Abstract
Background
“Locomotive syndrome”, a concept proposed by the Japanese Orthopaedic Association (JOA), refers to risk conditions among the elderly population that may lead to the need for nursing care services. The association between osteoporosis (OP) or chronic musculoskeletal pain (CMSP) and the screening results of locomotive dysfunction identified by the GLFS-25 (a 25-question geriatric locomotive function scale) has not yet been adequately investigated.
Materials and Methods
Two hundred eighty-seven Japanese subjects were evaluated for locomotive dysfunction using the GLFS-25 and were also evaluated for their bone status by a quantitative ultrasound (QUS) assessment of the bone status (i.e., the measurement of the speed of sound (SOS) of the calcaneus). Furthermore, a questionnaire survey concerning CMSP persisting for 3 months or longer was given to those subjects. Statistical analyses were conducted to clarify the association between the bone status or CMSP and the screening results for locomotive dysfunction.
Results
The % young adult mean (%YAM) of the SOS was significantly lower among the 43 subjects with locomotive dysfunction identified by the GLFS-25 than in the 244 subjects without locomotive dysfunction (p < 0.001). Moreover, low back pain (p < 0.01), shoulder pain (p < 0.05) and knee pain (p < 0.001) were significantly more frequently observed in the 43 subjects with locomotive dysfunction than the 244 subjects without locomotive dysfunction. The screening results of the %YAM of the SOS was significantly associated with the population demonstrating locomotive dysfunction screened by the GLFS-25 based on the age-, gender- and BMI-adjusted analysis (OR 0.95, 95 % CI 0.91–0.98). Furthermore, the %YAM of SOS correlated with the GLFS-25 score (β = -0.212, p = 0.001). Furthermore, low back pain (OR 2.60, 95 % CI 1.29–5.24), shoulder pain (OR 2.16, 95 % CI 1.00–4.66), and knee pain (OR 2.97, 95 % CI 1.41–6.28) were found to be associated with locomotive dysfunction based on the results of the age-, gender- and a BMI-adjusted analysis.
Conclusions
The %YAM of the SOS was associated with the population demonstrating locomotive dysfunction which was identified using the GLFS-25, and the severity of locomotive dysfunction evaluated by the GLFS-25 was found to correlate with the %YAM of the SOS. Furthermore, low back pain, shoulder pain and knee pain were found to be associated with the screening results for locomotive dysfunction by the GLFS-25.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
“Locomotive syndrome”, a concept regarding locomotive dysfunction proposed by the Japanese Orthopaedic Association (JOA), refers to risk conditions among the elderly population, including muscle weakness, joint or spine disorders and osteoporosis (OP) that may lead to the need for nursing services [1–3].
The elderly population has been rapidly increasing in Japan in recent years, and the number of patients with OP and osteoarthritis (OA) is increasing [4]. Importantly, the contraction and progression of such diseases are known to often lead to locomotive dysfunction [5–8]. Therefore, epidemiologic studies investigating the possible causative relationships between these factors are awaited. Additionally, because musculoskeletal diseases are usually associated with chronic musculoskeletal pain (CMSP) [9–13], which is a common symptom in Japan [13–16] and results in a decreased quality of life (QOL) [17–24], the contribution of these conditions to locomotive function should also be investigated.
Regarding the evaluation tools for assessing locomotive dysfunction, Seichi et al. developed the GLFS-25, a 25-question geriatric locomotive function scale, and demonstrated that the GLFS-25 is a valid and reliable questionnaire scale for detecting the population with locomotive dysfunction in elderly Japanese individuals [25].
The aim of the present study was to clarify the associations between OP or CMSP and the population with locomotive dysfunction identified by the use of the GLFS-25 in the Japanese general population.
