Abstract
After a caries decline of about 80% in children in Western Europe and other industrialized countries, there should be critical debate about the best way for future caries prevention. Multiple fluoride use played an important role in caries reductions achieved in the 1980s and 1990s, but it also resulted in a polarization of lesion distribution in young people: the majority consists of low-caries or even lesion-free individuals, while a minority is a so-called high caries risk group which seems not to be open to preventive programs. Recent studies indicate that frequent fluoride applications (>6 times/year) in conjunction with effective plaque removal can be a successful approach for effective future caries prevention in high caries risk groups. Health promotion programs that are merely educational and do not provide fluoride do not seem to be effective. Alternatively, preventive measures could be performed at home or in a private practice, but only minimal compliance is reached in high risk groups compared with out-reaching group programs. Thus, group programs are instrumental in providing effective and efficient caries-preventive measures in children. The more expensive time of a dental practice team should be limited to procedures where costly equipment is needed (professional tooth cleaning, sealants, etc.). For efficient caries prevention, measures formerly targeted specifically at either populations, groups, or individuals should be remodeled and aimed to interact in order to achieve optimal oral health in children at a reasonable cost.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Caries prevalence has decreased in children and adolescents in industrialized countries [24] by about 80%. Therefore, many decision makers, assuming that the caries problem has been solved, are posing the question Can we abandon caries preventive programs now? But even professionals are skeptical about the effectiveness of certain preventive measures or at least their cost-benefit ratio. Especially group preventive programs and semi-annual fluoride applications are questionable, as has been shown in a recent retrospective evaluation of the effect of the routine professional application of topical fluoride on caries and treatment experience in adolescents of low socio-economic status in the Netherlands [31]. As we know, caries activity is an imbalance between detrimental (sugars and bacteria) and preventive factors. At the moment, the preventive factors neutralize the cariogenic challenge in many children, but a reduction of prophylactic measures implies the risk of shifting the balance toward higher caries activity.
Epidemiologic situation
A closer look at the recent patterns of caries distribution shows that the caries decline has not occurred uniformly on all levels. In Europe, people in the former socialistic countries generally show a higher caries prevalence than in Western European countries [38]. Within most countries, there are considerable regional differences in caries prevalence, e.g., in the economically less affluent Mediterranean south of France or between western and eastern Germany [25, 27]. In addition, caries prevention in the deciduous dentition has been less successful than in permanent teeth: children accumulate more carious defects in their first 6 years (deft) than in the following 6 (DMFT), and early childhood caries in some populations even tends to rise [27, 28].
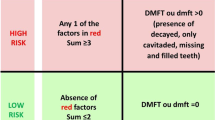
At a group and individual level, lesion distribution became skewed after the caries decline: about 25% of so-called (high) caries risk children developed about 75% of the carious defects. Education and deprivation seem to be the most important grouping variables, e.g., German gymnasium pupils show half the caries experience of their counterparts in the basic schools [27]. Low socio-economic status is an excellent indicator for a high treatment need in children [12].
At the tooth and surfaces level, epidemiologic surveys show that caries prevention has been less successful in the first permanent molars, especially their occlusal surface, where up to 80% of the carious defects are accumulated in adolescence [33].
Thus, even after the caries decline, a considerable number of caries lesions is present and progressing, and more targeted preventive programs seem to be necessary instead of abolishing caries prevention.
For these targeted preventive programs, precise information regarding the following points is needed:
-
Current caries prevalence and distribution
-
Etiologic and risk factors
-
Effective, efficacious and efficient preventive measures
-
Ways of access to the participants
-
Costs
Effective caries prevention
The epidemiologic situation, caries etiology and risk factors have been researched intensively during the last decades [3]. Also, the preventive measures which led to the caries decline were well documented and examined. Systematic reviews and expert views on the effectiveness of caries preventive measures [3, 13, 17, 18, 19] clearly agree on the strong evidence for caries reductions via fluoride. Summarizing earlier investigations, Kay and Locker [13] stated that oral health programs which did not use fluorides failed to achieve caries reductions. Daily brushing with fluoride toothpaste seems to be easier to achieve than the regular use of fluoride supplements. The systematic review [13] also points out that “there is no evidence that oral health promotion per se affects caries rates.” Thus, the effectiveness of purely informational or motivational presentations should be questioned.
During the introduction of fluorides in preventive dentistry, almost any fluoride application resulted in significant caries reductions (Table 1). Even two applications of fluoride gels, fluids or varnishes per year resulted in up to 60% reduction of caries incidence [2, 17, 18, 37]. Fluoridated domestic salt, the cheapest measure of all, has been recommended in Switzerland (83% market share since 2000) and Germany (53% market share in 2002) [23]. In these two countries, fluoridated salt has largely replaced fluoride supplements whose public value, important in some countries decades ago, is not warranted any more [5].
