Abstract
Background
Central obesity has been proved to be a strong risk factor for numerous health-related problems as well as mortality. However, there have been no studies on the relationship between central obesity and locomotive syndrome (LS). The present study investigated the influence of central obesity on LS.
Methods
A total of 217 females between the ages of 60 and 79 years (mean 68.2 ± 5.0 years) who completed the questionnaires, physical examination and physical performance tests in the Yakumo study in 2011–2012 were enrolled in this study. Participants were assessed according to the 25-Question Geriatric Locomotive Function Scale (GLFS-25), visual analog scale (VAS) for lower back pain (LBP) and knee pain, and the Roland Morris Disability Questionnaire (RDQ). LS was defined as having a score of >16 points on the GLFS-25. Height, weight, waist circumference (WC), hip circumference, % body fat and bone mineral density were measured. Body mass index and waist-to-hip ratio were calculated. The timed up-and-go test, one-leg standing time with eyes open, 10-m gait time and maximum stride were assessed. Back muscle strength and grip strength were measured. The relationships between obesity-related parameters and GLFS-25, RDQ, VAS and physical performance tests were analyzed.
Results
The GLFS-25, LBP and knee pain showed significant correlation with most of obesity-related parameters. Among obesity-related parameters, WC was most strongly related to the GLFS-25, LBP and knee pain. When participants were stratified by WC, larger WC was significantly associated with a higher GLFS-25 score, higher prevalence of LS and higher VAS for LBP and knee pain as well as poorer results in some physical performance tests even after adjustment by age.
Conclusions
The present study revealed that central obesity is significantly associated with LS, and WC can be a useful parameter to assess the risk of LS in elderly women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the past few decades, advances in medicine and public health, improved living standards and greater educational attainment have contributed to huge reductions in mortality worldwide. Now the importance of healthy aging is increasingly recognized. Healthy life expectancy (HALE) is the number of years that a person at a given age can expect to live in good health taking into account the age-specific mortality, morbidity and functional health status [1]. The HALE in Japan in 2010 was reported to be the highest in both sexes among 187 countries [2]. However, health care costs spent for disability in the elderly is still a large national burden. Since orthopedic problems, including joint diseases, osteoporosis and spinal disorders, are the main reasons for disability in the elderly, measures to prevent disabilities of the locomotive organs are urgently needed.
In 2007, the Japanese Orthopedic Association (JOA) proposed the term locomotive syndrome (LS) to designate middle-aged and elderly people at high risk of requiring nursing care because of problems with their locomotive organs [3]. Recently, a precise quantitative diagnostic tool called the 25-Question Geriatric Locomotive Function Scale (GLFS-25) has been developed to measure the degree of LS affecting an individual, and its validity and reliability have been confirmed [4]. The concept of locomotive syndrome is now increasingly recognized, but the risk factors for LS have not been fully investigated. Understanding factors that contribute to disability and functional decline in an aging population has enormous public health value.
Central obesity has been shown to be a predictor of mortality in the general population [5]. Waist circumference (WC) is an effective surrogate measure for central obesity, which demonstrates a strong relationship with increased risk for numerous health outcomes as well as mortality [6]. There is increasing evidence that central obesity may be more important than the overall body mass index (BMI) [7]. Despite the importance of measuring central obesity in health research, few epidemiological studies have evaluated indicators of central obesity in relation to functional disability in elderly populations [8].
We hypothesized that central obesity may also substantially influence LS since previous studies have shown that central obesity is associated with some strong indicators of LS: knee pain, lower back pain (LBP) and poorer physical function [9, 10]. The purpose of this study is to investigate the influence of central obesity as defined by waist circumference on LS, knee pain, LBP and physical performance in elderly women.
Participants and methods
The subjects were healthy Japanese volunteers who attended a basic health checkup supported by the local governments in 2011 and 2012. This checkup has been held annually in the town of Yakumo (population: 18,896 in 2010) for 31 years (Yakumo Study) and comprises voluntary orthopedic and physical function examinations as well as internal medical examinations and psychological tests.