Materials and methods
In a mountain village located in the northern area of Gunma prefecture in Japan (Katashina village, population 4465 in 2014), local medical examinations for the general population have been held annually to screen for life-related diseases. The total number of subjects examined in 2013 was 1037. (1) A total of 581 individuals participated in musculoskeletal examinations and provided written informed consent. Of these subjects, (2) 416 of the 581 individuals underwent screening for locomotive dysfunction using the GLFS-25, (3) 317 of 416 individuals underwent a quantitative ultrasound (QUS) assessment of the bone status and speed of sound (SOS) of the calcaneus using a CM-200 densitometer (Furuno Electric, Nishinomiya City, Japan) [26], (4) 311 of 317 individuals completed a questionnaire regarding CMSP, (5) demographic variables and body mass index (BMI) data were recorded for 298 of 311 individuals and (6) 287 of 298 individuals were 40 years of age or older. Therefore, in this study, a total of 287 subjects (100 males and 187 females, average age 64.7 years, range 40–89 years) who satisfied all of the above categories were included in this study.
We divided the subjects into two populations based on the GLFS-25 score, the population with locomotive dysfunction and the population without locomotive dysfunction; specifically, if the GLFS-25 score was 16 or greater, the subjects were assigned to the population with locomotive dysfunction, and if the score was 15 or less, the subjects were assigned to the population without locomotive dysfunction [25]. The current cutoff score for identifying a population with locomotive dysfunction was determined to be 16 based on a receiver-operating characteristic curve analysis in that study [25]. Furthermore, a questionnaire concerning CMSP (neck pain, back pain, low back pain, shoulder pain, elbow or wrist pain, hip pain and knee pain) persisting for three months or longer [27], was given during the musculoskeletal examinations.
The associations between the bone status and the CMSP and GLFS-25 scores were statistically investigated.
This study was approved by the institutional review board of Gunma University.
Statistical analyses
Univariate analyses were performed using Welch’s t test, the Chi square test, and Fisher’s exact probability test. As important confounding factors for the bone status and CMSP, age, gender and BMI were considered in the logistic regression and multiple regression analyses, referring to previous papers [13, 15, 28–30], even if these parameters were not associated with locomotive dysfunction in the univariate analyses. A p-value of 0.05 was considered to be statistically significant. All statistical analyses were conducted using the IBM SPSS Statistics 19 software package (IBM Japan, Tokyo, Japan).
Results
Forty-three of the 287 (15.0 %) subjects were classified as belonging to the population with locomotive dysfunction based on the results of the GLFS-25 scores.
Table 1 shows the association between locomotive dysfunction screened by the GLFS-25 scores and age, gender, BMI, chronic musculoskeletal pain and bone status. According to an univariate analysis, the mean subject age was found to be significantly different between the population with locomotive dysfunction and the population without locomotive dysfunction (p < 0.01). Conversely, there were no significant differences between the population with locomotive dysfunction and the population without locomotive dysfunction with regard to gender and BMI.
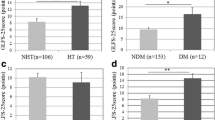
The %YAM) of the SOS was significantly lower among the individuals diagnosed with locomotive dysfunction according to the GLFS-25 (a score of 16 or greater) than in the individuals regarded as having a healthy locomotive function (score of 15 or less) (p < 0.001). Moreover, significant associations of low back pain (p < 0.01), shoulder pain (p < 0.05) and knee pain (p < 0.001) with locomotive dysfunction were observed in their cohort, whereas no significant associations were noted for neck pain, back pain, elbow or wrist pain or hip pain and locomotive dysfunction.
Table 2 shows the associations between CMSP and locomotive dysfunction based on the GLFS-25 score after adjusting for age, gender and BMI, while Table 2 also shows the associations between the bone status and locomotive dysfunction based on the GLFS-25 score after adjusting for age, gender and BMI.
