Abstract
Background
Surgical site infection (SSI) is an important complication after spine surgery. The management of SSI is characterized by significant variability, and there is little guidance regarding an evidence-based approach. The objective of this study was to identify risk factors associated with treatment failure of SSI after spine surgery.
Patients and methods
A total of 225 consecutive patients with SSI after spine surgery between July 2005 and July 2010 were studied retrospectively. Patients were treated with aggressive surgical debridement and prolonged antibiotic therapy. Outcome and risk factors were analyzed in 197 patients having 1 year of follow-up. Treatment success was defined as resolution within 90 days.
Results
A total of 126 (76 %) cases were treated with retention of implants. Forty-three (22 %) cases had treatment failure with five (2.5 %) cases resulting in death. Lower rates of treatment success were observed with late infection (38 %), fusion with fixation to the ilium (67 %), Propionibacterium acnes (43 %), poly microbial infection (68 %), >6 operated spinal levels (67 %), and instrumented cases (73 %). Higher rates of early resolution were observed with superficial infection (93 %), methicillin-sensitive Staphylococcus aureus (95 %), and <3 operated spinal levels (88 %). Multivariate logistic regression revealed late infection was the most significant independent risk factor associated with treatment failure. Superficial infection and methicillin-sensitive Staphylococcus aureus were predictors of early resolution.
Conclusion
Postoperative spine infections were treated with aggressive surgical debridement and antibiotic therapy. High rates of treatment failure occurred in cases with late infection, long instrumented fusions, polymicrobial infections, and Propionibacterium acnes. Removal of implants and direct or staged re-implantation may be a useful strategy in cases with high risk of treatment failure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgical site infection (SSI) following spine surgery remains a serious complication that is not uncommon. SSI in spine surgery has adverse effects on morbidity, mortality, patient outcomes, length of hospital stay, and costs [1, 2]. The incidence of SSI following spine surgery has been reported to range from 1.9 to 10 % depending upon the study populations [3–9]. Recent studies describe age, obesity, smoking, previous infection, diabetes, revision surgery, serum glucose levels, use of instrumentation, and estimated intraoperative blood loss as risk factors for SSI [3, 8–11]. The goals when treating SSI are to eradicate infection, maintain a stable spine, and manage pain. Treatment options include intravenous antibiotic therapy, surgical debridement, and/or removal of implants. There is currently no consensus with regard to the best management paradigm, especially regarding the management of implants. Repeated surgical debridement combined with prolonged intravenous antibiotics is often necessary [12]. Implant removal can lead to deformity progression and potential neural injury, and many studies have reported successful treatment with surgical debridement while retaining implants [4, 5, 9, 13, 14]. However, implant retention has necessitated multiple surgeries [6, 15]. Multiple factors such as the type of index surgery, timing of infection, and type of treatment and organisms may have an impact on outcomes. Propionibacterium acnes (P. acnes) and coagulase negative Staphylococcus (CNS) are organisms that have been commonly identified in pediatric scoliosis patients receiving instrumented fusion [15]. Although several case studies have focused on outcomes, predictive factors for treatment success have not been well studied [15]. In this retrospective cohort study, risk factors associated with treatment success and failure are identified.
