Abstract
Collection of salivary cortisol has been widely used as a method of investigating an array of health parameters. Monitoring of cortisol levels can help us to understand stress levels and the body’s response to stressors. Traditional methods of measuring cortisol in saliva, however, require costly equipment, trained personnel, and transportation of samples to a centralized laboratory. This creates a barrier to personal monitoring of cortisol. It also adds a level of cost and difficulty to large-scale studies which require participants to store and ship their saliva samples. Here, we present a novel system in which an individual with minimal training may collect their own saliva sample and measure it at home. Our system utilizes a lateral flow assay, a portable imaging device, and a smartphone to give salivary cortisol results in less than 15 min. We also demonstrate the use of our system on samples from a human study and give results from that study, which analyzes the relationship between cortisol levels and alertness across multiple days.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Cortisol is the so-called “stress hormone,” as it is a hormone produced in the body in response to a stressor. It is a product of the hypothalamic-pituitary-adrenal (HPA) axis, which is activated by stressors and produces a cascade of hormones which finally causes the production of cortisol in the adrenal gland [1]. Cortisol is involved in the process of maintenance of homeostasis in the body, termed “allostasis” [2]. Allostasis allows for adaptation to challenges which arise in daily life as well as major life stressors. The release of mediators of allostasis such as cortisol promotes adaptation to changes in a person’s situation [2]. As the HPA axis is activated in response to a stressor, the resulting cascade of hormones, which includes cortisol, causes improved alertness, attention, and reaction time [3].
Cortisol production, like many neurobehavioral processes, shows a roughly 24-h period known as a circadian rhythm. Cortisol’s rhythm causes it to sharply increase and peak between 30 and 45 min after awakening, decrease throughout the day, and increase again overnight. The increase in cortisol after awakening is called the cortisol awakening response (CAR). This rhythm can be affected by stress, shift work, depression, and other conditions [4]. Circadian profiles across individuals also vary, which can influence the timing and phase of cortisol secretion over the day [5]. Similarly, alertness profiles of different chronotypes are also known to be distinct—early types are more alert earlier in the day while late types are more alert later [6]. There are a range of other factors which can impact the individual’s cortisol response to daily events as well as stressors, making it important to assess cortisol levels individually rather than taking the entire population as a whole [7]. Due to these daily fluctuations and personal variations, a single measurement is insufficient to estimate the daily cortisol or alertness profile. By taking multiple samples across the day, the daily profile for each individual can be approximated and variations between days can be observed.
In many studies, salivary cortisol is measured by collecting saliva samples from participants and using traditional laboratory methods to analyze the concentration of cortisol in the sample. Methods used by recent studies include immunoassay techniques [8, 9] and liquid chromatography tandem-mass spectrometry [10]. Point-of-care techniques which use electrochemical reactions [11] and chemiluminescent signals [12] have also been developed. Traditional laboratory methods are expensive, use specialized equipment, require trained personnel, and require relatively large amounts of time. The point-of-care techniques which are currently being developed for salivary cortisol measurement use specialized equipment [11] or else require the user to act within a 1-min window in order to capture a usable image [12]. Researchers are also working on stress monitoring which utilizes ambient intelligence and monitoring; however, many of these do not use physiological markers but rather facial and voice monitoring for signs of stress or nonspecific markers such as heart rate and body temperature [13]. Here, we present a point-of-care lateral flow assay which measures cortisol concentration using a colorimetric signal that is imaged and processed by an inexpensive portable reader which interacts with a mobile device. Our novel system does not require large or expensive equipment and is easy to use, while still providing an accurate result.
For objectively assessing alertness, sleep clinicians and researchers commonly use the psychomotor vigilance task (PVT), which is a reaction time (RT) test. During the test, a visual stimulant is shown at a random interval and the user is instructed to respond to the visual stimulant (e.g., pressing a physical button). Here, the PVT is adapted to a mobile format, PVT Touch [14], which is implemented on subjects’ personal smartphones. Various statistical summaries of the reaction times during the test have been shown to correlate with wakefulness, sleep deprivation, and fatigue across different populations [15,16,17]. One distinct advantage of using PVT to assess cognitive performance over a long period of time is its immunity to practice or learning effects [18].
Both cortisol and alertness have been related to sleeping habits. The cortisol circadian rhythm is affected by shift work [19], and alertness is diminished by severe lack of sleep [20]. Another marker which has been linked to sleep is melatonin, a hormone secreted by the pineal gland. Melatonin has also been shown to decrease alertness and increase sleepiness when administered exogenously [21]. Salivary melatonin has been shown to correlate with serum levels of melatonin and to act as a marker of circadian phase [22, 23]. We have included melatonin in our study in order to assess the relationship between endogenous melatonin and alertness levels.
In this paper, we demonstrate a smartphone-based system which enables users to quantify and track personal levels of salivary cortisol and alertness. We validated our system in human samples from a study in which we observed measures of cortisol, melatonin, alertness, and sleep. While these things have all been studied separately in great detail, to the best of our knowledge, there have been no studies to date that examine the possibility of relationships between these metrics. Our novel point-of-care cortisol diagnostic system would allow users to track their own cortisol levels and creates an opportunity for the enhancement of salivary cortisol research.