Besides the data on effectiveness which resulted from clinically controlled studies, the efficacy (effectiveness under field/routine conditions) and the efficiency (cost-cost or cost-benefit ratio) are of key importance for the assessment of a preventive measure. Except for the biannual topical application in a private practice setting, fluoride use is cost-effective in comparison to restorative treatment, even considering the time needed to perform the fluoride program, which clearly neglects complications and cost of replacing fillings (Table 1). Fluoridated salt offers the best cost-benefit ratio, even if costs under European conditions could be in the range of 0.03–0.05 euro rather than 0.01 euro [23]. In contrast to this simplistic analysis, multiple fluoride use is believed to be an important factor for caries decline [21], but in combined use, the efficacy of every added fluoride is less than in single use. Unfortunately, the combined use of fluoride has not been well examined. A study in which the effect of amine fluoride toothpaste and gel was assessed in a controlled trial showed a lower caries incidence with the amine fluoride toothpaste in comparison with other traditional oral hygiene and a further significant reduction with the additional use of fluoride gel [16].
The use of fluoride by itself can alter the caries distribution within a population. For instance, besides a general caries reduction in comparison with non-fluoridated areas, water fluoridation in Australia reduced the effect of socio-economic inequities by 1 dmfs for mean values between high and low socio-economic classes [32]. In contrast to this “depolarization,” fluoride programs can also polarize the caries distribution: semi-annual fluoride varnish applications in children with low baseline caries values resulted in a 63% reduction of the caries increment after 6 years, but only a 25% reduction for children with initially high caries values after the same time period [14]. This reduced effectiveness of fluoride applications in highly caries-active children might be caused by a lack of oral hygiene, subsequent heavy plaque accumulation, and a biofilm which reduces the availability of fluoride directly on the tooth surface. Thus, a combination of fluorides and at least moderate oral hygiene might be needed for further caries reductions.
Caries prevention after the caries decline
Since the reasons for the successful caries decline of the past are known and a stable level of “basic prevention” is established, further efforts should concentrate on:
-
(High) risk children
-
(High) risk surfaces
A literature review of preventive programs in caries-risk children reveals a rather frustrating picture. Bader et al. [1] conclude in their systematic review that the strength of evidence for the efficacy of fluoride varnish programs is fair, but insufficient for all other methods. For instance, 3–4 varnish applications per year resulted in a 37% reduction of the caries increment in children in a deprived area [40]. Exemplary of the difficulties of intensive prevention are the studies by Hausen et al. [11]. Their analysis of the effects of counseling, F-varnish, F-lozenges, sealants and chlorhexidine use revealed minor caries reductions compared with basic prevention (counseling, one F-varnish per year); Pieper [26] found twice the caries increment in high-caries-risk children with professional tooth cleaning every 2 weeks than in low-risk children with only two topical fluoride applications per year. Thus, the risk prognosis was correct at a group level, but the effort to benefit the high-caries-risk groups was not successful. This is confirmed by Marthaler [20], who proposed selective intensive prevention in schoolchildren in 1975, but 20 years later had to admit that no highly effective preventive programs are known for high-caries-risk children due to low compliance [22]. In summary, Medline-based reviews conclude that several methods have been developed for the identification of high-risk groups or children with sensitivities and specificities in the range of 51–98% [29], but it is difficult to implement targeted programs in many situations [15, 34].
A closer look reveals that community or school dental programs, which have difficulties presenting their results in Medline-listed publications, have developed several successful methods for further caries reductions: Brunner-Strepp [4] achieved very low caries prevalence by weekly supervised brushing with elmex fluid at school and low caries prevalence in high-caries-risk children with four professional applications of elmex fluid in comparison with a control group. Even at the very low caries level in Solothurn/Switzerland (0.77 DMFT, 12-year-olds), where the use of fluoride toothpaste and fluoride salt is high (>90% and 80%, respectively), Guindy et al. [10] found a correlation between caries prevalence and the number of group prevention impulses (instruction, brushing with fluoride preparation). Trummler and Weiss [36] conclude that the very low caries level in St. Gallen/Switzerland (0.75 DMFT, 12-year-olds) is based on the school dentistry act of 1982 which obliges kindergarten and school teachers to take an active role in caries prevention, e.g., brushing of a fluoride gel at school twice every month for grades 1–6, which resulted in about 20 fluoride applications per year.