Methods
Patient population and characteristics
Surgical site infection was comprehensively diagnosed with clinical examinations, laboratory tests, radiographic results, and intraoperative or aspirated wound cultures among 7178 patients who underwent spine surgery at our institution between July 2005 and July 2010. Diagnosis of postoperative spine infection was based on the presence of at least one of the following findings: purulent drainage, back pain, fever, localized signs of inflammation such as swelling, redness or heat, and confirmation of the causative organism. Patients with infections deemed to have arisen through a different pathway such as hematogeneous seeding that were not related to the operative procedure were excluded from the study population. Superficial SSI was defined as infection involving only skin or subcutaneous tissue around the incision. For patients without implant, infection that occurred within 30 days after the index surgery was regarded as SSI. Among the patients with implants, manifestations of clinical signs and symptoms of infection within 90 days of implant placement were deemed early-onset SSI. The diagnostic criteria for late infection included the aforementioned diagnostic signs and findings of infection occurring more than 90 days after surgery along with radiological findings indicating screw loosening. Final determination for diagnosis of SSI was made by a physician from the Department of Infection Control and the attending surgeon. Patients with a primary diagnosis of osteomyelitis and who had a previous history of SSI were excluded. Two hundred twenty-five (3.1 %) patients with a diagnosis of SSI were identified by the UCSF Department of Hospital Epidemiology and Infection Control. Predictors of treatment success and failure included age, gender, number of operated spinal levels, fusion with fixation to the sacrum or ilium, revision surgery, use of instrumentation, diabetes, late infection, superficial infection, combined approach, individual organism, a gram-negative organism, and polymicrobial infection. Outcome measurement and risk factor analysis excluded 28 patients with follow-ups of <1 year.
Treatment strategy of SSI and management of implants
Each treatment course was reviewed for the type of surgery, management of implants, additional procedures, and duration of antibiotic therapy. Patients were treated with aggressive surgical debridement and prolonged antibiotic therapy. The wounds were irrigated and debrided of necrotic bone, muscle, and soft tissue, using at least 9 l of pulse lavage including vancomycin, gentamicin, and lactated Ringer’s solution. After cleaning the wound, implants were retained and subfascial drains were placed before closing the wound. Vacuum-assisted wound closure (VAC) systems [16, 17], antibiotic cement beads [12,], and antibiotic-containing irrigation-suction systems [13] were used according to the surgeon’s choice. Antibiotic therapy was initiated after intraoperative cultures had been taken. Intravenous antibiotics were typically administered for 6 weeks in the presence of instrumentation. The duration of antibiotic therapy was determined based on patient comorbidity, type of pathogen, type of surgery, and extension beneath the fascia. Implant removal was considered in cases of screw loosening or persistent infection. Reimplantation occurred during the debridement surgery as either primary or staged depending on the surgeon’s preference. Extension of fusion or supplemental anterior surgery was performed to treat loss of correction or pseudarthrosis. Diagnosis of infection, treatment course, management of implants, number of surgical debridements, and additional treatments were compiled from the electronic medical records.
Definition of clinical outcome and risk factor analysis
Outcomes were categorized into four types: (1) early resolution, which was defined as eradication of infection in <90 days with no clinical sign of infection such as purulent drainage, back pain, fever, localized swelling, and normalized laboratory data for at least 1 year; (2) delayed resolution, which was defined as infections taking more than 90 days to eradicate with at least 1-year freedom from infection; (3) persistence, which was defined as a recurrent infection, removal implants to eradicate the infection, or reimplantation for pseudarthrosis within a year from final follow-up; (4) death, which was defined as a patient who died because of an association with sepsis.
Statistical analysis
Statistical analyses were performed using SPSS v19.0.1 (SPSS Inc., Chicago IL). A T test was used to assess the significance of differences for continuous measures, a chi-square for dichotomous variables, and Fisher’s exact tests for cells with fewer than five cases. Stepwise forward multivariate logistic regression was used to identify the independent predictive factors of treatment failure. Statistical significance was predetermined for P-values <0.05.