2 Materials and methods
2.1 Preparation of gold nanoparticle (AuNP) conjugates with anti-cortisol antibodies
Innovacoat Gold Conjugation Kit (Innova Biosciences, Cambridge, UK), consisting of freeze-dried 40 nm AuNPs, was used for the conjugation process. We used the proprietary lysine residues existing on the surface of the Innovacoat AuNPs to obtain stable conjugation. We obtained mouse monoclonal anti-cortisol antibodies from CalBioreagents Inc. (San Mateo, CA, USA) and incubated them with the AuNPs. We then added a quenching buffer to terminate the conjugation reaction and centrifuged the solution to remove excess antibodies. These conjugates were stored at 4 °C until diluted to the desired optical density (O.D.) in a conjugate buffer, consisting of 2 mM borate buffer and 5% (w/v) sucrose (for resolubilization).
2.2 Preparation of lateral flow assay for cortisol detection
2.2.1 Conjugate pad preparation
We soaked glass fiber conjugate pads (GFDX103000, EMD Millipore, Billerica, MA, USA) cut to 30 cm × 5 mm for 2 min with the anti-cortisol conjugated AuNPs diluted to an O.D. of 0.18. We then dried them in an incubator at 37 °C overnight.
2.2.2 Nitrocellulose membrane preparation
We obtained nitrocellulose membranes (HF180MC100, EMD Millipore) with a 2.5-cm capillary length. We used a solution of 0.4 mg/ml Cortisol-BSA conjugate (CalBioreagents Inc.) diluted in 0.1× PBS for the test line and a 2.0-mg/ml solution of lyophilized anti-mouse IgG produced in goat (Sigma Aldrich Co. LLC, St. Louis, MO, USA) in 0.1× PBS for the control line. We dispensed both the solutions onto the nitrocellulose membrane using a Lateral Flow Reagent Dispenser (Claremont Biosolutions, Upland, CA, USA) attached to Legato 200 Dual Syringe Pump (Claremont Biosolutions), dispensing at a rate of 6.4 μL/min, which resulted in uniform test and control line width of approximately 1 mm, and a distance of 3 mm between the two lines after dispensation. We then dried the membrane overnight in a 37 °C incubator. The test and control lines are depicted in Fig. 1b, with the test line shown in green and the control line shown in orange.
Overview of lateral flow assay and system. a Depiction of process for running a lateral flow assay with a collected saliva sample. (From left to right): Saliva swab in collection tube, pressure application on saliva swab, tube with swab and tube insert removed and a disposable capillary tube, deposition of saliva from capillary tube to lateral flow assay, portable imaging device, image sent to smart device via Wi-Fi. b Schematic of lateral flow assay
2.2.3 Assembly and storage of the lateral flow assay
The test strip is made of several parts assembled on an adhesive backing pad, as shown in Fig. 1b. Cellulose fiber sample pad (CFSP203000, EMD Millipore) acted both as the sample pad for sample loading and as the absorbent pad at the end of the assay strip. We used an unsoaked glass fiber membrane (30 cm × 5 mm) as a spacer pad between the soaked conjugate pads and the nitrocellulose membrane to act as a small incubation area to allow for enhanced reaction between AuNP conjugates and the sample before they flow onto the nitrocellulose membrane. We created an overlap of 0.5 mm both between the spacer pad and the nitrocellulose membrane, and the spacer pad and the soaked conjugate pad, and an overlap of 2 mm between the soaked conjugate pads and the sample pad. We subsequently attached a cover tape (Kenosha, Amstelveen, The Netherlands) to secure the sample pad, the conjugate pad, the spacer, pad and the nitrocellulose membrane, and ensure proper contact between the respective membranes. We then used a rotary paper trimmer (Dahle North America, Inc., Peterborough, NH, USA) to cut the assembled 30-cm assay strip into individual 4-mm-wide test strips subsequently used for experiments. For storage of the strips, we added silica gel desiccants to the storage box to prevent damage to the test strips by atmospheric moisture.
2.3 Study design and recruitment of participants
Through public emails and recruitment posters, we recruited 13 participants from the Cornell University community. We described the study procedure in detail to the participants during an initial interview. The study was approved by Cornell University’s Institutional Review Board and all participants provided written informed consent prior to participation. All protocols were carried out in accordance with the relevant guidelines and regulations. Briefly, the participants were instructed to collect six saliva samples daily—three samples in the morning with one at waking and two at intervals of 30 and 45 min after waking and subsequently one sample each in the afternoon, evening, and night. Saliva collection kits (Salimetrics, State College, PA, USA) consisting of a saliva swab and collection tubes were provided to each participant. They were asked to note the time and date on each sample tube and store them in either refrigerators or freezers, whichever might be more easily accessible to the participant. Participants were asked to drop off the samples in a cold storage box each day, from which we collected and stored the samples in a freezer at − 20 °C until they were thawed later for enzyme-linked immunosorbent assay (ELISA) analysis.