The current study involved 217 female volunteers aged between 60–79 years (mean 68.2 ± 5.0 years). The inclusion criteria for this study were defined as follows: (1) age 60–79 years; (2) individuals who answered all questions on the GLFS-25 and VASs; (3) individuals who were informed of this study and consented to participate; (4) individuals who were able to complete all of the six physical performance tests. Individuals who had severe disability in walking or standing or any dysfunction of the central or peripheral nervous systems were excluded. In 2012, the volunteers who had participated in the physical performance tests in 2011 were excluded from the study in order to avoid the overlap of the same participants.
The severity of the LS was evaluated using the GLFS-25 score [4]. Extent of knee and lower back pain was assessed using a visual analog scale (VAS) of 10 cm from no pain to the worst possible pain. The averaged values of the VAS of the right and left knees were used for knee pain. Physical function tests included one-leg standing time with eyes open, TUG, 10-m gait time, maximum stride back muscle strength and grip strength. The study protocol was approved by the Committee on Ethics in Human Research of Nagoya University.
25-Question Geriatric Locomotive Function Scale (GLFS-25)
The GLFS-25 is self-administered, but it is relatively comprehensive consisting of 25 items graded on a 5-point scale from no impairment (0 points) to severe impairment (4 points) [4]. Added together, there is a total possible score of 0–100 with a higher number indicating a greater severity of LS. The validity and reliability of this new measurement were confirmed as satisfactory with a cutoff score for identifying LS set at 16 points. We diagnosed participants with GLFS-25 of 16 points or greater as having LS and those with 15 points or less as non-LS. All physical performance tests were conducted using the same methods as we reported previously [11].
Timed up-and-go test (TUG)
We measured the time it took a subject to rise from a standard chair (46-cm seat height), walk a distance of 3 m, turn around, walk back to the chair and sit down. Each subject performed the test two times, both at maximum pace, and the mean score was used for analyses.
One-leg standing time with eyes open (OLS)
One-leg standing time with eyes open was measured twice for each leg. Timing of the test spanned from when the subject raised his/her leg until the leg was set back down on the floor up to a maximum of 60 s. We recorded the average value of the four measurements (two trials on each leg).
Back muscle and grip strength
We examined back muscle strength as the maximal isometric strength of the trunk muscles in a standing posture with 30° lumbar flexion using a digital back muscle strength meter (T.K.K. 5102, Takei Co., Japan) making one measurement. We tested grip strength in a standing position once on each hand using a Toei Light handgrip dynamometer (Toei Light Co., Ltd., Saitama, Japan). The average value was used to characterize the subject's grip strength.
Ten-meter gait time
We evaluated the 10-m gait time as a reflection of subjects’ mobility. Walking time was the time required to complete a 10-m straight course. All participants walked the 10-m course once at their fastest pace.
Maximum stride
Maximum stride was measured from a standing position. Participants placed their right feet forward as far as possible and then brought their left feet up to the right feet without touching their hands to the floor or to their knees. This was repeated with the left foot forward. The average value divided by the participant’s height was used to characterize the subject's maximum stride.
Measurement of BMD and % of body fat
BMD was measured in the calcaneus using a bone densitometer (A1000 Insight, Lunar Corporation, WI, USA). The % fat was measured using a body fat meter (TBF-305, Tanita, Japan).
WC, HC and WHR
WC was measured at the level of the umbilicus (i.e., belly button) at the end of gentle expiration, and the hip circumference (HC) was measured at the widest trochanters with the subject standing using a non-stretchable measuring tape and recorded in centimeters to the nearest millimeter. Waist-to-hip ratio (WHR) was calculated by dividing the WC by the HC.
Statistical analysis
Differences in demographic variables between the groups were determined using the Mann–Whitney U test. Partial correlations between physique-related variables and GLFS-25, LBP, knee pain and RDQ were assessed using Pearson’s correlation coefficients adjusted by age. Partial correlations between physique-related variables and the outcome of physical performance tests were assessed using Pearson’s correlation coefficients adjusted by age. Prevalence of LS among groups stratified by WC was assessed using the Mantel–Haenszel test. Multivariate logistic regression analysis was performed to evaluate the age-adjusted significance between the prevalence of LS and WC strata. A general linear model was used to evaluate the age-adjusted significance between WC strata and GLFS-25, VAS for pain and the result of physical performance tests. We considered probability values of less than 0.05 as statistically significant. SPSS version 20.0 for Windows (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses.
