Abstract
Introduction
Anaemia is present in more than 30 % of patients with various cancers at the time of initial presentation. Anaemia or a lower level of haemoglobin (Hb) is an indicator of poorer prognosis in many cancers. Several studies have also demonstrated that high levels of proinflammatory cytokines contribute to the development of anaemia. However, no studies have assessed the correlation between anaemia and survival in patients with soft tissue sarcoma. The aim of this study was to elucidate the relationship between anaemia and clinical outcome and to determine whether pretreatment anaemia predicted disease-specific survival in patients with adult soft tissue sarcoma.
Methods
A total of 376 patients between 2003 and 2010 were retrospectively reviewed. Patients who presented with metastases or/and local recurrence at diagnosis were excluded from this study.
Results
Hb levels varied from 8.0 to 17.3 g/dl in all patients. Pretreatment anaemia was seen in 114 patients. Hb levels were significantly correlated to C-reactive protein levels (Spearman ρ = −0.54, p < 0.0001). The tumour histological grade, age and tumour size were also significantly correlated to Hb levels. Patients with anaemia had a worse disease-specific survival (52.6 % at 5 years) than those without anaemia (79.7 % at 5 years) (p < 0.0001). Patients with anaemia also had a worse event-free rate (44 % at 5 years) than those without anaemia (66.3 % at 5 years) (p < 0.0001). Multivariate analysis showed that anaemia remained an independent predictor of survival (p = 0.002) and events (p = 0.0003).
Conclusion
Pretreatment anaemia may be indicative of an aggressive characteristic in patients with soft tissue sarcoma. We recommend the routine measurement of Hb level to identify patients who are at greater risk of death or an event.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Several relevant prognostic factors have been defined for soft tissue sarcomas. Tumour size, depth, histological tumour grade and age are predictive factors of survival [1–3]. Anaemia is present in more than 30 % of patients with various cancers at the time of initial presentation [4]. Anaemia or a lower level of haemoglobin (Hb) is an indicator of poorer prognosis in many cancers, such as lung cancer [5], renal cell cancer [6], and multiple myeloma [7]. Several studies have demonstrated that high levels of proinflammatory cytokines contribute to the development of anaemia [8–10]. Especially, interleukin-6 (IL-6) could be a mediator of cancer-related anaemia [8–10], and it induces the production of C-reactive protein (CRP) in hepatocytes [11].
However, no studies have assessed the correlation between inflammation and anaemia and the relationship between anaemia and survival in patients with soft tissue sarcoma. The aim of this study was to elucidate the relationship between anaemia and clinical characteristics and to determine whether pretreatment anaemia predicted the disease-specific survival and event-free rate in patients with adult soft tissue sarcoma.
Patients and methods
Patients
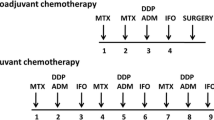
A total of 637 adult patients with primary soft tissue sarcoma were treated with surgical resection for primary tumour between January 2003 and December 2010 at a single institution (in the United Kingdom). Patients who presented with recurrent disease or distant metastasis at diagnosis or who were referred for additional resection were excluded from this study. Of the 637 patients treated with surgical resection, 258 patients had an incomplete clinical history or incomplete laboratory data. Three patients were excluded from this study because of obvious anaemia due to severe renal failure. The remaining 376 patients were retrospectively analyzed. Among the 376 patients in the cohort, the mean follow-up time was 32 months (range 1–101). Pretreatment staging included MR imaging of the primary tumour and CT scan of the lungs. Bone scintigraphy was performed for individual patients who were suspected of developing bone metastases. The histopathological diagnosis and tumour grade were determined using the French Federation of Cancer Centers Sarcoma Group (FNCLCC) grading system for all patients by experienced musculoskeletal pathologists. Treatment decisions were made by a multi-disciplinary team according to European Society of Medical Oncology (ESMO) clinical recommendations [12] and UK guidelines [13]. In general, most patients underwent surgical resection aimed at achieving clear margins followed by radiotherapy for large and/or deep high-grade tumours. Chemotherapy was considered for individual patients with a potentially chemosensitive subtype (such as synovial sarcoma, primitive neuroectodermal tumour) on the basis that it could not be excluded. The Hb levels were measured using an autoanalyzer as part of a routine clinical examination and were obtained before treatment for all patients. According to World Health Organization (WHO) cut-off levels, anaemia was defined as Hb levels below 13 g/dl in males and below 12 g/dl in females. A clinicopathological analysis was performed that compared the Hb levels to various factors, including age, gender, tumour size, tumour histological grade, American Joint Committee on Cancer (AJCC) stage, and the pretreatment levels of CRP.