Results
The mean patient age at the time of infection was 53.1 ± 18.5 years (range 7–85), with 54 % of the cases being male (Table 1). The mean duration of follow-ups from initial treatment was 21.4 months (range 6 days to 73 months). The median time from index surgery to initial treatment was 20 days (mean 54, range 2–868). A total of 162 (72 %) infections occurred within 30 days, 38 (17 %) within 30–90 days, 19 (8 %) within 90 days to 1 year, and 6 (3 %) more than 1 year after the index surgery. The majority of the cases involved the thoracolumbar region (83 %) with 17 % involving only the cervical spine. More than half of the cases had index diagnoses of either adult deformity (28 %) or degenerative disease (32 %). Of the pediatric deformity cases, 13 were diagnosed with neuromuscular scoliosis, 6 with idiopathic scoliosis, and 2 with Scheuermann’s kyphosis. When describing procedural characteristics, 2 out of 53 decompression cases used a mini-plate; no instrumentation was used in 2 out of 143 fusions, instrumentation was used in 2 out of 16 tumor excisions, 3 cases were implant removal, and 10 were reimplantations after removal of the implant. SSI at the anterior site occurred in only six cases with four of these as part of a combined approach. Of the 222 cases where cultures were taken, 78 (35 %) were polymicrobial, 6 (3 %) were fungal, and 7 (3 %) were culture negative. The most common cultured organism was Staphylococcus aureus (44 %, 100 cases) with 16 % (36 cases) displaying methicillin resistance (MRSA). Staphylococcus epidermidis was the second most common organism (27 %, 61 cases), and 13 % (29 cases) were methicillin resistant (MRSE). Vancomycin-sensitive Enterococcus (VSE) was isolated in 16 % (35 cases) and Propionibacterium acnes (P. acnes) in 7 % (16 cases). Gram-negative organisms were isolated in 22 % (58 cases) of cases, including E. coli in 10 % (23 cases), Pseudomonas aeruginosa in 5 % (11 cases), and Enterobacter cloacae in 5 % (11 cases).
Treatment course
The procedures used to treat instrumented and non-instrumented cases of SSI are described in Table 2. Non-instrumented cases were more often successfully treated without surgery (20 vs. 6 %), whereas instrumented cases more often required multiple (two or more) debridement surgeries (28 vs. 10 %). Of the 47 multiple surgery cases, 27 required 2, 11 required 3, 1 required 4, 5 required 5, and 3 required 6 surgeries to resolve the infection. Although infection was not suspected at the time of surgery, organisms were isolated from intraoperative wound culture in six cases. The VAC system was applied at the initial surgical debridement in nine cases and after several surgical debridements in ten cases. The average number of surgeries for a case with VAC placement was 3.1 (range 1–6). After the initial placement of VAC, the average time until wound closure was 11 days (range 4–24 days). Antibiotic cement beads were used after several surgical debridements (2–5). The mean length of intravenous and oral antibiotic therapy was longer for instrumented cases. Implants were retained in 126 (76 %) cases. Of these, antibiotics successfully treated the infection in 10 cases, 103 were resolved with a single surgical debridement, and 47 required multiple debridements. Additional surgeries involved removal of implants (11 cases), removal and reimplantation (24 cases; 14 primary, 10 staged), and reimplantation with extension of fusion or anterior fusion (5 cases).
Clinical outcomes and risk factor analysis
More than 1 year of follow-up information after infection treatment was available for 197 patients (147 instrumented and 50 non-instrumented). Early resolution was achieved in 154 (78 %) cases. Of the 43 cases defined as a treatment failure, 23 were resolved after more than 90 days of treatment (delayed resolution), 15 had persistent infection, and 5 (2.5 %) died from SSI-related complications. Of the deceased patients, two had hepatitis, one renal failure, and one Chiari malformation. All patients in the deceased group had early infection that was treated with retention of implants and surgical debridement; 4 died within 90 days (6, 10, 15, and 34 days) after surgical debridement. Acute spinal infection was deemed the cause of death in four patients. One patient, diagnosed with neuromuscular scoliosis, received surgical debridement five times with retention of the implant and died after 460 days because of ventriculoperitoneal shunt sepsis as a result of persistent infection.
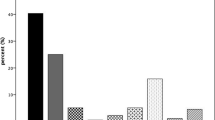
Risk factors and the percentage of patients successfully treated within 90 days are shown in Table 3. Low rates of treatment success were observed for infections involving P. acnes (43 %), late infection (38 %), fixation to the ilium (67 %), fusions involving more than six spinal levels (67 %), polymicrobial infection (68 %), and instrumented surgery (73 %). Higher rates of treatment success were observed with MSSA (95 %), superficial infection (93 %), the cervical region (92 %), and fusions involving fewer than three spinal levels (88 %). Multivariate regression analysis revealed late infection as the independent risk factor most strongly associated with treatment failure, while superficial infection and MSSA were associated with effective treatment (Table 4).