Results
There were 217 subjects: 36 females were defined as having LS (LS group) and 181 females did not have LS (non-LS group). The subjects’ demographics, questionnaire results and physical performance tests are listed in Table 1. We compared physique-related parameters between the non-LS and LS groups (Table 2). There were significant differences in age, height, BMI, WC and HC between the two groups. WC and WHR remained significantly larger in the LS group than in the non-LS group even after physique-related variables had been adjusted by age.
We evaluated age-controlled correlations between physique-related variables and GLFS-25 scores, LBP and knee pain. GLFS-25 score, LBP and knee pain correlated with most of the obesity-related parameters, and WC was most strongly related to the GLFS-25 score, LBP and knee pain (Table 3).
We also evaluated age correlations between physique-related variables and the outcomes of physical performance tests (Table 4). One-leg standing time (OLS), timed up-and-go (TUG), 10-m walking time and maximum stride correlated significantly with most of the obesity-related parameters, but back muscle strength and grip strength did not. Age-controlled correlation of BMI, WC, HC and % body fat with these physical performance tests were relatively strong.
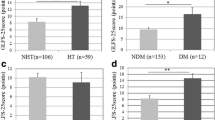
We stratified the participants into three groups with equal numbers of people (G1, G2 and G3) according to increasing WC; participants in G1 had the smallest WC, and participants in G3 had the largest WC. Mean, SD and range of WC in each group are shown in Table 5. The cutoff measurements between G1 and G2 and between G2 and G3 happened to be just 70 and 80 cm, respectively. Prevalence of people with LS was higher as WC increased (8 % in G1, 20 % in G2 and 27 % in G3). Larger waist stratum was a significant risk factor for having LS in the age-adjusted multivariate logistic regression model (p < 0.01). WC was also significantly associated with GLFS-25 scores and the VAS for LBP and knee pain even after adjustment by age (Fig. 1a, b, c). WC was also significantly associated with some physical performance tests: 10-m gait time and TUG as well as OLS, even after adjustment by age (Fig. 2a, b, c). However, there was no significant trend in maximum stride, back muscle strength and grip strength with WC strata (Fig. 2d, e, f).
a Mean age-adjusted GLFS-25 score in each waist stratum. b Mean age-adjusted visual analog scale for knee pain in each waist stratum. c Mean age-adjusted visual analog scale for lower back pain in each waist stratum. Participants were stratified into three groups (G1, G2 and G3) with equal numbers of patients according to waist circumference (Table 5). Error bar indicates standard error of the mean. *p < 0.05; **p < 0.01; ***p < 0.001
a Mean age-adjusted 10-m gait time in each waist stratum. b Mean age-adjusted timed up-and-go test in each waist stratum. c Mean age-adjusted one-leg standing time in each waist stratum. d Mean age-adjusted maximum stride in each waist stratum. e Mean age-adjusted back muscle strength in each waist stratum. f Mean age-adjusted grip strength in each waist stratum. Participants were stratified into three groups (G1, G2 and G3) with equal numbers of patients according to waist circumference (Table 4). Error bar indicates standard error of the mean. *p < 0.05; **p < 0.01; ***p < 0.001
Discussion
Some reports identifying the risk factors for LS have been reported. The incidence of LS is significantly higher in women than in men, and it increases with age [11, 12]. We also found that knee pain and LBP are significant risk factors for LS [11]. Radiographic knee OA was also reported to be a risk factor for LS [12]. However, there have been no reports on the relationship between LS and physique-related parameters.
Central obesity is drawing more attention as a risk factor for many health problems such as hypertension, atherosclerosis and type 2 diabetes [13, 14]. However, few studies have attempted to elucidate the relationship between central obesity and dysfunction of locomotive organs [15]. This is the first study to investigate the relationship between central obesity and LS.
