Abstract
Background
There have been few reports on falls in patients who have undergone total hip arthroplasty (THA). In the present study, we aimed to investigate the incidence and circumstances of falls in post-THA patients and to identify the factors associated with falling.
Materials and methods
After excluding comorbidities, osteoarthritis without THA, and patients who had undergone THA within the previous 1 year, 214 patients [11 males, 203 females; mean (SD) age, 66.0 (8.7) years] living independently for at least 1 year after THA were analyzed as available data. Using a self-administered questionnaire, we investigated the number and circumstances of falls in the preceding year, as well as functional outcome and ambulatory ability via the Oxford Hip Score. Multivariate logistic regression analysis was used to identify factors influencing falls in post-THA patients.
Results
The incidence of at least one fall in the past year was 36 %. Falls were most often caused by tripping and falling forward during the daytime. In the present study, 37.7 % of falls resulted in injuries and 5.2 % resulted in fractures. Experience of fall was significantly related to medication [odds ratio (OR) 4.09, 95 % confidence interval (CI) 1.90–8.80, P < 0.001] and postoperative duration (OR 0.89, 95 % CI 0.81–0.98, P < 0.05).
Conclusions
Thus, patients have an increased risk for falls and fall-induced injuries after THA. Falls in post-THA patients are associated with medication and shorter postoperative duration. Therefore, it is essential to prevent falls in patients who have undergone THA, particularly during the early postoperative period and among patients administered medications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As the number of elderly people continues to increase, the number of fall-related injuries is also likely to increase [1]. Approximately a third of community-dwellers aged ≥65 years fall each year [2, 3]. In Japan, the incidence of falls among the elderly aged ≥65 years has been reported to be 15–25 % [4–7]. While about 25–60 % of falls result in injury, 5–10 % result in fracture [2–5]. Reducing the risks of morbidity and mortality from falls requires the prevention of falls in the elderly [1, 8].
One risk factor for falls in the elderly is lower limb arthritis [9, 10]. Patients with knee osteoarthritis (OA) who have undergone total knee arthroplasty (TKA) have an increased risk of falls compared with healthy elderly people [11, 12]. Hip OA is also a risk factor for falls, with about 40–45 % of patients with hip OA having fallen in the year prior to investigation [13, 14]. Particularly, patients with a new episode of hip pain had an increased occurrence of falls [14]. Jorgensen et al. [15] reported that the incidence of fall-related hospital admissions 90 days after fast-track TKA and total hip arthroplasty (THA) was 1.6 %. There have been few reports on falls in patients after THA, a common surgical treatment for severe hip OA.
Falls in post-THA patients may lead to serious injuries such as prosthetic joint dislocation and periprosthetic femoral fracture. This study aimed to investigate the incidence and circumstances of falls in post-THA patients and to identify factors associated with falling.
Materials and methods
Study design and participants
The present study was cross-sectional in design. Participants were community-dwellers who attended a lecture presented by a hip orthopedic special clinic for patients with hip OA and THA. Using advertising literature and oral announcements by staff members in the clinic, we recruited 381 individuals to participate. Patients who had completed ≥1 year post THA were included; those with neurological impairment, cardiovascular disease, rheumatoid arthritis, visual impairment, severe cognitive impairment, or dizziness were excluded. Healthy subjects, patients with hip OA without THA, patients after revision THA, and patients who had undergone THA within the previous 1 year were also excluded. The 214 remaining participants were carefully informed about the purpose and the risks and benefits of the present study and provided signed informed consent. This research was approved by the appropriate institutional ethics review board.
Characteristics
Participant characteristics were determined by self-administered questionnaire. Baseline information included age, sex, height, and body weight. Body mass index (BMI) was calculated as weight (kg)/square of height (m2). Medical information included the date of THA, THA side, revision THA, number of medications, and comorbidities. In participants with bilateral THA, the date of the most recent THA was used to calculate postoperative duration.