In the logistic regression models, the %YAM of the SOS (OR 0.95, 95 % CI 0.91–0.98), low back pain (OR 2.60, 95 %CI 1.29–5.24), shoulder pain (OR 2.16, 95 % CI 1.00–4.66) and knee pain (OR 2.97, 95 % CI 1.41–6.28) were found to be factors significantly affecting the presence of locomotive dysfunction as identified based on the GLFS-25 scores.
In a single correlation analysis using Spearman’s correlation coefficient to assess the presence of associations between the measured variables and the GLFS-25 scores, age (r = 0.398, p < 0.001) was identified to be positively correlated with the GLFS-25 score and gender (r = −0.229, p < 0.001). In addition, the %YAM of the SOS (r = −0.317, p < 0.001) negatively correlated with the GLFS-25 score, whereas BMI did not significantly correlate with this parameter. Furthermore, a multiple regression model adjusted for age, gender and BMI showed a significant correlation between the %YAM of the SOS and the GLFS-25 score (β = −0.212, p = 0.001).
Discussion
OP has been reported to not only be a risk factor for fragility fractures [31], but also a major condition that leads to a decrease in the activities of daily living [18, 32]. Therefore, subjects with OP alone must also be considered to have “locomotive syndrome” based on the concept of “locomotive syndrome” proposed by the JOA [1–3].
In the present study, we demonstrated that a decreased %YAM of the SOS was associated with locomotive dysfunction as evaluated by the use of GLFS-25 scores, and the %YAM of the SOS correlated with the GLFS-25 score. Muramoto et al. showed that the %YAM of bone mineral density correlated with the GLFS-25 score, similar to the findings of the present study [33]. On the other hand, Muramoto et al. also reported that locomotive dysfunction identified using a cutoff score of 16 on the GLFS-25 was not associated with any differences in the bone mineral density [34], unlike that observed in this study. Because the subjects in the present study did not have any specific characteristics, including BMI, smoking habit, or alcohol habit, that is, the average BMI was 23.4 % and the rates of smoking and alcohol habits were 13.2 and 28.2 %, respectively [35], we speculate that the data of this cohort by and large reflect the general Japanese population. The varied results found between the previous study and the present study may be explained by differences in the age range of the subjects.
To date, the association between CMSP and locomotive dysfunction screened using the GLFS-25 score has not been adequately investigated [4, 33, 34]. In the present study, we demonstrated that low back pain, shoulder pain and knee pain are associated with locomotive dysfunction as identified by the use of the GLFS-25 scores. Based on these results, we speculate that preventing knee, lumbar and shoulder pathology is important for decreasing the number of patients with locomotive dysfunction.
There are some limitations associated with this study. First, this study is a cross-sectional study. Longitudinal studies are necessary to fully elucidate the associations between OP or CMSP and locomotive dysfunction. Second, we assessed the bone status using QUS, although measuring the bone mineral density via dual-energy X-ray absorptiometry is the gold standard for assessing OP [36]. However, it has been reported that the QUS parameters correlate with the bone mineral density [37, 38] and can be used to predict hip, wrist and non-spine fractures [39].
Third, the cause of CMSP could not be confirmed, because a detailed examination for the population with CMSP was not conducted in this study. Moreover, it may be possible that the recognition of each type of pain differs depending on the subject, because the area of CMSP was not clearly defined in this study. However, we believe that this study is, nevertheless, an important one, because the association between CMSP and locomotive dysfunction has not yet been sufficiently investigated.
In conclusion, we herein demonstrated that a poor bone status and CMSP were associated with locomotive dysfunction in 43 individuals within our cohort of 287 subjects.
Among the various types of CMSP, knee pain, low back pain and shoulder pain were more strongly associated with locomotive dysfunction. These results indicate that chronic pain in the lumbar, shoulder and knee areas may be important contributing factors for the etiology of locomotive dysfunction.
References
Nakamura K. The concept and treatment of locomotive syndrome: its acceptance and spread in Japan. J orthop Sci. 2011;16(5):489–91.