To assess alertness, we used the PVT, a widely used reaction test for measuring alertness [15]. While the original PVT version requires specialized hardware, we used a validated smartphone implementation, PVT-Touch [17]. In this test, a visual stimulus (in this case, a black and white checker pattern) is shown at random intervals to the participant, who responds by touching the phone screen. A visual representation of this can be seen in Supplementary Fig. 1. Reaction times are measured in milliseconds, and various statistical summaries of reaction time have been shown to be indicative of alertness [24]. While the original PVT version took around 10 min to complete, subsequent brief versions have also been shown to be reflective of changes in alertness [25]. In this work, we administered a 3-min version—a duration which has been validated for alertness assessment [26].
Participants were instructed to complete the PVT tasks 4 times a day—once each in the morning, afternoon, evening, and night, and if possible, at the same time as the saliva samples were collected. We reminded the participants to take saliva samples and PVT tasks using passive phone notifications. Given that speed and accuracy is important for PVT tests, we instructed participants during the initial interview to only begin a test if they expected to have 5 min without significant distraction. We also provided instructions and demonstrated how to perform the PVT on each person’s phone.
In addition to the PVT, we collected subjective measures of alertness including Chalder Fatigue Scale [27] and Fatigue Visual Analogue Scales (VAS) [28]. Participants also completed sleep journal recording when they went to sleep at night and upon awakening in the morning.
Participants were expected to take 7 days of samples (42 saliva samples and 28 PVT surveys overall) within a period of 2 weeks. Compensation was provided to participants, a detailed account of which can be found in the Supplementary Information.
2.4 Analysis of saliva samples
Frozen saliva samples were first thawed and then centrifuged at 3500 rpm for 10 min, followed by immediate analysis via ELISA kits to ascertain the cortisol and melatonin content in each sample. Commercially available cortisol and melatonin ELISA kits (Salimetrics, State College, PA, USA) were used for this purpose. ELISA protocol required 25 μl of saliva for the cortisol kit and 100 μl of saliva for the melatonin kit. In the samples in which there was not enough volume to allow for both tests, only cortisol levels were analyzed.
2.5 Analysis of PVT surveys
Each single PVT session required the participant to provide around 3 min of responses. Each of these responses was measured in milliseconds and was classified into three categories: false start, normal response, and lapse. A false start occurred when the user tapped the screen before the stimulus or within 100 ms of the appearance of the stimulus. A lapse occurred when it took more than 500 ms for the user to respond, and a normal response was anywhere between 100 and 500 ms [20, 24]. Number of false starts and lapses was counted for each session while a median RT was calculated from all the normal responses from a session. These three parameters were then separately used to quantify the PVT session [20].
2.6 Test strip protocol
A schematic of the test strip running process is shown in Fig. 1a. Saliva samples are collected using a swab which is placed under the tongue for 1–2 min. This swab is placed in a disposable tube which can be used to store the sample and to hold the swab in place while saliva is forced out of the swab by pressure or centrifugation. The saliva is then at the base of the tube and can be pipetted onto the test strip. For our study, stored saliva samples were thawed and subsequently centrifuged at 3500 rpm for 10 min before being used for the lateral flow assay. The assay strips were housed in a standard lateral flow cassette. Forty microliters of sample was then loaded onto the sample pad. This allowed the sample to wet the soaked conjugate pad, release the AuNP conjugates, and settle onto the spacer pad, where the sample and the conjugates were allowed to react for 5 min. At the end of 5 min, 40 μL of running buffer consisting of 1× TBS with 1% BSA, 1.5% Tween20, and 0.1% sodium azide was added to the sample inlet to initiate the assay. This forced the conjugates to flow from the spacer pad across the nitrocellulose membrane, where they would subsequently interact with the dispensed test and control lines and onto the absorbent pad (see Fig. 1a). At the test line, there is a competitive interaction between cortisol which is bound to the AuNP-antibody conjugates and cortisol immobilized on the test line. The signal at the test line therefore decreases with increasing cortisol concentration. At the control line, the secondary antibody immobilized on the surface binds to the remaining AuNP-antibody conjugates. A wait time of 5 min was used to allow the colorimetric signal to develop at the two lines, which were then read and analyzed in our imaging device (shown in Fig. 1a) as detailed below.
2.7 Calibration curve
Eight saliva samples with known values (through ELISA analysis) of cortisol concentration between 0 and 0.5 ng/ml were thawed and centrifuged as detailed above. They were then mixed together to obtain a single saliva solution consisting of a cortisol concentration between 0 and 0.5 ng/ml. This saliva solution was divided into five different solutions, which were then spiked with a known cortisol-BSA solution prepared in 1× PBS, to obtain saliva samples with final concentrations of approximately 0, 2.5, 5, 10, 30, and 50 ng/ml. These were then dispensed on the lateral flow assay according to the protocol laid out above for the human saliva samples. The ratio of the intensities of the test and control lines was used as the final signal value. The signal values of all the calibration samples were normalized to the mean signal value of the 0 ng/ml samples. These normalized values were then used to create a calibration curve for test to control line ratio and cortisol concentration. This curve was used to quantify cortisol levels in subsequent saliva samples.