Discussion
In the present study, the majority of instrumented spinal SSIs (76 %) were treated with preservation of implants. Treatment strategy decisions are often based upon the presence of instrumentation. In a recent study of over 100000 cases in the Scoliosis Research Society M&M database, the authors found higher SSI rates with instrumentation (2.3 vs. 1.8 % with no instrumentation) [3]. Participants in the National Healthcare Safety Network reported SSI rates of 1.5 % for primary fusion and 1.0 % for laminectomy for nearly 100000 cases from 2006 to 2008 [18]. Single-institution studies have examined outcomes for non-instrumented surgery [4, 5,] but did not consider the influence of implants. It was found that instrumented cases required a longer duration of antibiotic therapy, required more debridement surgeries, and had a higher rate of treatment failure. SSI was successfully eradicated within 90 days in all non-instrumented cases. These results suggest that implants increase the challenge of treating SSI. In a series reported by Gunne, implants were retained with debridement in 55 of 75 cases (73 %), and 11 cases were treated with removal and reimplantation because of screw loosening [4]. They also found 73 % of superficial infection cases were successfully treated without surgical debridement. However, in the present series, only 20 % of superficial infection cases were treated without surgery. Since it may be difficult to determine the depth of an infection, surgical debridement is considered to be a potentially definitive treatment. Several studies have reported the efficacy of aggressive surgical debridement with retention of implants in early infection [1, 5, 12, 13, 19]. The 79 % success rate in the present series for treating early infection while retaining implants supports these results. In the case of deformity, implant removal may result in progressive deformity or neural injury before stable bony fusion has been completed. Kim reported a 70 % pseudarthrosis rate when implants were removed during surgical debridement in a series of short spinal fusion cases [20]. Thus, in the case of early infection, surgical debridement while preserving implants can be an effective treatment for SSI. Additionally, it is essential to include prolonged oral antibiotic suppression therapy in infected instrumented cases [19]. Nearly all instrumented cases were treated with prolonged oral antibiotic suppression therapy in the current series.
The definition of treatment failure was based on a poor response to debridement, not pain. Implant removal was necessary in 18 cases (12 delayed and 6 persistent). Revision due to pseudarthrosis was also considered as a treatment failure. Reported rates of pseudarthrosis following spinal SSI ranged from 5 to 20 % [5, 12, 21, 22]. In addition, Sponseller et al. [7] reported high rates of pain in infected patients (50 vs. 18 % in the non-infected group) with cerebral palsy. Collins et al. [6] reported 46 % of patients achieved resolution with no pain, stabilization of the spine, and eradication of infections. It is difficult to assess whether the etiology for chronic back pain is related to implants or due to other causes such as immunological, inflammation, adjacent segmental disease, proximal junctional kyphosis, or pseudarthrosis. Therefore, a chronic pain treatment failure criterion was not included. The definition of deep SSI as proposed by the Centers for Disease Control (CDC) is an infection occurring within 1 year if an implant is in place. In the setting of instrumented spine infections, however, Rihn et al. reported that the average time point of late-onset infection was 34.3 months (range 18–87 months) after the index surgery, and Richards et al. [14, 22] reported a corresponding time period of 25 months (range 11–45 months). Based on the review of clinical experiences, Richards et al. [22] stated that the cause of late infection in their series could have been intraoperative seeding at the index surgery that remained subclinical for an extended period of time. Therefore, patients with infection occurring more than 1 year after surgery were also included in the population of this study when it was considered to have arisen from the surgical site. The most common organisms associated with late infections are P. acnes and Staphylococcus epidermidis [6, 15, 22–24]. Skin flora at the time of the initial surgery was implicated as the primary route of contamination. Sampedro indicated that P. acnes was detected in 45 % and CNS in 40 % of peri-implant tissues and sonicated implants [25]. These organisms respond poorly to treatment because of their adherence to biofilm formation on implant surfaces [22, 26]. P. acnes