The community with the lowest caries prevalence in Europe is Nexö/Denmark (0.23 DMFS, 12-year-olds). Their program is based on early access to all children of the community from 8 months of age, a high quality of plaque control plus F-application, which simply means toothbrushing additionally performed by the parents, as well as risk-based recall intervals. The success is well documented in the Nexö studies [6, 7, 8, 9, 35]. Special attention is given to the occlusal surface of the first permanent molar during eruption. As it has a long eruption span and is not cleaned by the conventional horizontal brushing technique (Fig. 1), the children and parents are trained in a special cross-brushing technique.
In order to implement the above-mentioned preventive measures, access to the children is necessary, especially when the compliance of the family is reduced and they are not eager to take part in even free-of-charge preventive programs in private offices. A repeated outreach program offers better chances to reach children most in need of dental prevention, as shown by a study on the effect of school dental screening on dental attendance, which revealed much more visits at the dentist (73%) for children provided with a reply slip and a follow-up than for children without follow-up (42%) [39].
Summary and conclusions
In summary, an appropriate method of collective fluoride use which leads to high caries reductions at low cost should be established in every country. Group prevention programs do not seem to produce caries reduction if they are merely educational and do not apply fluoride. Recent studies indicate that frequent fluoride applications (>6 times/year) in conjunction with effective plaque removal are needed for caries reductions exceeding the results of individual home care. The effectiveness and efficiency of these programs is high. Such measures should pay special attention to including the occlusal surface of the first permanent molar during eruption. Alternatively, these preventive measures could be performed at home or in a private practice, but both approaches fail to reach the children and families most in need of prevention. Furthermore, the costs in a private practice are much higher, meaning a reduced efficiency in comparison with group programs. Thus, group programs offer access to provide effective and efficient caries-preventive measures in children. The more expensive time in a dental practice should be limited to procedures where costly equipment is needed (professional tooth cleaning, sealants, further diagnostics such as bitewing radiographs, or restorative treatment). An interaction of collective, group, and individualized caries prevention is required to achieve optimal oral health in children at a reasonable cost.
References
Bader JD, Shugars DA, Bonito AJ (2001) Systematic reviews of selected dental caries diagnostic and management methods. J Dent Educ 65:960–968
Brambilla E, Toselli A, Felloni A, Gagliani M, Malerba A, Strohmenger L (1997) The effect of biannual applications of amine fluoride solution on caries incidence in permanent first molars: a 5-year study. Int J Paediatr Dent 7:9–14
Bratthall D, Hänsel Petersson G, Sundberg H (1996) Reasons for the caries decline: what do the experts believe? Eur J Oral Sci 104:416–422 (Discussion, pp 423–425, 430–432)
Brunner-Strepp B (2001) Intensive fluoridation in group prevention programs, a long term observation (Abstract 32). Community Dent Health 18:199
Burt B (1999) The case of eliminating the use of dietary fluoride supplements for young children. J Publ Health Dent 59:269–274
Carvalho JC, Thylstrup A, Ekstrand KR (1992) Results after 3 years of non-operative occlusal caries treatment of erupting permanent first molars. Community Dent Oral Epidemiol 20:187–192
Ekstrand K, Christiansen C, Christiansen J (2000) Cost minimisation analysis of two occlusal caries preventive programmes. Community Dental Health 17:260–261
Ekstrand KR, Christiansen ME, Qvist V (2003) Influence of different variables on the inter-municipality variation in caries experience in Danish adolescents. Caries Res 37:130–141
Ekstrand KR, Nielsen LA, Carvalho JC, Thylstrup A (1993) Dental plaque and caries on permanent first molar occlusal surfaces in relation to sagittal occlusion. Scand J Dent Res 101:9–15
Guindy JS, Weber C, Meyer J (2000) Die Zahngesundheit von 7- und 12-jährigen Schülerinnen und Schülern im Kanton Solothurn. Acta Me Dent Helv 5:119–124
Hausen H, Karkkainen S, Seppa L (2000) Application of the high risk strategy to control dental caries. Community Dent Oral Epidemiol 28:26–34
Jones CM (2001) Capitation registration and social deprivation in England. An inverse ‘dental’ care law? Consultant in Dental Public Health, Highland Health Board, Assynt House, Inverness. Br Dent J 24:203–206