Fall assessment
Participants completed a standardized questionnaire recording the number and circumstances of falls in the past year. A fall was defined as an unexpected event in which the participants came to rest on the ground, floor, or a lower level [16]. The circumstances of falls included the location (e.g., indoors, outdoors, or on stairs), time (morning, daytime, or night), direction (forward, sideways, or backward), cause (slipping, tripping, loss of balance, hitting something, or giving way), and injury (none, wound, bruise, fracture, or dislocation of joint prosthesis). Falls due to extraordinary environmental factors (e.g., traffic accidents and falls while riding a bicycle) and dizziness were excluded from the count.
Functional outcome score
The Japanese version of the Oxford Hip Score (OHS) was used for the self-assessment of a patient’s disability after THA [17, 18]. The questionnaire contains 12 items: usual level of hip pain, trouble with washing and drying, trouble with transport, putting on socks/stockings/tights, doing household shopping alone, walking time before severe pain, difficulty in walking up the stairs, pain on standing up after sitting, limping when walking, sudden severe pain from the hip, work interference due to pain, and pain in bed at night. Each item is scored from 1 to 5, with 1 representing the least difficulty or severity and 5 representing the most difficulty or severity. The scores are then added to produce a single figure that can range from 12 (least difficult) to 60 (most difficult).
Ambulatory ability
Participants were asked, “Do you use a walking aid outdoors?” Participants were also asked to assess walking capacity as follows: “How much time can you walk without stopping?” [19]. Possible responses were over 1 h, over 30 min to less than 60 min, over 15 min to less than 30 min, less than 15 min, and almost none.
Statistical analysis
Data were organized using descriptive statistics. Baseline characteristics are expressed as mean [standard deviation (SD)]. Postoperative duration and OHS are expressed as median and interquartile range. Participants were classified as “fallers” or “non-fallers” based on the fall assessment data. The non-paired t test and Mann-Whitney U test were used to compare the differences between fallers and non-fallers for the following variables: age, height, body weight, BMI, OHS, and postoperative duration. The chi-square test was used to compare the differences between fallers and non-fallers for sex, medication, number of comorbidities, THA side, use of walking aids, and walking capacity. Multivariate logistic regression analysis was used to identify the factor or factors influencing falls in patients after THA. The dependent variable was experience of fall in the past year. Independent variables were age, sex, BMI, medications, comorbidities, bilateral THA, postoperative duration, OHS, use of a walking aid, and walking capacity. All statistical analyses were performed using JMP 8.0.2 (SAS Institute Inc., Cary, NC, USA) statistical software. Statistical significance was set at the level of P < 0.05.
Results
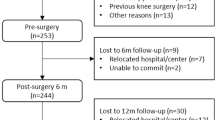
Of the 381 people approached, 359 (94.2 %) agreed to participate in the present study, of whom 214 post-THA patients were analyzed as available data and 145 were excluded from analysis (Fig. 1). In all participants, THA had been performed using a posterolateral approach by the same orthopedist between 1993 and 2010. The average age was 66.0 ± 8.7 (42–90) years.
Descriptive statistics of patient characteristics and the incidence of falls in the past year are shown in Table 1. The incidence of at least one fall in the past year was 36 %, and 21 participants (9.8 %) had fallen twice or more.
The circumstances of falls are shown in Table 2. More falls occurred indoors (53.2 %) than outdoors (42.9 %). Most falls occurred during the daytime (70.1 %). The most common direction of falls was forward (50.6 %). Tripping (48.1 %) was the primary cause of falls, followed by lost balance (28.6 %) and slipping (16.9 %). In total, 37.7 % of falls resulted in injuries, of which bruising was the most common, and 5.2 % of falls resulted in fractures. Almost all the fractures were Colles’ and rib fractures; there was no dislocation of prosthesis or periprosthetic femoral fracture.
Characteristics of fallers and non-fallers are shown in Table 3. There were significant differences between the two groups for age (P = 0.004), height (P = 0.037), medication (P < 0.001), comorbidities (P = 0.044), postoperative duration (P = 0.023), OHS (P < 0.001), use of a walking aid (P = 0.006), and walking capacity (P = 0.001).