was cultured in 7 of 12 late infection cases, MRSE in 6, and MSSE in 4. These organisms also comprised the majority of polymicrobial infections (P. acnes in 56 %, MSSE in 72 %, and MRSE in 83 %). There is no consensus regarding the management of implants in late infection. Of the late infection patients treated with implant retention and surgical debridement, 7 out of 12 (58 %) required subsequent removal of implants to eradicate the infection. There is no consensus regarding the management of implants in late infection. Implant removal often leaves the potential for curve progression and persistent back pain in cases of deformity surgery, whereas preserving implants can lead to persistent infection [15, 19, 21, 27]. In a similar series, Kowalski et al. [19] reported that implants were retained with surgical debridement in 28 out of 30 patients when the infection occurred within 30 days of the index surgery, and implants were removed in 32 out of 51 (63 %) patients with late infections. In a series reported by Ho et al. [15], 20 out of 43 (47 %) patients with idiopathic scoliosis required a second surgical debridement when implants were retained. Muschik et al. [21] found that a substantial proportion of pediatric scoliosis patients experienced loss of correction when implants were removed and not reinstrumented. These findings suggest that the treatment for late-onset infection, which include radical debridement and implant removal, should also include a plan in which the implants are reinserted at some point. Due to the fact that there are no data supporting when implants should be reinserted, it is unclear whether they should be reinserted at the same time as implant removal. At this point, intraoperative clinical judgment is paramount. For instance, if the surgeon enters the wound and finds liquid pus throughout the wound and covering the instrumentation, it may be best to wait a week after implant removal, give antibiotics, and then insert implants a week later after the frank pus is gone. However, if the surgeon finds that the wound has mainly fibrinous material that is easily debrided back to highly vascular and healthy tissue, then reinserting new implants at the same time could be considered.
Unfortunately, 5 of the 7178 patients receiving spine surgery at our institution during the period of this study (0.07 %) died because of sepsis following treatment for SSI. Schoenfeld et al. [28] reported a mortality rate of 0.3 % with increasing patient age and infection as independent predictors of mortality. The mortality rate for adult deformity cases reported to the Scoliosis Research Society morbidity and mortality database is 0.3 % [29]. Of the 17 deaths in the SRS database, 6 of these patients had had sepsis, but an association between sepsis and spine infection was not ascribed. The mortality rate among patients experiencing perioperative spinal infection in the National Inpatient Sample database is 1.4 %, but in this database, it is difficult to differentiate elective from emergent cases [2]. Patients with infection were 5.83 times more likely to expire than those without infection. In the present study, the mortality rate after spinal SSI was 2.5 %, which is significantly higher than in the general spine surgery population. The comorbidity burden should be evaluated before initial treatment for SSI, and implants should be promptly removed to reduce the risk of death. Furthermore, a less invasive index surgery should be considered in patients with multiple comorbidities.
One limitation to this study pertains to the retrospective nature of the case series and the heterogeneity of the treatment decisions made by the attending surgeons: removal of implants, the timing of surgery, use of a VAC system, use of antibiotic cement beads, and variation of the duration of antibiotic therapy. Supplemental procedures were initiated at the time of infection or after several irrigations, and these could potentially influence the treatment outcomes. A prospective study would provide stronger evidence for effective treatments. A second limitation relates to the imprecision when determining the etiology of infection. The definition established for treatment failure may have underestimated treatment success by including revision surgery for pseudarthrosis. Third, complete clinical information including the laboratory data and operating time was not available for some patients included in the study. Finally, treatment success was defined as at least a year free from infection; however, an optimal infection-free duration for defining treatment success is lacking. In the present series, 3 % (6 of 225 cases) of infections occurred more than 1 year after the index surgery.