The primary purpose of this study was to elucidate the prognostic factors, including anaemia, associated with patient survival using univariate and multivariate analyses. The following factors were studied: patient’s age (>60 vs. ≤60), gender, tumour depth (superficial vs. deep), tumour size (>10 cm vs. ≤10 cm), surgical margin (negative vs. positive), tumour grade (G1, G2 vs. G3), and presence of anaemia. The second purpose of this study was to determine the prognostic factors associated with the patient’s event-free rate using univariate and multivariate analyses.
Statistical analysis
The duration of disease-specific survival or event-free survival was defined as the interval between the date of initial treatment for the primary tumour and that of death, local recurrence or metastasis, respectively. Correlations between Hb and clinical characteristics were tested using Spearman rank correlation analysis [14]. A statistically significant Spearman ρ implies a correlation in the population. Survival curves were constructed using the Kaplan–Meier method. The log-rank test was used to compare disease-specific survival among patients. A multivariate analysis was performed using a Cox proportional hazards model. The variables included in the multivariate analysis were the significant factors identified in the univariate analysis. A value of p < 0.05 was considered to be significant in all statistical analyses.
Results
Patient, tumour, and treatment characteristics
A total of 376 patients were studied, including 221 males and 155 females, and their details are shown in Table 1. The patients were histologically classified as follows: 123 malignant fibrous histiocytomas (MFH), 94 liposarcomas, 47 myxofibrosarcomas, 34 leiomyosarcomas, 22 synovial sarcomas, 10 fibrosarcomas, 9 malignant peripheral nerve sheath tumours (MPNST), and 37 other tumours. The primary tumour sites were the thighs (n = 169), legs (n = 34), forearms (n = 22), buttock (n = 20), upper arms (n = 19), pelvis (n = 17), knees (n = 15), chest walls (n = 13), shoulders (n = 10) and other sites (n = 57).
Relationships between anaemia and clinical characteristics
Hb levels varied from 8.0 to 17.3 g/dl (mean 13.2 g/dl, median 13.4 g/dl). Pretreatment anaemia was seen in 114 patients. Fifty-one of the 123 patients with MFH had anaemia and 21 of the 93 patients with liposarcoma had anaemia (Table 2).
The correlation between the clinical characteristics and preoperative Hb levels is shown in Table 3. Tumour histological grade, age, tumour size and CRP levels were all significantly correlated to Hb levels (Fig. 1). We excluded CRP levels from prognostic analysis because they showed a moderate correlation (Spearman ρ = −0.54, p < 0.0001) with anaemia using Spearman rank correlation that could affect the analysis.
Disease-specific survival and predictors of mortality
One hundred and eighty-eight of the 376 patients (50 %) were alive with continuous disease-free (CDF) status as of December 2011, 242 had no evidence of disease (NED), 31 were alive with disease (AWD), 78 had died of disease (DOD), and 25 had died of other causes (DOOC). The 5-year disease-specific survival rate was 71.8 %.
Patients with anaemia before initial treatment had a worse disease-specific survival than patients without anaemia (p < 0.0001). The disease-specific survival at 5 years was 52.6 vs. 79.7 %, respectively (Fig. 2). Univariate analysis also revealed significantly worse survival for older patients (p = 0.04), larger tumour size (p = 0.01), higher histological grade tumour (p < 0.0001) and surgical positive margin (p = 0.01) (Table 4). Anaemia remained a significantly prognostic factor in multivariate analysis (p = 0.002) (Table 5). On receiver operating characteristic (ROC) analysis, a value of 12.5 g/dl was found to be an appropriate threshold to identify if patients were at risk from death at 2 years (Fig. 3). We also examined the relationship between anaemia, survival, and event separately for patients with MFH and liposarcoma. Patients with an MFH and anaemia before their initial treatment had a significantly poorer disease-specific survival than those without anaemia (p = 0.006). The rates of survival for patients with a liposarcoma did not significantly differ between those with and without anaemia (p = 0.07) (Table 6).