Nakamura K. A “super-aged” society and the “locomotive syndrome”. J Orthop Sci. 2008;13(1):1–2.
Nakamura K. Locomotive syndrome: disability-free life expectancy and locomotive organ health in a “super-aged” society. J Orthop Sci. 2009;14(1):1–2.
Yoshimura N, Muraki S, Oka H, Mabuchi A, En-Yo Y, Yoshida M, Saika A, Yoshida H, Suzuki T, Yamamoto S, Ishibashi H, Kawaguchi H, Nakamura K, Akune T. Prevalence of knee osteoarthritis, lumbar spondylosis and osteoporosis in Japanese men and women: the research on osteoarthritis/osteoporosis against disability study. J Bone Miner Metab. 2009;27(5):620–8.
Hirano K, Imagama S, Hasegawa Y, Ito Z, Muramoto A, Ishiguro N. The influence of locomotive syndrome on health-related quality of life in a community-living population. Mod Rheumatol. 2013;23(5):939–44.
Lawrence RC, Helmick CG, Arnett FC, Deyo RA, Felson DT, Giannini EH, Heyse SP, Hirsch R, Hochberg MC, Hunder GG, Liang MH, Pillemer SR, Steen VD, Wolfe F. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis Rheum. 1998;41(5):778–99.
Ohtori S, Ito T, Yamashita M, Murata Y, Morinaga T, Hirayama J, Kinoshita T, Ataka H, Koshi T, Sekikawa T, Miyagi M, Tanno T, Suzuki M, Aoki Y, Aihara T, Nakamura S, Yamaguchi K, Tauchi T, Hatakeyama K, Takata K, Sameda H, Ozawa T, Hanaoka E, Suzuki H, Akazawa T, Suseki K, Arai H, Kurokawa M, Eguchi Y, Suzuki M, Okamoto Y, Miyagi J, Yamagata M, Toyone T, Takahashi K. Evaluation of low back pain using the Japanese orthopaedic association back pain evaluation questionnaire for lumbar spinal disease in a multicenter study: differences in scores based on age, sex, and type of disease. J Orthop Sci. 2010;15(1):86–91.
Sasaki E, Ishibashi Y, Tsuda E, Ono A, Yamamoto Y, Inoue R, Takahashi I, Umeda T, Nakaji S. Evaluation of locomotive disability using loco-check: a cross-sectional study in the Japanese general population. J Orthop Sci. 2013;18(1):121–9.
Kitahara H, Ye Z, Aoyagi K, Ross PD, Abe Y, Honda S, Kanagae M, Mizukami S, Kusano Y, Tomita M, Shindo H, Osaki M. Associations of vertebral deformities and osteoarthritis with back pain among Japanese women: the Hizen-Oshima study. Osteoporos Int. 2013;24(3):907–15.
Muraki S, Akune T, Nagata K, Ishimoto Y, Yoshida M, Tokimura F, Tanaka S, Oka H, Kawaguchi H, Nakamura K, Yoshimura N. Association of knee osteoarthritis with onset and resolution of pain and physical functional disability: the ROAD study. Mod Rheumatol. 2014;24(6):966–73.
Muraki S, Oka H, Akune T, Mabuchi A, En-yo Y, Yoshida M, Saika A, Suzuki T, Yoshida H, Ishibashi H, Yamamoto S, Nakamura K, Kawaguchi H, Yoshimura N. Prevalence of radiographic lumbar spondylosis and its association with low back pain in elderly subjects of population-based cohorts: the ROAD study. Ann Rheum Dis. 2009;68(9):1401–6.
Nemoto O, Kitada A, Naitou S, Tsuda Y, Matsukawa K, Ukegawa Y. A longitudinal study of low back pain and radiological changes of lumbar spine in asymptomatic Japanese military young adults. Eur Spine J. 2013;22(2):453–8.