In conclusion, postoperative spine infections were most commonly treated with aggressive surgical debridement and antibiotic therapy. Superficial infection, short fusion cervical spine surgery, and MSSA were predictors of early resolution and were often treated while retaining implants. High rates of treatment failure occurred in cases of late infection, long instrumented fusions, polymicrobial infections, and P. acnes infections.
References
Mok JM, Guillaume TJ, Talu U, Berven SH, Deviren V, Kroeber M, Bradford DS, Hu SS. Clinical outcome of deep wound infection after instrumented posterior spinal fusion: a matched cohort analysis. Spine. 2009;34:578–83.
Goode AP, Cook C, Gill JB, Tackett S, Brown C, Richardson W. The risk of risk-adjustment measures for perioperative spine infection after spinal surgery. Spine. 2011;36:752–8.
Smith JS, Shaffrey CI, Sansur CA, Berven SH, Fu KM, Broadstone PA, Choma TJ, Goytan MJ, Noordeen HH, Knapp DR Jr, Hart RA, Donaldson WF 3rd, Polly DW Jr, Perra JH, Boachie-Adjei O, Scoliosis Research Society Morbidity and Mortality Committee. Rates of infection after spine surgery based on 108,419 procedures: a report from the Scoliosis Research Society Morbidity and Mortality Committee. Spine. 2011;36:556–63.
Pull ter Gunne AF, Mohamed AS, Skolasky RL, van Laarhoven CJ, Cohen DB. The presentation, incidence, etiology, and treatment of surgical site infections after spinal surgery. Spine. 2010;35:1323–8.
Weinstein MA, McCabe JP, Cammisa FP Jr. Postoperative spinal wound infection: a review of 2,391 consecutive index procedures. J Spinal Disord. 2000;13:422–6.
Collins I, Wilson-MacDonald J, Chami G, Burgoyne W, Vineyakam P, Berendt T, Fairbank J. The diagnosis and management of infection following instrumented spinal fusion. Eu Spine J. 2008;17:445–50.
Sponseller PD, Shah SA, Abel MF, Newton PO, Letko L, Marks M. Infection rate after spine surgery in cerebral palsy is high and impairs results: multicenter analysis of risk factors and treatment. Clin Orthop Relat Res. 2010;468:711–6.
Koutsoumbelis S, Hughes AP, Girardi FP, Cammisa FP Jr, Finerty EA, Nguyen JT, Gausden E, Sama AA. Risk factors for postoperative infection following posterior lumbar instrumented arthrodesis. J Bone Joint Surg Am. 2011;93:1627–33.
Fang A, Hu SS, Endres N, Bradford DS. Risk factors for infection after spinal surgery. Spine. 2005;30:1460–5.
Olsen MA, Nepple JJ, Riew KD, Lenke LG, Bridwell KH, Mayfield J, Fraser VJ. Risk factors for surgical site infection following orthopaedic spinal operations. J Bone Joint Surg Am. 2008;90:62–9.
Pull ter Gunne AF, Cohen DB. Incidence, prevalence, and analysis of risk factors for surgical site infection following adult spinal surgery. Spine. 2009;34:1422–8.
Glassman SD, Dimar JR, Puno RM, Johnson JR. Salvage of instrumental lumbar fusions complicated by surgical wound infection. Spine. 1996;21:2163–9.
Levi AD, Dickman CA, Sonntag VK. Management of postoperative infections after spinal instrumentation. J Neurosurg. 1997;86:975–80.
Rihn JA, Lee JY, Ward WT. Infection after the surgical treatment of adolescent idiopathic scoliosis: evaluation of the diagnosis, treatment, and impact on clinical outcomes. Spine. 2008;33:289–94.
Ho C, Skaggs DL, Weiss JM, Tolo VT. Management of infection after instrumented posterior spine fusion in pediatric scoliosis. Spine. 2007;32:2739–44.