2.8 Test strip image readout and image processing
Test strips in cassettes were analyzed by a portable imaging device (Fig. 1a, right side) previously described by Lu et al. as well as other lab members and collaborators [29,30,31,32]. The inner workings of the device can be seen in the paper by Lu et al., and we will describe them briefly here. The device consists of a CMOS camera (Raspberry Pi, Cambridge, UK), focusing lens (Thorlabs Inc., Newton, NJ, USA), Raspberry Pi computer board, and cassette tray all surrounded by a 3D-printed light-tight container. We used this device to image the test strips and send the images via Wi-Fi to a web application running on a mobile device such as a smartphone, tablet, or laptop computer, which could then be used to analyze the intensities of the test and control lines. The intensities of the test and control lines relative to the background color of the strip were determined using Python. The ratio of these intensities was taken as the signal and compared with the calibration curve to calculate a cortisol concentration.
2.9 Statistical analysis
We performed statistical analysis of the data using the R and Python programming languages. We explored population-level correlations between whole-day measures using linear mixed models with cortisol and melatonin as fixed effects and subject as a random effect. We used simple linear regression to assess relationships between whole-day measures of cortisol, PVT metrics, melatonin, and sleep for each participant. Significance of the regression slope estimates was determined by t test. We performed a residual analysis for each model to ensure that the model assumptions of normality and homogeneous variance of the error terms were met. We constructed multilevel linear models and determined the significance of the coefficients of the models by analysis of variance (ANOVA) using a likelihood ratio test. Significance in this analysis was defined as p < 0.05. Analysis of the quality of fit for both the calibration curve and the lateral flow analysis of the human samples was done in Python using an R-squared calculation.
3 Results
3.1 Test strip calibration
As described in Section 2.7, we created a calibration curve from saliva samples spiked to several concentrations. Each calibration sample was tested on three strips (except for the samples at 30 and 50 ng/ml, which were tested twice). An image of one of each of the calibration strips is shown in Fig. 2b. The test to control line intensity ratio for each of the strips was calculated and normalized to the mean of the test to control ratios of the 0 ng/ml strips and the mean and standard deviation for each concentration can be seen in Fig. 2a. To calculate a calibration curve, we used a 4-parameter logistic function fitted to the equation
In this function, test and control are the intensities of the respective lines (in arbitrary units), concentration is the known concentration of cortisol in the sample in ng/mL, and A, B, C, and D are curve fit parameters, where A = 0, B = 1.010, C = 7.104, and D = 2.408. The R-squared value of the data fitted to the calculated curve is 0.924.
3.2 Human sample testing and validation of test strip assay
We validated our test and calibration curve with 16 human samples at varying cortisol concentrations. Images of some human sample test strips can be seen in Fig. 3b. The test and control intensities of these images were used to calculate an estimated sample concentration (in ng/mL) according to the equation
The concentrations estimated by our test and those estimated by the ELISA kit can be seen compared in Fig. 3a. The R-squared value of the fitted data is 0.874. The point which was farthest from the line of best fit was only 2.7 ng/ml away, with 87.5% of the points falling within 2 ng/ml of the line of best fit and 62.5% of the points falling within 1 ng/ml of the line of best fit. The limit of detection for this test is 2.5 ng/ml. Our test can distinguish concentrations 2.5 ng/ml and higher from zero, with high accuracy in the range higher than 2.5 ng/ml. The lateral flow assay with human samples required less than 15 min to obtain a result, whereas the ELISA kit required more than 4 h per batch of samples.
3.3 Daily cortisol, melatonin, and PVT responses
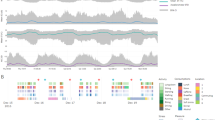
In our pilot study, we interviewed and recruited 12 participants, of whom only 10 (4 men and 6 women) were able to fully participate in all parts of the study. More details on compliance and sample viability can be found in the Supplementary Information. Sample concentrations for cortisol and melatonin were plotted against time since awakening in order to obtain the daily variations of cortisol and melatonin (Fig. 4a, b). Here, we defined “time of awakening” as the time reported by the participant for collection of the first saliva sample of the day, and we plotted all charts with “time of awakening” as 00:00 h. Representative data collected for a single participant (Participant 01) for cortisol levels, melatonin levels, and PVT median RT values are shown in Fig. 4.
Daily profiles of measured values for Participant 01. a Salivary cortisol profiles across 7 days. b Salivary melatonin profiles across 7 days. c Boxplot of PVT median reaction times (RTs) (binned by time across day) averaged over all days on which PVT was collected. Green lines represent median of bin and whiskers are at 1.5 times the interquartile range
Even though the specific daily profiles obtained varied notably between different participants, and across different days for the same participant, the general profiles followed expected trends. Cortisol was seen to peak in the morning, with a decrease observed across the day with minimum values achieved in later hours. The typical cortisol awakening response (CAR) was observed on 49.4% of days (i.e., cortisol levels in the second sample of day were higher than that in the first sample of the day), with time of peak cortisol varying between 30 and 45 min after awakening. Similarly, melatonin levels were seen to follow expected trends with low values in the morning, remaining flat for most of the day, and then rising sharply in the evening and peaking at night. Patterns in results for PVTs were not as evident in our data as were the patterns in cortisol and melatonin. The spread in the data was large, as evidenced by the large error bars in Fig. 4c.
