Abstract
Background
Reported revision of internal fixation for undisplaced intracapsular hip fractures is between 12 and 17 % at 1 year. This risk is greater for elderly patients, for whom mortality after such a fracture is also higher. Our purpose was to identify predictors of fixation failure and mortality for elderly patients sustaining undisplaced intracapsular hip fractures, and to assess whether their socioeconomic status affected their outcome.
Methods
During a 3-year period we prospectively compiled a consecutive series of 162 elderly (≥65 years old) patients who underwent internal fixation for an undisplaced (Garden stage I or II) intracapsular hip fracture. Patient demographics, American Society of Anesthesiologists (ASA) grade, and posterior tilt (measured on the lateral radiograph) were recorded pre-operatively. All patients were followed up for a minimum of 1 year. Each patient’s socioeconomic status was assigned by use of the Scottish Index of Multiple Deprivation. Patient mortality was established by use of the General Register Office for Scotland.
Results
There were 28 failures of fixation during the study period. In Cox regression analysis, ASA grade and the presence of posterior tilt (p < 0.0001) were significant independent predictors of fixation failure. Overall unadjusted mortality at 1 year was 19 % (n = 30/162). Cox regression analysis also affirmed ASA grade to be the only significant independent predictor of 1-year mortality (p = 0.003). The standardised mortality rate for the cohort was 2.3 (p < 0.001), and was significantly greater for patients less than 80 years of age (p = 0.004). Socioeconomic status did not affect outcome, but the most deprived patients sustain their fracture at a significantly younger age (p = 0.001).
Conclusion
We have demonstrated that ASA grade and posterior tilt of the femoral neck are independent predictors of fixation failure of undisplaced intracapsular hip fractures in elderly patients, and ASA grade was also an independent predictor of mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hip fractures account for 12 % of all adult fractures presenting to orthopaedic trauma surgeons [1], and are a major cause of morbidity and mortality for elderly patients [2]. Although the reported annual incidence of hip fractures during the last decade has plateaued [3], the population at risk continues to increase [4]. Hence, elderly patients will continue to form an increasing proportion of the orthopaedic trauma workload in the future.
Approximately 50 % of hip fractures are intracapsular [5], of which 32 to 38 % are undisplaced [6, 7]. Conventional management of an undisplaced intracapsular hip fracture is by internal fixation; however, revision is reported to be between 12 and 17 % at 1 year [8, 9]. Recently, Gjertsen et al. [7] demonstrated that outcome for displaced intracapsular hip fractures managed with a hemiarthroplasty was better than for undisplaced intracapsular hip fractures managed with internal fixation. If patients with a high risk of revision surgery could be identified before fixation of their undisplaced intracapsular hip fracture, they may benefit from a primary hemiarthroplasty or, potentially, a total hip replacement [10]. Conn and Parker [8] identified age, mobility, and the lateral Garden angle as risk factors for non-union after fixation of undisplaced intracapsular hip fractures. Whether these or other factors, for example social deprivation, are independent predictors of failure of fixation is unknown.
One-year mortality after a hip fracture is approximately 30 % [11]. Independent patients surviving beyond this time may benefit from a total hip replacement rather than hemiarthroplasty [10, 12]. Isolated independent predictors of survival have been identified for hip fractures, but these are inclusive of intra and extra-capsular fractures [11, 13]. Holt et al. [2] specifically identified intra-capsular fractures as being associated with reduced early mortality relative to other hip fracture patterns. Predictors of patient survival after sustaining an undisplaced intracapsular hip fracture have not previously been described. If these predictors were available, patients with a high risk of fixation failure of their undisplaced hip fracture and who are likely to survive beyond 1 year may benefit from an arthroplasty.
Social deprivation affects the outcome of orthopaedic intervention [14, 15]. Quah et al. [15] demonstrated that social deprivation was associated with an increased incidence of hip fractures among elderly patients. Socially deprived patients were younger, had greater comorbidity, and suffered a higher unadjusted mortality relative to more affluent patients [15]. The effect of social deprivation on the outcome of specific hip-fracture patterns, for example intracapsular fractures, remains unknown.