Mehbod AA, Ogilvie JW, Pinto MR, Schwender JD, Transfeldt EE, Wood KB, Le Huec JC, Dressel T. Postoperative deep wound infections in adults after spinal fusion: management with vacuum-assisted wound closure. J Spinal Disord Tech. 2005;18:14–7.
Canavese F, Gupta S, Krajbich JI, Emara KM. Vacuum-assisted closure for deep infection after spinal instrumentation for scoliosis. J Bone Joint Surg Br. 2008;90:377–81.
Edwards JR, Peterson KD, Mu Y, Banerjee S, Allen-Bridson K, Morrell G, Dudeck MA, Pollock DA, Horan TC. National Healthcare Safety Network (NHSN) report: data summary for 2006 through 2008, issued December 2009. Am J Infect Control. 2009;37:783–805.
Kowalski TJ, Berbari EF, Huddleston PM, Steckelberg JM, Mandrekar JN, Osmon DR. The management and outcome of spinal implant infections: contemporary retrospective cohort study. Clin Infect Dis. 2007;44:913–20.
Kim JI, Suh KT, Kim SJ, Lee JS. Implant removal for the management of infection after instrumented spinal fusion. J Spinal Disord Tech. 2010;23:258–65.
Muschik M, Luck W, Schlenzka D. Implant removal for late-developing infection after instrumented posterior spinal fusion for scoliosis: reinstrumentation reduces loss of correction. A retrospective analysis of 45 cases. Eu Spine J. 2004;13:645–51.
Richards BS. Delayed infections following posterior spinal instrumentation for the treatment of idiopathic scoliosis. J Bone Joint Surg Am. 1995;77:524–9.
Haidar R, Najjar M, Der Boghossian A, Tabbarah Z. Propionibacterium acnes causing delayed postoperative spine infection: review. Scand J Infect Dis. 2010;42:405–11.
Hahn F, Zbinden R, Min K. Late implant infections caused by Propionibacterium acnes in scoliosis surgery. Eu Spine J. 2005;14:783–8.
Sampedro MF, Huddleston PM, Piper KE, Karau MJ, Dekutoski MB, Yaszemski MJ, Currier BL, Mandrekar JN, Osmon DR, McDowell A, Patrick S, Steckelberg JM, Patel R. A biofilm approach to detect bacteria on removed spinal implants. Spine. 2010;35:1218–24.
Gristina AG, Costerton JW. Bacterial adherence to biomaterials and tissue. The significance of its role in clinical sepsis. J Bone Joint Surg Am. 1985;67:264–73.
Hedequist D, Haugen A, Hresko T, Emans J. Failure of attempted implant retention in spinal deformity delayed surgical site infections. Spine. 2009;34:60–4.
Schoenfeld AJ, Ochoa LM, Bader JO, Belmont PJ Jr. Risk factors for immediate postoperative complications and mortality following spine surgery: a study of 3475 patients from the National Surgical Quality Improvement Program. J Bone Joint Surg Am. 2011;93:1577–82.
Sansur CA, Smith JS, Coe JD, Glassman SD, Berven SH, Polly DW Jr, Perra JH, Boachie-Adjei O, Shaffrey CI. Scoliosis research society morbidity and mortality of adult scoliosis surgery. Spine. 2011;36:E593–7.
Acknowledgments
We are grateful to Dr. Steven Takemoto, Dr. Amir Abdul-jabbar, Dr. Serena S. Hu, Dr. Shane Burch, Praveen V. Mummaneni, MD, and Dr. Dean Chou for preparation of the manuscript.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was approved by the UCSF Committee on Human Research.
About this article
Cite this article
Maruo, K., Berven, S.H. Outcome and treatment of postoperative spine surgical site infections: predictors of treatment success and failure. J Orthop Sci 19, 398–404 (2014). https://doi.org/10.1007/s00776-014-0545-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00776-014-0545-z