Event-free survival and predictors of events
The five-years event-free survival was 59.4 % in all patients. Patients with anaemia before initial treatment had a worse event-free rate after initial treatment than patients without anaemia (p < 0.0001). The event-free survivals at 5 years were 44 vs. 66.3 %, respectively (Fig. 4). A univariate analysis also revealed significantly poorer outcomes for older patients (p = 0.04), for those with a positive surgical margin (p = 0.02), and higher histological tumour (p < 0.0001) (Table 7). A multivariate analysis showed that the pretreatment anaemia remained an independent predictor of events (p = 0.0003) (Table 8). Anaemia was a significant adverse prognostic factor for MFH and liposarcoma (p = 0.01, p = 0.048, respectively) (Table 6).
Discussion
Pretreatment anaemia is detected in approximately 30 % of patients with cancers [4]. Bacci reported that 13 % of 359 patients with Ewing sarcomas had anaemia by the time of diagnosis [15]. The current study showed that 30 % of the patients with soft tissue sarcomas had anaemia by the time of diagnosis. This was related to large, high-grade tumours such that 56 % of patients with AJCC stage III tumours had anaemia by the time of presentation. Specifically, only 21 % of 94 patients with liposarcoma had anaemia, although 41 % of 123 patients with MFH did (Table 2). Of the 94 patients with liposarcoma, 24 patients had grade 1 liposarcoma, and these results may have affected the small number of patients with pre-treatment anaemia.
Pretreatment anaemia is an indicator of worse prognosis in many cancers [4–7, 16]. The present univariate and multivariate analysis showed that pretreatment anaemia was associated with decreased disease-specific survival and event-free survival in 376 adult patients with soft tissue sarcoma. We also elucidated the relationship between anaemia and survival for patients with MFH separately from those with liposarcoma. Anaemia was an adverse prognostic factor for disease-specific survival in patients with MFH and other sarcomas, but not in those with liposarcoma. Although the results for liposarcoma were less conclusive, there was a trend towards significance which may be clarified through the analysis of a larger sample size. Our results suggest that pre-treatment anaemia is a measure of tumour aggressiveness: this was shown by its association with disease-specific survival for MFH and other sarcomas.
Several studies have previously demonstrated that high levels of the inflammatory cytokine IL-6 contribute to the development of anaemia [8–10]. It has been shown that IL-6 is a strong inducer of hepcidin in liver cells [8]. Hepcidin is considered to be an iron-regulatory hormone that is responsible for inflammation-induced iron disutilization, resulting in the anaemia associated with acute and chronic infections, chronic kidney disease, and malignant tumours [8]. Rutkowski [17] showed that increased serum levels of IL-6 were found in 61 % of soft tissue sarcoma patients. In the current study, Hb levels were significantly negatively correlated with CRP levels. Although we did not investigate the levels of IL-6, it is well known that IL-6 induces the production of CRP in hepatocytes [11].
There are a few limitations of the present study. First, the presence of other diseases may be associated with lower levels of Hb. Although we excluded patients with obvious anaemia due to severe renal failure, other chronic conditions were not taken into consideration due to a lack of information. The retrospective design of the study was another limitation. However, we believe that the measurement of Hb level is an extremely useful method of recognizing patients who are at greater risk of death or an event.
References
Stojadinovie A, Leung DHY, Hoos A, Jaques DP, Lewis JJ, Brennan MF. Analysis of the prognostic significance of microscopic margins in 2084 localized primary adult soft tissue sarcoma. Ann Surg. 2002;235:424–34.
Stefannovski PD, Bidoli E, De Paoli A, Buonadonna A, Boz G, Libra M, Morassut S, Rossi C, Carbone A, Frustaci S. Prognostic factors in soft tissue sarcomas: a study of 395 patients. EJSO. 2002;28:153–64.
Lewis JJ, Antonescu CR, Leung DH, Blumberg D, Healey JH, Woodruff JM, Brennan MF. Synovial sarcoma: a Multivariate analysis of prognostic factor in 112 patients with primary localized tumors of the extremity. J Clin Oncol. 2000;18:2087–94.