3.4 Exploration of direct relationships between study parameters
In order to explore relationships between cortisol, melatonin, and PVT, we first used whole-day measures to express each of these parameters as a single metric for each day. Maximum cortisol was defined as the highest level of cortisol measured in each day, typically found within the first three samples of the day. Total cortisol was calculated by dividing the area under the daily cortisol profile by the duration (in hours) between the first and last sample of the day. Finally, the CAR was defined as the increase in cortisol from time of awakening to the peak level, which generally occurs between 30 and 45 min after awakening. For melatonin, we used the maximum value of melatonin for the day (generally from the last sample of the day). The whole-day measures for PVT surveys were the averages across the day for each of the session quantities (median RT, number of lapses per session, and number of false starts per session).
To examine relationships between the described whole-day measures of cortisol, alertness, melatonin, and sleep, we used a linear mixed model with fixed effects as either cortisol or melatonin and a random effect for subject-to-subject variation. No comparisons were found to have significant correlations. A complete list of the tests, their estimates, p values, and n values can be found in Supplementary Table 1.
Although a population-level analysis did not reveal strong relationships between cortisol, alertness, and melatonin, some individuals were found to show trends between the observed variables. Different individuals showed a large variability in both the magnitude and the sign of the slope (i.e., positive or negative correlation) between the examined variables (See Supplementary Figs. 2 and 3). However, most participants did not have statistically significant relationships between the variables, in part due to sparsity of data for each individual comparison. It is possible that this information may be useful in assessing whether sleep duration impacts a person’s average alertness and cortisol levels. For example, in this study, four participants out of nine were found to have a negative trend in total cortisol versus sleep length and a positive trend in total cortisol versus number of lapses. For these participants, this suggests that sleeping longer tends to coincide with a lower cortisol level and a lower cortisol level is related to higher alertness (lower number of lapses). Individuals’ relationships between melatonin, alertness, and sleep were also investigated and similar variability in trends is seen for melatonin, as in cortisol. (Slopes, p values, and n values for each individual and each parameter comparison can be found in the supplementary information (Supplementary Tables 2–7).)
3.5 Multilevel model for cortisol variation
In order to capture the effects of the different times, days, and participants from which we collected saliva samples, we used a hierarchical linear model that gives a better representation of how cortisol varies with time, day, and individual. This model, which was previously described by Hruschka et al. [28], allows cortisol to vary with time and allows variance beyond this to be attributed to different individuals and days. One individual’s cortisol levels can vary considerably between days, even when taken at the same time point after awakening [28]. Different individuals may also have different mean levels of cortisol and different rates at which cortisol decreases throughout the day [28]. These different types of variation, within-individual and between individuals, can be best captured by a multilevel model [28]. A detailed description of the formation of this model can be found in the Supplementary Information.
Our model takes the natural log of cortisol as a function of time since awakening. Each data point represents a sample obtained from a participant. The reference model is one in which the intercept (β0) and slope (β1) of the population may vary. The terms b1i and b0i allow for the slope and intercept, respectively, to vary for each individual. The term cij allows the intercept to vary depending on day, and the term εijk accounts for the residual error. The complete model equation is:
A graphical representation of the population data and mean, one individual’s data and mean (Participant 01), and 1 day’s data and mean (Participant 01, day 1) is shown in Fig. 5. The addition of each of the covariates (β0, β1, b0i, b1i, and cij) in the model was found to be significant (p < 0.001).
Plots depicting different levels in cortisol multilevel model. a All data points of ln(CORT) (Eqs. (1)–(3)) versus time since waking with population mean regression line. b Data points for Participant 01 shown with the population mean regression line and the Participant 01 mean regression line. c Data points for Day 1 of data for Participant 01 shown with the population mean regression line, the individual mean regression line, and the day mean regression line
After creating a model which captures variance of cortisol in terms of time, day, and individual, we then modified our statistical model to allow for alertness to contribute to the variation in each day. We included an additional covariate (d), here added as a fixed effect, which contained an average measure of alertness for each day in which both PVT and saliva samples were obtained. The equation for this model is then:
Average PVT median RT each day as well as average number of lapses each day was used as the PVT metric in this model. The addition of a term representing the average PVT median each day was not found to be significant (p = 0.286) and the addition of a term representing average number of lapses each day was only marginally significant (p = 0.078). Maximum melatonin from each day was added in a similar way, with the fixed effect of melatonin found not to be significant. When we attempted to add sleep parameters to the cortisol model, there was not enough data to resolve the model.
4 Discussion
Here, we have presented a novel system which has the power to collect and analyze saliva quantitatively for cortisol concentration. By utilizing easy-to-use saliva collection swabs, simple paper-based colorimetric lateral flow assays, and a portable and inexpensive test strip reader, we have created a system which can monitor the user’s cortisol in any setting. This system, which can interact with a smartphone or other mobile device, can be used in conjunction with our smartphone-based alertness monitoring. Because the range of cortisol concentration in saliva is relatively low (0–15 ng/ml, generally), it can be difficult to detect at the point of care. Our system’s use of a light-tight container with a custom lighting and optics setup allows us to measure with good accuracy relative to a traditional ELISA kit (R-squared = 0.874) throughout the range of common physiological concentrations. The limit of detection of our test is not as low as that of the ELISA (0.07 ng/ml); however, for personal cortisol monitoring, it would not be crucial to have that level of sensitivity. Our system can distinguish that the concentration is low (0–2.5 ng/ml) and can provide good quantitation above these concentrations.