Yoshimura N, Akune T, Fujiwara S, Shimizu Y, Yoshida H, Omori G, Sudo A, Nishiwaki Y, Yoshida M, Shimokata H, Suzuki T, Muraki S, Oka H, Nakamura K. Prevalence of knee pain, lumbar pain and its coexistence in Japanese men and women: the longitudinal cohorts of motor system organ (LOCOMO) study. J Bone Miner Metab. 2014;32(5):524–32.
Graphical Review of Japanese Household: From Comprehensive survey of living conditions 2013. Tokyo: Statistics and Information Department, Minister’s Secretariat, Ministry of Health, Labour and Welfare; 2014.
Nakamura M, Nishiwaki Y, Ushida T, Toyama Y. Prevalence and characteristics of chronic musculoskeletal pain in Japan. J Orthop Sci. 2011;16(4):424–32.
Nakamura M, Nishiwaki Y, Ushida T, Toyama Y. Prevalence and characteristics of chronic musculoskeletal pain in Japan: a second survey of people with or without chronic pain. J Orthop Sci. 2014;19:339–50.
Hirano K, Imagama S, Hasegawa Y, Ito Z, Muramoto A, Ishiguro N. Impact of low back pain, knee pain, and timed up-and-go test on quality of life in community-living people. J Orthop Sci. 2014;19(1):164–71.
Kanis JA on behalf of the WHO Scientific Group. Assessment of osteoporosis at the primary health care level. Sheffield: WHO Collaborating Center for Metabolic Bone Disease; 2007.
Ministry of Health, Labour and Welfare. Outline of the results of National Livelihood Survey 2010. http://www.mhlw.go.jp/toukei/saikin/hw/k-tyosa/k-tyosa10/4-2.html.
Muraki S, Akune T, Oka H, En-yo Y, Yoshida M, Saika A, Suzuki T, Yoshida H, Ishibashi H, Tokimura F, Yamamoto S, Nakamura K, Kawaguchi H, Yoshimura N. Association of radiographic and symptomatic knee osteoarthritis with health-related quality of life in a population-based cohort study in Japan: the ROAD study. Osteoarthr Cartil. 2010;18(9):1227–34.
Muraki S, Akune T, Oka H, En-yo Y, Yoshida M, Saika A, Suzuki T, Yoshida H, Ishibashi H, Tokimura F, Yamamoto S, Nakamura K, Kawaguchi H, Yoshimura N. Impact of knee and low back pain on health-related quality of life in Japanese women: the research on osteoarthritis against disability (ROAD). Mod Rheumatol. 2010;20(5):444–51.
Muraki S, Akune T, Oka H, En-yo Y, Yoshida M, Saika A, Suzuki T, Yoshida H, Ishibashi H, Tokimura F, Yamamoto S, Nakamura K, Kawaguchi H, Yoshimura N. Health-related quality of life in subjects with low back pain in a population-based cohort study of Japanese men: the Research on Osteoarthritis Against Disability study. Spine. 2011;36(16):1312–9.
Muraki S, Oka H, Akune T, En-yo Y, Yoshida M, Suzuki T, Yoshida H, Ishibashi H, Tokimura F, Yamamoto S, Nakamura K, Kawaguchi H, Yoshimura N. Independent association of joint space narrowing and osteophyte formation at the knee with health-related quality of life in Japan: a cross-sectional study. Arthritis Rheum. 2011;63(12):3859–64.
Orimo H, Nakamura T, Hosoi T, Iki M, Uenishi K, Endo N, Ohta H, Shiraki M, Sugimoto T, Suzuki T, Soen S, Nishizawa Y, Hagino H, Fukunaga M, Fujiwara S. Japanese 2011 guidelines for prevention and treatment of osteoporosis executive summary. Arch Osteoporos. 2012;7(1–2):3–20.
