontal regeneration may be obtained following the application of alloplastic materials [13, 20, 21, 22].
Histologic findings from human case reports have recently demonstrated that a bovine-derived xenograft (BDX) alone, or in combination with autogenous bone, GTR or EMD, may also enhance a regenerative type of healing as evidenced by formation of new cementum, new periodontal ligament and new alveolar bone [3, 4, 11, 19]. Very recently, the combination of BDX and collagen (BDX Coll) with or without GTR has also been shown to enhance periodontal regeneration in human intrabony defects [14]. Despite the positive results reported, there are still very limited data from human histological material evaluating these treatment modalities.
The purpose of the present study was, therefore, to histologically evaluate in humans the healing of advanced intrabony defects following regenerative periodontal therapy with either BDX + GTR or BDX Coll + GTR.
Materials and methods
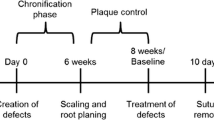
Eight patients (five females and three males) suffering from chronic periodontitis were included in the study. The study protocol was approved by the ethical committee of the Semmelweis University of Medicine, Budapest, Hungary. Each patient displayed one deep intrabony defect at a tooth or root scheduled for extraction due to advanced destruction of the attachment apparatus and further prosthetic considerations. The clinical measurements and defect characteristics for all eight patients are presented in Table 1. Criteria for inclusion in the study were: a) no systemic diseases which could influence the outcome of the therapy; b) good level of oral hygiene; and c) compliance with the maintenance program. The patients received oral hygiene instructions and full mouth scaling and root planing under local anesthesia 2 months prior to the surgical procedure.
The measurements were made with the same type of manual periodontal probe (PCP 12, Hu-Friedy, Chicago, IL, USA; probe tip diameter 0.4 mm) by one blinded and previously calibrated investigator. In cases where the position of CEJ was not clearly distinguishable, a restoration margin was used for the measurements. In the calculations evaluating PPD, GR and CAL, only the deepest site per tooth was included. The histometry was performed at the sites where these clinical measurements were previously made.
Surgical procedure
Following intracrevicular incisions, mucoperiosteal flaps were raised vestibularly and orally. All granulation tissue was removed from the defects and the roots were thoroughly scaled and planed using hand and ultrasonic instruments. Notches serving as landmarks for the histological measurements were prepared on the root surfaces at the most apical part of the defects. Vertical releasing incisions were performed only if necessary for a better access or to achieve a better closure of the surgical site. All granulation tissue was removed from the defects and the roots were thoroughly scaled and planed using hand and ultrasonic instruments. No root surface conditioning was performed.
The defects were filled with either bovine porous bone mineral granules of particle size 0.25–1.0 mm (BDX) (BioOss, Geistlich, Wolhusen, Switzerland) (five defects) or with bovine porous granules mixed with collagen (BDX Coll) (BioOss Collagen, Geistlich, Wolhusen, Switzerland) (three defects). Following grafting, a bioresorbable collagen membrane of porcine origin (BioGide Perio, Geistlich, Wolhusen, Switzerland) was trimmed and adapted over the defect so as to cover 2–3 mm of the surrounding alveolar bone and to ensure stability of the graft material. No sutures or pins were used for membrane fixation or stabilization. Finally, the mucoperiosteal flaps were repositioned coronally and fixed with vertical or horizontal mattress sutures.
Since no randomization was performed, the patients were treated consecutively first with BDX + GTR (the first five defects) and then with BDX Coll + GTR (the remaining three defects).
All patients received antibiotics for 1 week (1 g Augmentin/day). The postoperative care consisted of 0.2% chlorhexidine digluconate rinses twice daily for 4 weeks. Sutures were removed at 14 days after surgery. Recall appointments associated with professional tooth cleaning were performed once per week for the first 4 weeks and once per month for the remaining period. No subgingival instrumentation in the operated areas was performed during the entire experimental period of 6 months.