Another point-of-care diagnostic developed by Zangheri et al. [12] has a lower reported limit of detection (0.3 ng/ml), due to the use of a chemiluminescent signal. The reported range of this assay is from 0.3 to 60 ng/ml, which is similar in utility to our detection range (2.5–30 ng/ml), because the typical salivary cortisol levels are less than 20 ng/ml. While this assay has a lower limit of detection, it also requires multiple user steps, including the use of a needle and syringe, and has a quantifiable signal that lasts for only 1 min. Our assay requires only the use of a swab, tube, disposable plastic capillary pipette, and dropper bottle of running buffer. While the detection of the other test is more sensitive, it is not practical or user-friendly. The times when cortisol quantification would be most crucial are during the CAR and in times of stress. During these times, cortisol concentration is generally greater than 2.5 ng/ml, and so our test would then be able to provide accurate results. Although our test may not have the precision to detect very small changes in cortisol (< 1 ng/ml), it can monitor a person’s diurnal cycle and detect high levels of cortisol during periods of stress.
The imaging device used in this work is a multi-purpose device which can be used to image virtually any lateral flow assay with a colorimetric signal. This device has been used by our lab for the analysis of other test strips measuring analytes in blood serum and whole blood [29,30,31,32]. In this work, we develop a novel immunoassay for cortisol measurement in saliva. The gold nanoparticles used as a marker in this assay can be imaged and analyzed by our imaging device in a manner similar to that of our previous work.
Saliva is known to have many components, including mucins, proteins, enzymes, and many other molecules and biological constituents [33]. While it is possible that these various components may interfere with the interactions taking place in our test, we took care when developing the calibration curve to use pooled human saliva samples with known concentrations below 0.5 ng/ml as the basis of all the tests. We then spiked these known near-zero samples to various concentrations to form the calibration curve, rather than using a spiked buffer solution. These tests, therefore, provide the closest approximation to the measured saliva samples and should, at least in part, take into account any interference that would be observed from saliva components in normal saliva samples. Further, as is standard for any salivary cortisol measurement, we requested that our participants not partake in any food or drink or brush their teeth for 30 min prior to taking saliva samples. This would prevent food particles, a change in saliva pH, or trace amounts of blood from impacting the results of the ELISA or the lateral flow strips. The cross-reactivity of the antibody is another possible source of interference in the test, and by examining the specifications given by the antibody manufacturer, we can see that the highest cross-reactivity exists with prednisolone at 4.9%, 11-deoxycortisol at 0.5%, and corticosterone at 0.3%. These are somewhat insignificant given the error present in our test, although whether or not a user is taking a corticosteroid such as prednisolone would be a factor to consider in understanding the results of the test.
Although the design of the system allows for good lighting and focus, each of the parts within the system is still able to be purchased inexpensively. The lateral flow assay itself has a materials’ cost of less than $1 per strip, and the portable imaging device is made up of off-the-shelf products and a 3-D-printed case totaling less than $400. Large-scale manufacturing of this device, without the use of 3-D printing, would likely greatly reduce the cost. A commercial cortisol ELISA kit, such as the one used in this study from Salimetrics, Inc., costs approximately $250 and can be used to analyze 38 saliva samples. Using an ELISA kit also requires expensive lab equipment and trained personnel, further adding to the cost of analysis. The cost of having a lab such as Salimetrics, Inc. analyze samples is over $14 per sample, which would add up quickly in large-scale analysis or even as an individual monitoring their own cortisol status. Also, while traditional laboratory methods generally take 4 h or more to get results about concentration of cortisol, our test takes less than 15 min. This allows us to have near-immediate results and measure samples as they are taken rather than waiting to run a large batch all at once. This type of result is ideal for personal monitoring in almost real time.
Although in this pilot study we were not able to definitively link salivary cortisol with PVT reaction times, there remains the possibility that monitoring both cortisol and alertness in more participants and for longer durations could reveal relationships. Our smartphone-based system would make a formal investigation easier and less expensive, and it would enable individuals to monitor their own natural rhythms and make decisions based on their body’s behavior. We discussed the possibility of a personalized monitoring system during exit interviews with the participants of our study. When asked whether they would try a system in which you must take saliva samples and alertness tests, but which would give you your own personal alertness schedule, four out of eight interviewed said that they would definitely try it, three said that they might try it, and only one said that they had no need for such a system. Only one participant had an issue with the invasiveness of the saliva collection, while the rest had no difficulties or problems with collecting a saliva sample via a swab. While the participants did not use the lateral flow assay part of the system, they reported that they were comfortable with the use of the saliva collection kit and PVT tests.