Previously, we reported that knee and LBP and some physical performance tests are significantly associated with LS. In that study, physique-related parameters showed relatively weak correlations with the GLFS-25 score, so we did not analyze them thoroughly. Although physique-related parameters are not as strongly related to the GLFS-25 score as are knee pain, LBP and some of the physical performance tests, some of them have weak but significant correlations with the GLFS-25. WC was found to have a better correlation with the GLFS-25 score than other obesity-related parameters. A possible mechanism whereby WC could be the most predictive marker of obesity risk may be through its ability to reflect the size of abdominal fat deposits. WC has been shown to correlate with the amount of fat in the abdomen as measured by magnetic resonance imaging (MRI) and computed tomography (CT) [16, 17].
The main achievement of this study is that we not only demonstrated the association between obesity-related parameters and LS, but also identified WC as a better marker for the severity of LS. WC and WHR were significantly larger in the LS group than in the non-LS group, while weight and BMI were not. Moreover, WC and WHR correlated significantly with the GLFS-25 score.
Being overweight is known to adversely affect activities of daily living (ADL) and health-related quality of life (HRQL) [18, 19]. However, some researchers insist that central obesity is more directly related to self-reported disability [20]. There are several established limitations in using BMI as a measure of obesity [21], and BMI may not be a good indicator of obesity in the elderly population because of the disproportional loss of lean body mass. The result of our study supports these previous reports.
The parameters of central obesity also significantly correlated with knee pain and LBP in our study. Obesity as defined by BMI is a well-know factor in knee OA and knee pain [22, 23]. There are many fewer studies on central obesity and knee pain [9]. However, our study revealed central obesity to be a risk factor for knee pain, and the results suggest that WC may be a better indicator of knee pain than other obesity-related parameters.
The association between LBP and obesity is more controversial. A remarkable number of studies have been published attempting to address the nature of the relationship between LBP and overweight/obesity, but most of them failed to provide conclusive evidence. Systematic reviews also conclude that there is insufficient evidence for a causal link between body weight and LBP and that obesity should be considered a possible weak risk indicator for LBP [24]. Although only a few studies have investigated the association between central obesity and LBP using WC or WHR as parameters, they showed significant associations between them [25]. Our study is in accordance with their findings. Central obesity defined by WC or WHR may prove to be an independent risk factor for LBP in a larger scale study in the future. Since LBP and knee pain are significant risk factors for LS [11], the correlation between central obesity and LS may be partly due to LBP and knee pain.
Obesity is known to have a significant impact on physical performance [26]. However, data are sparse on measured functional limitations rather than self-reported limitations and for markers of obesity other than BMI. In this study, several obesity-related parameters had significant associations with some physical performance tests supporting those previous studies. Several studies bear out the relationship between quickness and obesity [27]. Balancing ability is also known to be influenced by obesity [28]. WC also correlates with tests for balance [15]. However, back muscle strength and grip strength were not significantly correlated with most of the obesity-related parameters in the current study. The relationship between BMI and grip strength was less consistent in a previous study [29]. A person must exert power to move, balance and support the body’s weight in one-leg standing time, TUG, 10-m gait time and maximum stride tests. On the other hand, body weight is not a burden on back muscle strength and grip strength. Therefore, it is not surprising that obesity influenced the strength tests differently than other tests in the current study. To summarize, obesity had a significant relationship to the results of physical performance tests. However, we did not find central obesity-related parameters (WC, WHR) to be superior to general obesity-related parameters (weight, BMI, % body fat) in the relationship to physical performance tests. Further study is needed to address this issue.
Weight reduction is reported to have positive effects on musculoskeletal pain, both perceived disability and observed functional limitations, and health-related QOL [30], but there have been no studies looking at the effect of weight reduction on LS. The result of our study clearly showed that central obesity is associated with LS, and this suggests that reducing WC may help lower GLFS-25 scores and improve ADL and QOL. Diet aimed at weight and WC reduction together with physical exercise may show better results than anti-LS training alone. A prospective interventional study is required to test this hypothesis.