Histological procedure
Under local anesthesia mucoperiosteal flaps were raised and the roots were removed together with some of their surrounding soft and hard tissues. The biopsies were placed in 10% buffered formalin for fixation. After healing of the extraction sites the patients received fixed prosthetic reconstructions. The teeth were decalcified in EDTA, dehydrated and embedded in paraffin. Mesio-distal sections were cut parallel to the long axes of the teeth with the microtome set at 8 µm and subsequently stained with hematoxylin-eosin, van Giesson’s connective tissue stain or with the Ladevig’s connective tissue staining method. For the histological analysis three sections 100 µm apart and representing the central part of the teeth were selected. The histological analysis was performed by one blinded and calibrated examiner.
Results
The clinical and histological measurements are presented in Table 1.
Clinical findings
There were no complications such as abscesses or allergies against the graft or the membrane material. Membrane exposure occurred at 3 weeks after surgery in two cases (cases 1 and 7 from Table 1). The exposed parts of the membranes disintegrated within a few days without any adverse reactions. The clinical measurements revealed a PPD reduction and a CAL gain in all eight cases (Table 1).
Histological findings
No differences in the histological findings were observed between the two treatments. Therefore, the histological observations are characteristic for both treatments provided.
Formation of new cementum with inserting collagen fibers was found in seven out of the eight treated cases, whereas in the remaining case (case 5 from Table 1, treated with BDX + GTR) the healing was characterized by formation of a long junctional epithelium along the debrided root surface and no formation of cementum or bone. In the specimens demonstrating periodontal regeneration the new cementum was always of a cellular type (Figs. 1, 2, 3 and 4). In the areas demonstrating formation of cementum and periodontal ligament, the graft particles were embedded in bone (Figs. 1, 2, 3 and 4). In some areas, the bone tissue around the graft particles was connected by perpendicularly inserting collagen fibers to the newly formed cementum on the root surface (Figs. 3 and 4). The epithelium downgrowth stopped generally at the most coronal part of the newly formed cementum. No remnants of the membrane material were observed in any of the biopsies. Connective tissue encapsulation of the graft particles was rarely observed and was limited to the most coronal part of the defects.
Photomicrograph of healing following treatment with BDX + GTR. New cementum with inserting collagen fibers has formed on the debrided root surface. Most BDX particles (G) are surrounded by bone (NB). NC new cementum, D dentin, A artifact. (Original magnification ×25: van Giesson’s connective tissues stain)
Higher magnification of the defect shown in Fig. 1. The BDX particles (G) are surrounded by bone (NB). NC new cementum, NPL new periodontal ligament, A artifact. (Original magnification ×150: van Giesson’s connective tissues stain)
Representative histologic view of a healing following treatment with BDX Coll + GTR. The healing occurred in formation of new cementum with inserting collagen fibers (C) and new bone (NB) coronally to the notch (N) in the root surface. BDX (G) particles are surrounded by bone. A artifact. (Original magnification ×50: van Giesson’s connective tissues stain)
High-power magnification of the regenerated area shown in Fig. 3. BDX particle (G) is surrounded by bone. C new cementum, NPL new periodontal ligament, NB new bone. (Original magnification ×250: van Giesson’s connective tissues stain)
Discussion
The observations of this study have shown that healing of human intrabony defects following treatment with either BDX + GTR or BDX Coll + GTR was characterized by formation of new cementum, new periodontal ligament and new bone. In one out of the eight biopsies the healing occurred through formation of a long junctional epithelium along the debrided root surface and no periodontal regeneration. In the seven specimens demonstrating periodontal regeneration, the new cementum was always of a cellular type, which is in agreement with observations made in previous studies evaluating the healing of human intrabony defects following various regenerative techniques [1, 2, 6, 11, 15, 16, 17, 18, 19, 20]. In the seven specimens demonstrating a regenerative type of healing, most of the graft particles were surrounded by bone, which in turn points to the highly osteoconductive potential of the graft material. It is important to point out that in the two cases where a membrane exposure was observed, the healing was either characterized by a long junctional epithelium or the amount of regenerated cementum and bone was very limited. These observations corroborate findings from previous studies which have provided evidence that membrane exposure and subsequent bacterial colonization is one of the most important factors affecting healing following regenerative periodontal therapy with GTR [8, 23].