In our study, we collected information about participants’ cortisol, melatonin, alertness, and sleep while they went about their normal daily routine. After exploration of relationships between the measured variables, although we did not find correlations between whole-day measures for cortisol, alertness, and melatonin of the population, we found that the sign of the correlations (positive or negative) for each of the comparisons varied from individual to individual. If each individual does indeed have distinct relationships between their cortisol and alertness, our system would allow them to track these relationships and create a personalized record that could help them make better decisions about their sleep and work schedules. With our multilevel model, we could better classify the between- and within-individual variances, which allowed us to observe a marginal significance of PVT average number of lapses in accounting for variation in cortisol. Although the size of our study does not give us enough statistical power to prove a relationship, our finding that average number of lapses is marginally significant in predicting cortisol suggests that lower alertness is observed on days on which cortisol levels are higher. Further discussion of study results including compliance to study protocols and various types of analysis on the gathered data can be found in the Supplementary Information.
In conclusion, we have created a system which allows for individuals to monitor their own salivary cortisol and alertness levels. Each of the parts of our system is either inexpensive (lateral flow assay, portable reader) or devices that many people already own (smartphone, tablet, laptop). In this way, our system would open the door to personal monitoring of stress and alertness markers and make large-scale studies easier and less expensive. We have demonstrated our system’s use on human samples from a pilot study which analyzes the possibility of relationships between cortisol, melatonin, sleep, and alertness. Although we only found marginal significance in our pilot study results, they demonstrate the potential utility of our system in obtaining cortisol data from several subjects over an extended period of time.
Abbreviations
- HPA axis:
-
Hypothalamic-pituitary-adrenal axis
- CAR:
-
Cortisol awakening response
- PVT:
-
Psychomotor vigilance task
References
O’Connor TM, O’Halloran DJ, Shanahan F (2000) The stress response and the hypothalamic-pituitary-adrenal axis : from molecule to melancholia. Q J Med 93:323–333
McEwen BS (2004) Protection and damage from acute and chronic stress: allostastis and allostatic overload and relevance to the pathophysiology of psychiatric disorders. Ann N Y Acad Sci 1032:1–7
Shannon M, King TL, Kennedy HP (2007) Allostasis: a theoretical framework for understanding and evaluating perinatal health outcomes. JOGNN 36:125–134
Gold PW, Loriaux DL, Roy A, Kling MA, Calabrese JR, Kellner CH, Nieman LK, Post RM, Pickar D, Gallucci W, Avgerinos P, Paul S, Oldfield EH, Cutler GB Jr, Chrousos GP (1986) Responses to corticotropin releasing hormone in the hypocortisolism of depression and Cushing’s disease. N Engl J Med 314:1329–1335
Bailey SL, Heitkemper MM (2001) Circadian rhythmicity of cortisol and body temperature: morningness-eveningness effects. Chronobiol Int 18:249–261. https://doi.org/10.1081/CBI-100103189
Van Dongen HPA, Dinges DF (2005) Circadian Rhythms in Sleepiness, Alertness, and Performance. In: Kryger MH, Roth T, Dement WC (eds) Princ Pract Sleep Med. 4th ed. pp 435–443
Hellhammer DH, Wüst S, Kudielka BM (2009) Salivary cortisol as a biomarker in stress research. Psychoneuroendocrinology 34:163–171. https://doi.org/10.1016/j.psyneuen.2008.10.026
Ward Thompson C, Roe J, Aspinall P, Mitchell R, Clow A, Miller D (2012) More green space is linked to less stress in deprived communities: evidence from salivary cortisol patterns. Landsc Urban Plan 105:221–229. https://doi.org/10.1016/j.landurbplan.2011.12.015
Petrowski K, Wintermann G-B, Schaarschmidt M, Bornstein SR, Kirschbaum C (2013) Blunted salivary and plasma cortisol response in patients with panic disorder under psychosocial stress. Int J Psychophysiol 88:35–39. https://doi.org/10.1016/j.ijpsycho.2013.01.002
La Marca-Ghaemmaghami P, La Marca R, Dainese SM et al (2013) The association between perceived emotional support, maternal mood, salivary cortisol, salivary cortisone, and the ratio between the two compounds in response to acute stress in second trimester pregnant women. J Psychosom Res 75:314–320. https://doi.org/10.1016/j.jpsychores.2013.08.010
Yamaguchi M, Matsuda Y, Sasaki S, Sasaki M, Kadoma Y, Imai Y, Niwa D, Shetty V (2013) Immunosensor with fluid control mechanism for salivary cortisol analysis. Biosens Bioelectron 41:186–191. https://doi.org/10.1016/j.bios.2012.08.016
Zangheri M, Cevenini L, Anfossi L, Baggiani C, Simoni P, di Nardo F, Roda A (2015) A simple and compact smartphone accessory for quantitative chemiluminescence-based lateral flow immunoassay for salivary cortisol detection. Biosens Bioelectron 64:63–68. https://doi.org/10.1016/j.bios.2014.08.048