The primary purpose of this study was to identify predictors of failure of internal fixation and 1 year mortality of elderly patients sustaining undisplaced intracapsular hip fractures. The secondary purpose was to describe epidemiology and outcome for elderly patients with undisplaced intracapsular hip fractures according to their socioeconomic status.
Patients and methods
Ethical approval was not required because the data reported in this study were obtained during normal clinical follow-up within the health care system of the reporting country.
During a 3-year period (2008–2010) we prospectively compiled a consecutive series of 162 elderly (≥65 years old) patients who underwent internal fixation for an undisplaced (Garden stage I or II [16]) intracapsular hip fracture. The study centre is the only hospital receiving adult trauma for a predominately urban population of 818,000 (East Lothian, Mid Lothian, West Lothian, and the City of Edinburgh), of which 14.7 % are aged 65 years old or more [17]. All patients from the catchment area who were treated in the study centre but who resided outside these areas were excluded from analysis. All patients receiving their initial management outside our catchment area but who resided within it were included. All data were prospectively collected and recorded (NDC, KG, NM).
The patients demographic details, socio-economic status, and American Society of Anesthesiologists (ASA) grade were recorded. The patients socio-economic status was assigned by use of the Scottish Index of Multiple Deprivation (SIMD) [18]. Each patient’s postcode was used to allocate their social quintile, with the first quintile being the most deprived and the fifth quintile being the least deprived. The radiographs were assessed by a single author (NDC) and were classified according to the Garden [16] and Pauwels [19] classification. Garden’s lateral angle [20] was also measured and if the angle less than 170° the patients were defined to have posterior tilt (Fig. 1). Screw positioning was considered adequate if:
-
it was parallel (<5° deviation);
-
at least two screws were within 5 mm of the subchondral bone;
-
it had both posterior and calcar contact for support; and
-
there was at least one screw in the posterior and one in the inferior aspect of the femoral head [9].
All patients were managed according to hip fracture protocols established by the Scottish Intercollegiate Guidelines Network [21]. The study centre has eleven orthopaedic trauma surgeons who were responsible for care of the patients. No intra-operative reduction manoeuvres were performed. Either a direct mini lateral approach or a percutaneous approach was used to insert 6.5 mm AO cannulated screws (Stratec Medical, Welwyn Garden City, Hertfordshire, UK) under fluoroscopy guidance. Three screws were used for all cases, with most screws being placed in an inverted triangle configuration, depending on surgeons’ preference. Patients were encouraged to bear weight as able from the first post-operative day.
Patients were followed-up for a minimum of 1 year to a maximum of 3.6 years, with a mean follow-up of 1.7 years. No patient was lost to follow-up. Failure of the fixation was defined as revision of the screws for any reason, or if there was any intention to revise. Forty-three patients (27 %) died during the study period, and the exact date was retrieved from the General Register Office for Scotland [22].
Statistical analysis
SPSS version 16.0 software was used for statistical analysis (SPSS, Chicago, IL, USA). Unpaired t-tests or analysis of variance (ANOVA) were used to compare linear variables, and Chi-squared tests or a Fisher’s exact tests (if <10) were used to compare dichotomous variables between groups. Age and gender standardized mortality rate (SMR) was calculated by use of life-expectancy data held by the Scottish Office for the population at risk [22]. Kaplan–Meier methodology was used to investigate survival. Cox regression analysis, using forward conditional methodology entering all case-mix variables, was used to identify significant independent predictors of failure of fixation and 1 year mortality. A p value of ≤0.05 determined statistical significance.
Results
The mean age of the patients was 81.8 years (range 65–98). The mean age of males patients was 80.8 (range 66–96) years; that of female patients was 82.1 (range 65–98) years (unpaired t test p = 0.37). Most patients were female and had a severe systemic disease according to their ASA grade (Table 1). A simple fall from standing height was the cause of the fracture for all except one, who fell from a bicycle. Our cohort was relatively affluent according to their socioeconomic status. Garden stage I was the commonest fracture pattern, with Pauwels grade III being a rare configuration (Table 1). Posterior tilt was observed for 27 patients (16.7 %), and more than 90 % of patients were classified as having had adequate screw fixation.