There are some important strengths of our study. First, although most previous studies have been based only on self-reported disability, we confirmed our results using well-validated physical performance tests for mobility, balance and strength. Second, we used as many as six obesity-related parameters, weight, BMI, WC, HC, WHR and % body fat, in order to thoroughly investigate the relationship between LS and obesity.
This study also had limitations. First, the number of participants is relatively small, and their degrees of obesity and ADL impairment were mild. Nevertheless, we demonstrated a significant relationship between abdominal obesity and LS in this study; a larger study in the future may elucidate a stronger association. Second, this study did not include males because there were fewer male attendants and because a smaller percentage of males have LS. Another study is needed on the question of central obesity and LS in males.
In summary, WC is significantly associated with LS as defined by the GLFS-25, and its association was more significant than other obesity-related parameters. WC also had a significant relationship with knee pain, lower back pain and the results of physical performance tests. The findings of this study suggest that central obesity is associated with disability, and they support the use of WC to assess the risk of LS in elderly females.
References
Robine JM, Ritchie K. Healthy life expectancy—evaluation of global indicator of change in population health. British Med J. 1991;302:457–60.
Salomon JA, Wang H, Freeman MK, Vos T, Flaxman AD, Lopez AD, Murray CJL. Healthy life expectancy for 187 countries, 1990–2010: a systematic analysis for the Global Burden Disease Study 2010. Lancet. 2012;380:2144–62.
Nakamura K. A “super-aged” society and the “locomotive syndrome”. J Orthop Sci. 2008;13:1–2.
Seichi A, Hoshino Y, Doi T, Akai M, Tobimatsu Y, Iwaya T. Development of a screening tool for risk of locomotive syndrome in the elderly: the 25-Question Geriatric Locomotive Function Scale. J Orthop Sci. 2012;17:163–72.
Petursson H, Sigurdsson JA, Bengtsson C, Nilsen TIL, Getz L. Body configuration as a predictor of mortality: comparison of five anthropometric measures in a 12 year follow-up of the norwegian HUNT 2 study. Plos One 2011;6(10):e26621. doi:10.1371/journal.pone.0026621.
Coutinho T, Goel K, de Sa DC, Kragelund C, Kanaya AM, Zeller M, Park J-S, Kober L, Torp-Pedersen C, Cottin Y, Lorgis L, Lee S-H, Kim Y-J, Thomas R, Roger VL, Somers VK, Lopez-Jimenez F. Central obesity and survival in subjects with coronary artery disease a systematic review of the literature and collaborative analysis with individual subject data. J Am Coll Cardiol. 2011;57:1877–86.
Allison DB, Faith MS, Heo M, Kotler DP. Hypothesis concerning the U-shaped relation between body mass index and mortality. Am J Epidemiol. 1997;146:339–49.
Ramsay SE, Whincup PH, Shaper AG, Wannamethee SG. The relations of body composition and adiposity measures to ill health and physical disability in elderly men. Am J Epidemiol. 2006;164:459–69.
Sa KN, Pereira CdM, Souza RC, Baptista AF, Lessa I. Knee pain prevalence and associated factors in a Brazilian population study. Pain Med. 2011;12:394–402.
Shiri R, Solovieva S, Husgafvel-Pursiainen K, Taimela S, Saarikoski LA, Huupponen R, Viikari J, Raitakari OT, Viikari-Juntura E. The association between obesity and the prevalence of low back pain in young adults. Am J Epidemiol. 2008;167:1110–9.
Muramoto A, Imagama S, Ito Z, Hirano K, Ishiguro N, Hasegawa Y. Physical performance tests are useful for evaluating and monitoring the severity of locomotive syndrome. J Orthop Sci. 2012;17(6):782–8.
Sasaki E, Ishibashi Y, Tsuda E, Ono A, Yamamoto Y, Inoue R, Takahashi I, Umeda T, Nakaji S. Evaluation of locomotive disability using loco-check: a cross-sectional study in the Japanese general population. J Orthop Sci. 2013;18:121–9.