Carneiro D, Novais P, Augusto JC, Payne N (2017) New methods for stress assessment and monitoring at the workplace. IEEE Trans Affect Comput:1–1. https://doi.org/10.1109/TAFFC.2017.2699633
Umeda T, Hiramatsu R, Iwaoka T et al (1981) Use of saliva for monitoring unbound free cortisol levels in serum. Clin Chim Acta 110:245–253. https://doi.org/10.1016/0009-8981(81)90353-3
Dinges DF, Powell JW (1985) Microcomputer analyses of performance on a portable, simple visual RT task during sustained operations. Behav Res Methods Instrum Comput 17:652–655
Van Dongen HPA, Maislin G, Mullington JM, Dinges DF (2003) The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and Total sleep deprivation. Sleep 26:117–126
Kay M, Rector K, Consolvo S et al (2013) PVT-Touch: adapting a reaction time test for touchscreen devices. In: 7th Int. Conf. Pervasive Comput. Technol. Healthc. Work. Venice, Italy, pp 248–251
Wright KP Jr, Hull JT, Czeisler CA (2002) Relationship between alertness, performance and body temperature in humans. Am J Phys Regul Integr Comp Phys 283:R1370–R1377. https://doi.org/10.1152/ajpregu.00205.2002
Lamond N, Jay SM, Dorrian J, Ferguson SA, Roach GD, Dawson D (2008) The sensitivity of a palm-based psychomotor vigilance task to severe sleep loss. Behav Res Methods 40:347–352
Basner M, Dinges DF (2011) Maximizing sensitivity of the psychomotor vigilance test (PVT) to sleep loss. Sleep 34:581–591
Lieberman HR, Waldhauser F, Garfield G, Lynch HJ, Wurtman RJ (1984) Effects of melatonin on human mood and performance. Brain Res 323:201–207
Laakso M-L, Porkka-Heiskanen T, Alila A, Stenberg D, Johansson G (1990) Correlation between salivary and serum melatonin: dependence on serum melatonin levels. J Pineal Res 9:39–50
Voultsios A, Kennaway DJ, Dawsont D (1997) Salivary melatonin as a circadian phase marker: validation and comparison to plasma melatonin. J Biol Rhythm 12:457–466
Loh S, Lamond N, Dorrian J, Roach G, Dawson D (2004) The validity of psychomotor vigilance tasks of less than 10-minute duration. Behav Res Methods Instrum Comput 36:339–346
Basner M, Mollicone D, Dinges DF (2011) Validity and sensitivity of a brief psychomotor vigilance test (PVT-B) to total and partial sleep deprivation. Acta Astronaut 69:949–959. https://doi.org/10.1016/j.actaastro.2011.07.015
Basner M, Rubinstein J (2011) Fitness for duty: a 3 minute version of the psychomotor vigilance test predicts fatigue related declines in luggage screening performance. J Occup Environ Med 53:1146–1154
Chalder T, Berelowitz G, Pawlikowska T, Watts L, Wessely S, Wright D, Wallace EP (1993) Development of a fatigue scale. J Psychosom Res 37:147–153
Hruschka DJ, Kohrt BA, Worthman CM (2005) Estimating between- and within-individual variation in cortisol levels using multilevel models. Psychoneuroendocrinology 30:698–714. https://doi.org/10.1016/j.psyneuen.2005.03.002
Lu Z, O’Dell D, Srinivasan B, Rey E, Wang R, Vemulapati S, Mehta S, Erickson D (2017) A rapid diagnostic testing platform for iron and vitamin A deficiency. Proc Natl Acad Sci 114:13513–13518. https://doi.org/10.1073/pnas.1711464114
Srinivasan B, O’Dell D, Finkelstein JL, Lee S, Erickson D, Mehta S (2018) ironPhone: mobile device-coupled point-of-care diagnostics for assessment of iron status by quantification of serum ferritin. Biosens Bioelectron 99:115–121. https://doi.org/10.1016/J.BIOS.2017.07.038
Vemulapati S, Rey E, O’Dell D, Mehta S, Erickson D (2017) A quantitative point-of-need assay for the assessment of vitamin D3 deficiency. Sci Rep 7:14142. https://doi.org/10.1038/s41598-017-13044-5
Rey EG, O’Dell D, Mehta S, Erickson D (2017) Mitigating the hook effect in lateral flow sandwich immunoassays using real-time reaction kinetics. Anal Chem 89:5095–5100. https://doi.org/10.1021/acs.analchem.7b00638
Humphrey SP, Williamson RT (2001) A review of saliva: normal composition, flow, and function. J Prosthet Dent 85:162–169. https://doi.org/10.1067/mpr.2001.113778
Acknowledgements
A large portion of the work done for this paper was done in the Nanobiotechnology Center at Cornell University. Some of the equipment used in this work was located in the Kotlikoff Lab in the Cornell University College of Veterinary Medicine. Support for statistical analysis was provided by Lynn Johnson at the Cornell Statistical Consulting Unit.
Funding
This work was supported by the National Science Foundation [grant number CBET-1343058], the Robert Wood Johnson Health Data Exploration Agile Research Grant, and the Intel Science and Technology Center for Pervasive Computing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by Cornell University’s Institutional Review Board.
Electronic supplementary material
ESM 1
(PDF 580 kb)
Rights and permissions
About this article
Cite this article
Rey, E., Jain, A., Abdullah, S. et al. Personalized stress monitoring: a smartphone-enabled system for quantification of salivary cortisol. Pers Ubiquit Comput 22, 867–877 (2018). https://doi.org/10.1007/s00779-018-1164-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00779-018-1164-z