The finding that treatment with BDX + GTR may enhance periodontal regeneration in humans is in agreement with previously published reports [3, 4, 11, 19]. Furthermore, the observation that in all cases treated with BDX Coll + GTR, formation of cementum, periodontal ligament and bone were found indicates that also this treatment approach may promote a regenerative type of healing. In a very recent human histological study the healing response following treatment of intrabony defects with either BDX Coll alone or BDX Coll + GTR was evaluated [14]. The clinical results have shown that both treatment protocols led to a reduction in pocket depth and gain in clinical attachment level, whereas the histologic evaluation demonstrated in all four biopsies formation of cementum, periodontal ligament and bone.
All eight defects treated in the present study were very advanced 1–2 wall intrabony defects which are not optimal candidates for any type of regenerative therapy [8]. Conversely, it may be assumed that these defects had a rather limited potential for regeneration and thus, the histological results may only serve as proof of principle. On the other hand, it should be kept in mind that larger histological studies in humans are very difficult to perform due to obvious ethical reasons and, therefore, such findings should be used for supporting the biologic rationale for any type of regenerative treatment.
In none of the cases presented in this report was a collapse of the mucoperiosteal flap observed during the entire healing phase, a factor that may have significantly affected the amount of regenerated tissues [23]. Since all treated defects were very advanced intrabony defects, it may be assumed that the prevention of a flap collapse could especially be due to the graft material and may be responsible for ensuring space provision and wound stability [23].
The surgical protocol employed in the present study did not involve any chemical root surface conditioning, as was the case in previous studies evaluating the same treatment modalities [3, 4, 14]. Thus, it may be anticipated that the histological findings were most likely the effect of the employed regenerative materials.
It is, however, important to point out that based on the present results no conclusions on the possible advantage of using BDX + GTR or BDX Coll + GTR for treating intrabony defects can be drawn. As of now there are no data from controlled clinical studies comparing treatment with BDX Coll to access flap surgery or to treatment with BDX + GTR. Prospective, randomized, controlled clinical studies are needed in order to clarify these issues.
In conclusion, our findings together with the available data from the literature suggest that the clinical healing following treatment of intrabony defects with BDX + GTR and BDX Coll + GTR may represent, at least to a certain extent, periodontal regeneration characterized by formation of cementum, periodontal ligament and bone [3, 4, 11, 14, 19].
Conclusion
The findings of the present study provide evidence that treatment of intrabony defects with both BDX + GTR and BDX Coll + GTR may enhance periodontal regeneration in humans.
References
Bowers GM, Chadroff B, Carnevale R, Mellonig J, Corio R, Emerson J, Stevens M, Romberg E (1989) Histologic evaluation of new attachment apparatus in humans. Part I. J Periodontol 60:664–674
Bowers GG, Chardroff B, Carnevale R, Mellonig J, Corio R, Emerson J, Stevens J, Romberg E (1989) Histologic evaluation of new human attachment apparatus formation in humans: Part II. J Periodontol 60:675–682
Camelo M, Nevins M, Schenk R, Simion M, Rasperini G, Lynch S, Nevins M (1998) Clinical, radiographic, and histologic evaluation of human periodontal defects treated with Bio-oss and Bio-Gide. Int J Periodontics Restorative Dent 18:321–331
Camelo M, Nevins, ML, Lynch S, Schenk RK, Simion M, Nevins M (2001) Periodontal regeneration with an autogenous Bone-Bio-Oss composite graft and a Bio-Gide membrane. Int J Periodontics Restorative Dent 21:109–119
Dragoo MR, Sullivan HC (1973) A clinical and histologic evaluation of autogenous iliac bone grafts in humans. Part I. Wound healing 2 to 8 months. J Periodontol 44:559–613