Multivariate logistic regression analysis revealed that the experience of fall was significantly related to medication [odds ratio (OR) 4.09, 95 % confidence interval; CI 1.90–8.80, P < 0.001] and postoperative duration (OR 0.89, 95 % CI 0.81–0.98, P < 0.05) (Table 4).
Discussion
Here we report the incidence, circumstances, and risk factors of falls in patients after THA. Results of the present study indicate that 77 out of 214 post-THA patients (mean age, 66 years) had fallen at least once in the past year and that the incidence of falls was 36 %. Previous studies have reported the incidence of falls among the elderly (mean age, 73–74 years) in Japan to be 15–25 % [4–6]. Shimada et al. [7] showed that the incidence of falls in community-dwelling older people who had some physical disability and frailty was 21.8 %. Risk of falls in post-THA patients was higher than in the older and frail elderly people.
Our finding that more falls occurred indoors than outdoors was contradictory to the findings of other studies among the healthy elderly [4, 5]. Environmental factors are one of the risk factors for falls occurring indoors; thus, it is necessary to assess environmental risk factors for falls (e.g., bumps, slippery floors, unsuitable slippers, and hindrances such as electric cords present indoors). The most common time for falls was daytime (70.1 %), which is similar to the results of studies among the healthy elderly [4, 5]. The most common direction of falls was forward (50.6 %), followed by sideways (28.6 %) and backward (20.8 %). In the healthy elderly, the incidence of backward falls equaled that of forward falls; backward falls occur relatively frequently [20]. The most common cause of falls was tripping (48.1 %), followed by loss of balance (28.6 %); that is, about half of the falls in post-THA patients were the result of tripping and falling forward during walking. Falls in the healthy elderly are caused more by unstable legs [5] and loss of balance [20] than by tripping. In the present study, more fallers tripped than lost balance, which may be considered to be a characteristic cause in patients after THA.
In the present study, 37.7 % falls resulted in injuries and 5.2 % resulted in fractures, which is similar to the results of studies among the healthy elderly [4, 5]. Almost all the fractures were Colles’ and rib fractures; there were no periprosthetic femoral fractures. However, the number of THA procedures continues to rise annually, and the age of patients after THA is increasing, which may lead to an increase in periprosthetic femoral fractures. Measures should be devised and implemented to address this potential increase.
Comparison of the characteristics of fallers and non-fallers revealed that fallers had significantly higher OHS, higher rates of use of walking aids, and lower walking capacity than non-fallers; in other words, fallers had lower physical function and gait characteristics than non-fallers. Falls in post-THA patients may be associated with physical function and gait characteristics. However, objective outcomes of physical functions and gait characteristics were not evaluated in this study, and further investigations are necessary to clarify them.
Results of multivariate logistic regression analysis revealed that falling was associated with medication, which is consistent with research demonstrating that medication was associated with an increased risk of falls among the elderly [21–23]. Leipzig et al. [21] revealed an increased risk of falls among patients administered psychotropic medications, class 1A antiarrhythmic medications, digoxin, and diuretics. Robbins et al. [23] showed that administration of four or more medications was associated with falls. This study revealed that, as in the healthy elderly population, falls in post-THA patients were also associated with medication. Medications administered to post-THA patients should be evaluated in light of the risk of falling. However, the type and number of medications administered to post-THA patients in this study remain unknown, and further investigation is necessary.
Multivariate logistic regression analysis also revealed that shorter postoperative duration increased the risk of falling. Rubenstein et al. [24] showed that muscle weakness was the most common risk factor for falls in elderly people. Also, elderly people with lower limb arthritis [9] and patients after TKA [11] may be at increased risk of falling because of deficits in muscle strength and lower limb proprioception. In post-THA patients, impairments and functional limitations are reported to persist at 1 year after surgery [25, 26]. Sicard-Rosenbaum et al. [27] reported that lower extremity strength in patients about 2 years after THA was lower than that in healthy people. Muscle weakness may be one of the risk factors for falls among patients after THA. Thus, it is essential to consider the possibility of falls, particularly in the early postoperative period, during which physical function has not yet sufficiently recovered.