Ludwig H, Van Belle S, Barrett-Lee P, Birqeqard G, Bokemeyer C, Gascon P, Kosmidis P, Krzakowski M, Nortier J, Olmi P, Schneider M, Schrijvers D. The European Cancer Anaemia Survey (ECAS): a large multinational, prospective survey defining the prevalence, incidence, and treatment of anaemia in cancer patients. Eur J Cancer. 2004;40:2293–306.
Martin F, Santolaria F, Batista N, Milena A, Gonzalez-Reimers E, Brito MJ, Oramas J. Cytokine levels (IL-6 and IFN-gamma), acute phase response and nutritional status as prognostic factors in lung cancer. Cytokine. 1999;11:80–6.
Falkensammer CE, Thurnher M, Leonhartsberger N, Ramoner R. C-reactive protein is a strong predictor for anaemia in renal cell carcinoma: role of IL-6 in overall survival. BJU Int. 2011;107:1893–8.
Zakraoui L, Cheour I, Jeridi T, Jellouli N, Berqaoui N, Moalla M, Abdeladhim A, Karoui M. Ben Hamida A, Zouari R. Prognostic factors in multiple myeloma. Critical analysis based on a multicenter study of 53 cases. Tunis Med. 1988;66:663–72.
Nemeth E, Rivera S, Gabayan V, Keller C, Taudorf S, Pedersen BK, Ganz T. IL-6 mediates hypoferremia of inflammation by inducing the synthesis of the iron regulatory hormone hepcidin. J Clin Invest. 2004;113:1271–6.
Nieken J, Mulder NH, Buter J, Vellenga E, Limburg PC, Piers DA, de Vries EG. Recombinant human interleukin-6 induces a rapid and reversible anemia in cancer patients. Blood. 1995;86:900–5.
Mori K, Fujimoto-Ouchi K, Onuma E, Noguchi M, Shimonaka Y, Yasuno H, Nishimura T. Novel models of cancer-related anemia in mice inoculated with IL-6-producing tumor cells. Biomed Res. 2009;30:47–51.
Castell JV, Gomez-Lechon MJ, David M, Fabra R, Trullenque R, Heinrich PC. Acute-phase response of human hepatocytes; regulation of acute-phase protein synthesis by interleukin-6. Hepatology. 1990;12:1179–86.
Leyvraz S, Jelic S. ESMO Guidelines Task Force. ESMO Minimum Clinical Recommendation for diagnosis, treatment and follow-up of soft tissue sarcomas. Ann Oncol. 2005;16(Suppl 1):i69–70.
Grimer R, Judson I, Peake D, Seddon B. Guidelines for the management of soft tissue sarcomas. Sarcoma. 2010;2010:506182.
Dusick DM. Spearman rank correlation. http://bold-ed.com/corrsp.htm. Accessed 12 June 2013.
Caro JJ, Salas M, Ward A, Goss G. Anemia as an independent prognostic factor for survival in patients with cancer: a systematic, quantitative review. Cancer. 2001;91:2214–21.
Bacci G, Ferrari S, Bertoni F, Rimondini S, Longhi A, Bacchini P, Forni C, Manfrini M, Donati D, Picci P. Prognostic factors in nonmetastatic Ewing’s sarcoma of bone treated with adjuvant chemotherapy: analysis of 359 patients at the Istituto Orthpedico Rizzoli. J Clin Oncol. 2000;18:4–11.
Rutkowski P, Kaminska J, Kowalska M, Ruka W, Steffen J. Cytokine serum levels in soft tissue sarcoma patients: correlations with clinico-pathological features and prognosis. Int J Cancer. 2002;100:463–71.
Conflict of interest
Each author certifies that he has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article, and declares that they have no conflict of interest.
Ethical standard
Each author certifies that his institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with the ethical principles of research.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Nakamura, T., Grimer, R., Gaston, C. et al. The relationship between pretreatment anaemia and survival in patients with adult soft tissue sarcoma. J Orthop Sci 18, 987–993 (2013). https://doi.org/10.1007/s00776-013-0454-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00776-013-0454-6