Gottlow J, Nyman S, Lindhe J, Karring T, Wennström J (1986) New attachment formation in the human periodontium by guided tissue regeneration. Case reports. J Clin Periodontol 13:604–616
Hiatt WH, Schallhorn RG, Aaronian AJ (1978) The induction of new bone and cementum formation. IV. Microscopic examination of the periodontium following human bone and marrow allograft, autograft and non-graft periodontal regenerative procedures. J Periodontol 49:495–512
Karring T, Lindhe J, Cortellini P (1997) Regenerative periodontal therapy. In: Lindhe J, Karring T, Lang NP (eds) Clinical periodontology and implant dentistry. Munksgaard, Copenhagen, pp 597–646
Listgarten MA, Rosenberg MM (1979) Histological study of repair following new attachment procedures in human periodontal lesions. J Periodontol 50:333–344
Mellonig JT (1999) Enamel matrix derivative for periodontal reconstructive surgery: technique and clinical and histologic case report. Int J Periodontics Restorative Dent 19:9–19
Mellonig J (2000) Human histologic evaluation of a bovine-derived xenograft in the treatment of periodontal osseous defects. Int J Periodontics Restorative Dent 20:19–29
Nasr HF, Aichelmann-Reidy ME, Yukna RA (1999) Bone and bone substitutes. Periodontology 2000 19:74–86
Nevins ML, Camelo M, Nevins M, King CJ, Oringer RJ, Schenk RK, Fiorellini JP (2000) Human histologic evaluation of bioactive ceramic in the treatment of peridontal defects. Int J Periodontics Restorative Dent 20:458–467
Nevins ML, Camelo M, Lynch SE, Schenk RK, Nevins M (2003) Evaluation of periodontal regeneration following grafting intrabony defects with Bio-Oss Collagen: a human histologic report. Int J Periodontics Restorative Dent 23:9–17
Nyman S, Lindhe J, Karring T, Rylander H (1982) New attachment following surgical treatment of human periodontal disease. J Clin Periodontol 9:290–296
Sculean A, Donos N, Chiantella GC, Windisch P, Reich E, Brecx M (1999) Treatment of intrabony defects with bioabsorbable membranes. A clinical and histologic study. Int J Periodontics Restorative Dent 19:501–509
Sculean A, Donos N, Windisch P, Gera I, Brecx M, Reich E, Karring T (1999) Healing of human intrabony defects following treatment with enamel matrix proteins or guided tissue regeneration. J Periodont Res 34:310–322
Sculean A, Chiantella GC, Windisch P, Donos N (2000) Clinical and histologic evaluation of treatment of intrabony defects with an enamel matrix protein derivative (Emdogain). Int J Periodontics Restorative Dent 20:375–381
Sculean A, Windisch P, Keglevich T, Chiantella GC, Gera I, Donos N (2003) Clinical and histologic evaluation of human intrabony defects treated with an enamel matrix protein derivative combined with a bovine-derived xenograft. Int J Periodontics Restorative Dent 23:47–55
Sculean A, Windisch P, Keglevich T, Gera I (2004) Clinical and histological evaluation of an enamel matrix protein derivative combined with a bioactive glass for the treatment of intrabony periodontal defects in humans. Int J Periodontics Restorative Dent (in press).
Stahl SS, Froum S (1987) Histologic and clinical responses to porous hydroxylapatite implants in human periodontal defects. 3 to 12 months postimplantation J Periodontol 58:689–695
Stahl SS, Froum S, Tarnow D (1990) Human clinical and histological responses to the placement of HTR polymer particles in 11 intrabony lesions. J Periodontology 61:269–274
Wikesjö UME, Selvig KA (1999) Periodontal wound healing and regeneration. Periodontology 2000 19:21–39
Yukna RA, Mellonig JT (2000) Histologic evaluation of periodontal healing in humans following regenerative therapy with enamel matrix derivative. A 10-case series. J Periodontol 71:752–759
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sculean, A., Stavropoulos, A., Windisch, P. et al. Healing of human intrabony defects following regenerative periodontal therapy with a bovine-derived xenograft and guided tissue regeneration. Clin Oral Invest 8, 70–74 (2004). https://doi.org/10.1007/s00784-004-0254-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-004-0254-7