Kay E, Locker D (1998) A systematic review of the effectiveness of health promotion aimed at improving oral health. Community Dent Health 15:132–144
Klimek J, Schmidt S, Schmidt HFM, Jürgensen R (1992) Der kariesprophylaktische Effekt von Duraphat nach 6 Jahren in Abhängigkeit vom Kariesrisiko. Dtsch Zahnärztl Z 47:761–763
Letters to the Editor (2002) Community Dent Health 19:187–189
Madlena M, Nagy G, Gabris K, Marton S, Keszthelyi G, Banoczy J (2002) Effect of amine fluoride toothpaste and gel in high risk groups of Hungarian adolescents: results of a longitudinal study. Caries Res 36:142–146
Marinho VC, Higgins JP, Logan S, Sheiham A (2002) Fluoride gels for preventing dental caries in children and adolescents. Cochrane Database Syst Rev 2: CD002280
Marinho VC, Higgins JP, Logan S, Sheiham A (2002) Fluoride varnishes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev 3: CD002279
Marinho VC, Higgins JP, Sheiham A, Logan S (2003) Fluoride toothpastes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev 1: CD002278
Marthaler T (1975) Selektive Intensivprophylaxe zur weitgehenden Verhütung von Zahnkaries, Gingivitis und Parodontitis beim Schulkind [Selective intensive prophylaxis for major reductions of the incidence of dental caries, gingivitis and periodontitis in the school children] SSO Schweiz Monatsschr Zahnheilkd 85:1227–1240
Marthaler TM (1990) Cariostatic efficacy of the combined use of fluorides. J Dent Res 69:797–800 (Discussion, pp 820–823)
Marthaler TM (1995) Zahnmedizinische Gruppenprophylaxe in der Schweiz: Beobachtungen und Schlüsse für die Vorbeugung in Deutschland. DAZ-forum 14:211–214
Marthaler TM (2003) Success and drawbacks in the caries-preventive use of fluorides—lessons to be learnt from history. Oral Health Prev Dent 1:129–140
Marthaler TM, O’Mullane DM, Vrbic V (1996) The prevalence of dental caries in Europe 1990–1995. ORCA Saturday afternoon symposium 1995. Caries Res 30:237–255
Muller M, Jasmin JR (1988) L’etat bucco-dentaire d’une population d’enfants scolarises dans le Sud-Est de la France. [The oro-dental status of a population of school children in the southeast of France]. Faculte de Chirurgie-Dentaire, Parc Valrose, Nice J Biol Buccale 16:239–244
Pieper K (1990) Selektive Intensivprophylaxe im Rahmen der Gruppenprophylaxe. [Selective intensive prophylaxis in area of group prophylaxis] ZWR 99:174–179
Pieper K (2001) Epidemiologische Begleituntersuchungen zur Gruppenprophylaxe 2000. S & W Druckerei und Verlag, Marburg
Poulsen S, Pedersen MM (2002) Dental caries in Danish children: 1988–2001. Eur J Pae Dent 3:195–198
Powell LV (1998) Caries prediction: a review of the literature. Community Dent Oral Epidemiol 26:361–371
Schmelzer J (2002) Einschätzung der Effektivität von Inividual-Prophlaxeprogrammen zur Verbesserung der Mundhygiene. Prophylaxe impuls 6:167–173
Schuller AA, Kalsbeek H (2003) Effect of the routine professional application of topical fluoride on caries and treatment experience in adolescents of low socio-economic status in the Netherlands. Caries Res 37:172–177
Spencer AJ, Slade GD, Davies M (1996) Water fluoridation in Australia. Community Dent Health: 13[Suppl 2]: 27–37
Splieth Ch, Rosin M, Kuusela S, Honkala E (1999) Erkrankungs- und Therapiemuster der Karies bei Kindern in zahnärztlichen Praxen. Oralprophylaxe 21:122–125
Tickle M (2002) The 80:20 phenomenon: help or hindrance to planning caries prevention programmes? Community Dent Health 19:39–42
Thylstrup A, Vinther D, Christiansen J (1997) Promoting changes in clinical practice. Treatment time and outcome studies in a Danish public child dental health clinic. Community Dent Oral Epidemiol 25:126–134
Trummler A, Weiss V (2000) DMFT scores in 12-year-old school children in the city of St. Gallen. Oralprophylaxe 22:206–208
van Rijkom HM, Truin GJ, van’t Hof MA (1998) A meta-analysis of clinical studies on the caries-inhibiting effect of fluoride gel treatment. Caries Res 32:83–92
WHO (2003) Oral Health Country/Area Profile Programme
Zarod BK, Lennon MA (1992) The effect of school dental screening on dental attendance. The results of a randomised controlled trial. Community Dent Health 9:361–368
Zimmer S, Robke FJ, Roulet JF (1999) Caries prevention with fluoride varnish in a socially deprived community. Community Dent Oral Epidemiol 27:103–108
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Splieth, C.H., Nourallah, A.W. & König, K.G. Caries prevention programs for groups: out of fashion or up to date?. Clin Oral Invest 8, 6–10 (2004). https://doi.org/10.1007/s00784-003-0250-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-003-0250-3