Seichi A, Hoshino Y, Doi T, Akai M, Tobimatsu Y, Iwaya T. Development of a screening tool for risk of locomotive syndrome in the elderly: the 25-question geriatric locomotive function scale. J Orthop Sci. 2012;17(2):163–72.
Gluer CC. Quantitative ultrasound techniques for the assessment of osteoporosis: expert agreement on current status. J Bone Miner Res. 1997;12(8):1280–8.
Classification of chronic pain. Descriptions of chronic pain syndromes and definitions of pain terms. Harold Merskey and Nikolai Bogduk (eds). Prepared by the international association for the study of pain, Subcommittee on Taxonomy. Pain Supplement.1986, 3:S1-226.
Iizuka Y, Iizuka H, Mieda T, Tajika T, Yamamoto A, Takagishi K. Association between “loco-check” and EuroQol, a comprehensive instrument for assessing health-related quality of life: a study of the Japanese general population. J Orthop Sci. 2014;19(5):786–91.
Felson DT, Zhang Y, Hannan MT, Anderson JJ. Effects of weight and body mass index on bone mineral density in men and women: the Framingham study. J Bone Miner Res. 1993;8(5):567–73.
Yoshimura N, Oka H, Muraki S, Akune T, Hirabayashi N, Matsuda S, Nojiri T, Hatanaka K, Ishimoto Y, Nagata K, Yoshida M, Tokimura F, Kawaguchi H, Nakamura K. Reference values for hand grip strength, muscle mass, walking time, and one-leg standing time as indices for locomotive syndrome and associated disability: the second survey of the ROAD study. J Orthop Sci. 2011;16(6):768–77.
Osteoporosis prevention, diagnosis, and therapy. NIH Consens Statement 17:1–45.
Oka H, Yoshimura N, Kinoshita H, Saiga A, Kawaguchi H, Nakamura K. Decreased activities of daily living and associations with bone loss among aged residents in a rural Japanese community:the Miyama Study. J Bone Miner Metab. 2006;24(4):307–13.
Muramoto A, Imagama S, Ito Z, Hirano K, Ishiguro N, Hasegawa Y. Physical performance tests are useful for evaluating and monitoring the severity of locomotive syndrome. J Orthop Sci. 2012;17(6):782–8.
Muramoto A, Imagama S, Ito Z, Hirano K, Tauchi R, Ishiguro N, Hasegawa Y. Threshold values of physical performance tests for locomotive syndrome. J Orthop Sci. 2013;18(4):618–26.
Ministry of Health, Labour and Welfare. Outline of the National Health and Nutrition Survey Japan 2012. http://www.mhlw.go.jp/bunya/kenkou/eiyou/h24-houkoku.html.
Laugier P. An overview of bone sonometry. Int Congr Ser. 2004;1274:23–32.
Collinge CA, Lebus G, Gardner MJ, Gehrig L. A comparison of quantitative ultrasound of the calcaneus with dual-energy x-ray absorptiometry in hospitalized orthopaedic trauma patients. J Orthop Trauma. 2010;24(3):176–80.
Trimpou P, Bosaeus I, Bengtsson BA, Landin-Wilhelmsen K. High correlation between quantitative ultrasound and DXA during 7 years of follow up. Eur J Radiol. 2010;73(2):360–4.
Fujiwara S, Sone T, Yamazaki K, Yoshimura N, Nakatsuka K, Masunari N, Fujita S, Kushida K, Fukunaga M. Heel bone ultrasound predicts non-spine fracture in Japanese men and women. Osteoporos Int. 2005;16(12):2107–12.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify they have no commercial associations that might pose conflicts of interest in connection with this article.
About this article
Cite this article
Iizuka, Y., Iizuka, H., Mieda, T. et al. Population-based study of the association of osteoporosis and chronic musculoskeletal pain and locomotive syndrome: the Katashina study. J Orthop Sci 20, 1085–1089 (2015). https://doi.org/10.1007/s00776-015-0774-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00776-015-0774-9