The incidence of falls was high, even at 5 years post THA in the present study, suggesting that the physical function of patients may remain inferior to those of healthy elderly people even at several years after THA. However, only a few studies have investigated the recovery of patients for more than 1 year after THA, and the long-term outcomes of THA remain unclear. Thus, the insufficient recovery of patients after THA may be overlooked. Therefore, further investigations are required to identify the long-term factors associated with falls in patients after THA.
The results of the present study suggest that patients have an increased risk for falls after THA and require preventive measures and continuous rehabilitation to prevent falls. In particular, during the early postoperative period, certain modifications should be made in the patients’ houses. Furthermore, they should be careful to avoid tripping, have their medications adjusted, and use walking aids.
A limitation of the present study is its cross-sectional design, which does not allow changes in the incidence of falls before and after THA or detailed risk factors for falls to be determined. Another is that our results were compared with those of similar previous studies among the elderly rather than directly compared with those of a control group. Finally, the present study is an investigation by self-administered questionnaire; objective outcomes of physical functions and gait characteristics were not evaluated. Prospective observational studies of falling before and after THA are needed to clarify the relationships among physical functions, gait characteristics, and the incidence of falls and to reveal the risk factors for falls in patients after THA.
Conclusion
In the year following THA, 36 % of patients fell at least once. Approximately 50 % of falls were caused by tripping and falling forward. Approximately 40 % of falls resulted in injuries and approximately 5 % resulted in fractures. Falls in post-THA patients were associated with medications and shorter postoperative duration. After THA, patients require preventive measures and continuous rehabilitation to prevent falls. In particular, during the early postoperative period, patients at increased risk for falls should be provided with environmental modifications to their homes, medication adjustments, and walking aids.
References
Kannus P, Parkkari J, Koskinen S, Niemi S, Palvanen M, Jarvinen M, Vuori I. Fall-induced injuries and deaths among older adults. JAMA. 1999;281(20):1895–9.
Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319(26):1701–7.
Campbell AJ, Borne MJ, Spears GF, Jackson SL, Brown JS, Fitzgerald JL. Circumstances and consequences of falls experienced by a community population 70 years and over during a prospective study. Age Ageing. 1990;19(2):136–41.
Yasumura S, Haga H, Niino N. Circumstances of injurious falls leading to medical care among elderly people living in a rural community. Arch Gerontol Geriatr. 1996;23(2):95–109.
Aoyagi K, Ross PD, Davis JW, Wasnich RD, Hayashi T, Takemoto T. Falls among community-dwelling elderly in Japan. J Bone Miner Res. 1998;13(9):1468–74.
Yamada M, Nishiguchi S, Fukutani N, Tanigawa T, Yukutake T, Kayama H, Aoyama T, Arai H. Prevalence of sarcopenia in community-dwelling Japanese older adults. J Am Med Dir Assoc. 2013;14(12):911–5.
Shimada H, Suzukawa M, Tiedemann A, Kobayashi K, Yoshida H, Suzuki T. Which neuromuscular or cognitive test is the optimal screening tool to predict falls in frail community-dwelling older people? Gerontology. 2009;55(5):532–8.
Hill K, Schwarz J, Flicker L, Carroll S. Falls among healthy, community-dwelling, older women: a prospective study of frequency, circumstances consequences and prediction accuracy. Aust NZ J Public Health. 1999;23(1):41–8.
Sturnieks DL, Tiedemann A, Chapman K, Munro B, Murray SM, Lord SR. Physiological risk factors for falls in older people with lower limb arthritis. J Rheumatol. 2004;31(11):2272–9.
Leveille SG, Jones RN, Kiely DK, Hausdorff JM, Shmerling RH, Guralnik JM, Kiel DP, Lipsitz LA, Bean JF. Chronic musculoskeletal pain and the occurrence of falls in an older population. JAMA. 2009;302(20):2214–21.