Hayashi T, Boyko EJ, Leonetti DL, McNeely MJ, Newell-Morris L, Kahn SE, Fujimoto WY. Visceral adiposity is an independent predictor of incident hypertension in Japanese Americans. Ann Intern Med. 2004;140:992–1000.
Kramer CK, von Muehlen D, Gross JL, Barrett-Connor E. A prospective study of abdominal obesity and coronary artery calcium progression in older adults. J Clin Endocrinol Metab. 2009;94:5039–44.
Ochi M, Tabara Y, Kido T, Uetani E, Ochi N, Igase M, Miki T, Kohara K. Quadriceps sarcopenia and visceral obesity are risk factors for postural instability in the middle-aged to elderly population. Geriatr Gerontol Int. 2010;10:233–43.
Stewart KJ, DeRegis JR, Turner KL, Bacher AC, Sung J, Hees PS. Usefulness of anthropometrics and dual-energy X-ray absorptiometry for estimating abdominal obesity measured by magnetic resonance imaging in older men and women. J Cardiopulm Rehabil. 2003;23:109–14.
Pouliot MC, Despres JP, LEmieux S, Moorjani S, Bouchard C, Tremblay A. Waist circumference and abdominal sagittal diameter: best simple anthropometric indexes of abnominal visceral adipose tissue accumulation and related cardiovascular risk in men and women. Am J Cardiol. 1994;73:460–8.
Lean MEJ, Han TS, Seidell JC. Impairment of health and quality of life using new US federal guidelines for the identification of obesity. Arch Intern Med. 1999;159:837–43.
Peeters A, Bonneux L, Nusselder WJ, De Laet C, Barendregt JJ. Adult obesity and the burden of disability throughout life. Obes Res. 2004;12:1145–51.
Angleman SB, Harris TB, Melzer D. The role of waist circumference in predicting disability in periretirement age adults. Int J Obes. 2006;30:364–73.
Eckhardt CL, Adair LS, Caballero B, Avila J, Kon IY, Wang JZ, Popkin BM. Estimating body fat from anthropometry and isotopic dilution: a four-country comparison. Obes Res. 2003;11:1553–62.
Sridhar MS, Jarrett CD, Xerogeanes JW, Labib SA. Obesity and symptomatic osteoarthritis of the knee. J Bone Joint Surg Br. 2012;94B:433–40.
Sakakibara H, Zhu SK, Furuta M, Kondo T, Miyao M, Yamada S, Hideaki T. Knee pain and its associations with age, sex, obesity, occupation and living conditions in rural inhabitants of Japan. Environ Health Prev Med. 1996;1:114–8.
Janke EA, Collins A, Kozak AT. Overview of the relationship between pain and obesity: what do we know? Where do we go next? J Rehabil Res Dev. 2007;44:245–61.
Toda Y, Segal N, Toda T, Morimoto T, Ogawa R. Lean body mass and body fat distribution in participants with chronic low back pain. Arch Intern Med. 2000;160:3265–3269.
Hergenroeder AL, Brach JS, Otto AD, Sparto PJ, Jakicic JM. The influence of body mass index on self-report and performance-based measures of physical function in adult women. Cardiopulm Phys Ther J. 2011;22:11–20.
Vincent HK, Vincent KR, Lamb KM. Obesity and mobility disability in the older adult. Obes Rev. 2010;11:568–79.
Blaszczyk JW, Cieslinska-Swider J, Plewa M, Zahorska-Markiewicz B, Markiewicz A. Effects of excessive body weight on postural control. J Biomech. 2009;42:1295–300.
Woo J, Leung J, Kwok T. BMI, body composition, and physical functioning in older adults. Obesity. 2007;15:1886–94.
Fontaine KR, Barofsky I, Andersen RE, Bartlett SJ, Wiersema L, Cheskin LJ, Franckowiak SC. Impact of weight loss on health-related quality of life. Qual Life Res. 1999;8:275–7.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Muramoto, A., Imagama, S., Ito, Z. et al. Waist circumference is associated with locomotive syndrome in elderly females. J Orthop Sci 19, 612–619 (2014). https://doi.org/10.1007/s00776-014-0559-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00776-014-0559-6