Levinger P, Menz HB, Wee E, Feller JA, Bartlett JR, Bergman NR. Physiological risk factors for falls in people with knee osteoarthritis before and early after knee replacement surgery. Knee Surg Sports Traumatol Arthrosc. 2011;19(7):1082–9.
Matsumoto H, Okuno M, Nakamura T, Yamamoto K, Hagino H. Fall incidence and risk factors in patients after total knee arthroplasty. Arch Orthop Trauma Surg. 2012;132(4):555–63.
Arnold CM, Faulkner RA. The history of falls and the association of the timed up and go test to falls and near-falls in older adults with hip osteoarthritis. BMC Geriatr. 2007;4(7):17.
Nahit ES, Silman AJ, Macfarlane GJ. The occurrence of falls among patients with a new episode of hip pain. Ann Rheum Dis. 1998;57(3):166–8.
Jogensen CC, Kehlet H. Lundbeck Foundation Centre for Fast-track Hip and Knee Replacement Collaborative Group. Fall-related admissions after fast-track total hip and knee arthroplasty—cause of concern or consequence of success? Clin Interv Aging. 2013;8:1569–77.
Lamb SE, Jorstad-Stein EC, Hauer K, Becker C. Development of a common outcome data set for fall injury prevention trials: the prevention of falls network Europe consensus. J Am Geriatr Soc. 2005;53(9):1618–22.
Dawson J, Fitzpatrick R, Carr A, Murray D. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg Br. 1996;78(2):185–90.
Uesugi Y, Makimoto K, Fujita K, Nishii T, Sakai T, Sugano N. Validity and responsiveness of the Oxford hip score in a prospective study with Japanese total hip arthroplasty patients. J Orthop Sci. 2009;14(1):35–9.
Remerand F, Le Tendre C, Baud A, Couvret C, Pourrat X, Favard L, Laffon M, Fusciardi J. The early and delayed analgesic effects of ketamine after total hip arthroplasty: a prospective, randomized, controlled, double-blind study. Anesth Analg. 2009;109(6):1963–71.
Hwang HF, Lee HD, Huang HH, Chen CY, Lin MR. Fall mechanisms, bone strength, and hip fractures in elderly men and women in Taiwan. Osteoporos Int. 2011;22(8):2385–93.
Leipzig RM, Cumming RG, Tinetti ME. Drugs and falls in order people: a systematic review and meta-analysis: I. psychotropic drugs. J Am Geriatr Soc. 1999;47(1):30–9.
Haritikainen S, Lonnroos E, Louhivuori K. Medication as a risk factor for falls: critical systematic review. J Gerontol A Biol Sci Med Sci. 2007;62(10):1172–81.
Robbins AS, Rubenstein LZ, Josphson KR, Schulman BL, Osterweil D, Fine G. Predictors of falls among elderly people: results of two population-based studies. Arch Intern Med. 1989;149(7):1628–33.
Rubenstein LZ, Josephson KR. The epidemiology of falls and syncope. Clin Geriatric Med. 2002;18(2):141–58.
Vissers MM, Bussmann JB, Verhaar JA, Arends LR, Furlan AD, Reijman M. Recovery of physical functioning after total hip arthroplasty: systematic review and meta-analysis of the literature. Phys Ther. 2011;91(5):615–29.
Ewen AM, Stewart S. St Clair Gibson A, Kashyap SN, Caplan N. Post-operative gait analysis in total hip replacement patients: a review of current literature and meta-analysis. Gait Posture. 2012;36(1):1–6.
Sicard-Rosenbaum L, Light KE, Behrman AL. Gait, lower extremity strength, and self-assessed mobility after hip arthroplasty. J Gerontol A Biol Sci Med Sci. 2002;57(1):M47–51.
Acknowledgments
We would like to thank the patients who kindly agreed to participate. We are grateful to Keiichi Tagomori and Namika Miura for their help and support.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Ikutomo, H., Nagai, K., Nakagawa, N. et al. Falls in patients after total hip arthroplasty in Japan. J Orthop Sci 20, 663–668 (2015). https://doi.org/10.1007/s00776-015-0715-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00776-015-0715-7