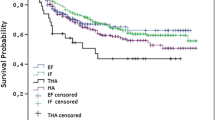
There were 28 failures of fixation during the study period. This resulted in 1-year implant survival of 87 % (95 % CI 81.5–92.5); this diminished to 81 % (95 % CI 75.9–86.1) and 78 % (95 % CI 71.9–84.1) at 2 and 3 years, respectively, however (Fig. 2). The only significant risk factors of fixation failure after univariate analysis were ASA grade and the presence of posterior tilt (Table 2; Figs. 3, 4). Subgroup analysis was also undertaken according to surgical grade (p = 0.13, χ 2) and surgeon (p = 0.56, χ 2) performing the surgery, neither of which was a significant predictor of failure. ASA grade and the presence of posterior tilt remained significant independent predictors of fixation failure, after adjusting for confounding variables (Table 3). On post-hoc analysis, we identified that those patients who had a shorter length of hospital stay were more likely to fail than those patients with a longer length of stay (unpaired t test p = 0.003).
Overall unadjusted mortality at 1 year was 19 % (n = 30/162). ASA grade was the only significant risk factor of 1-year mortality (Table 2), and remained the only significant independent predictor of mortality (odds ratio 2.0, 95 % CI 1.3–3.1, Cox regression p = 0.003) after adjusting for case-mix variables. The overall SMR for the cohort was 2.3 (95 % CI 1.59–3.25, Chi-squared p < 0.0001), but this varied according to gender and age (Table 4). There was no significant difference between genders (Chi-squared p = 0.23), but patients aged 65–79 year old had a significantly greater 1-year SMR (Chi-squared p = 0.004) than older patients.
Incidence, patient demographics, and fracture patterns were similar across all social quintiles, with no statistical difference (Table 5). The mean age, however, was significantly different among social quintiles (ANOVA p = 0.001), with the most deprived patients sustaining their hip fracture some 7 years earlier than the least deprived (Fig. 5). There were no significant differences in outcome according to social status, with similar fixation failure, unadjusted mortality, and SMR being observed (Table 5).
Discussion
We have demonstrated that ASA grade and posterior tilt of the femoral neck are independent predictors of fixation failure of undisplaced intracapsular hip fractures in elderly patients, and ASA grade was also an independent predictor of mortality. Although social deprivation did not affect outcome for undisplaced intracapsular hip fractures in the elderly, the age at which the most deprived sustained their fracture was significantly younger than more affluent patients.
A limiting factor of this study was that only patients who re-presented with pain or dissatisfaction and were subsequently revised were labelled as a failure. It is possible that patients with limited functional demand or who died did not re-present and may have become covert failures. Hence, the fixation survival results we present probably represent the best case scenario, which may be worse if all patients had endured radiographic assessment. The prospective nature, with a relatively large cohort and 100 % follow-up from a defined catchment population, are the main strengths of the study lending validity to our results. We also tried to assess the effect of bone mineral density on failure of the cannulated screws; only 46 patients in our cohort had a dual-energy X-ray absorptiometry scan performed before their hip fracture, however. Analysis of this smaller sub-group revealed a trend toward significance for increased failure in patients with lower bone mineral density (−1.2 versus −2.3, p = 0.09 un-paired t test).
The implant survival we reported of 78 % at 3 years is lower than that observed in previous studies. Survival of 83 % [9] to 100 % [23] have been reported, with the largest series in the literature reporting 88 % survival [8]. The reason for our lower reported survival may relate to the case-mix variables of the cohort. We only included patients aged 65 years or more, and hence the mean age of our cohort (82 years) is the oldest reported in the literature [8]. Increasing age has been associated with non-union of femoral neck fractures [8, 24, 25], and hence the lower survival we observed may be because of the older age of our cohort. Age was, however, not demonstrated to be a predictor of implant survival in our elderly cohort, with only ASA grade and posterior tilt being significant predictors. Interestingly a lower ASA grade was associated with greater occurrence of fixation failure; this may be the opposite to what is expected, because with increasing morbidity there is a greater rate of non-union for displaced intracapsular hip fractures [26]. It would seem from our cohort that increasing comorbidity for undisplaced intracapsular fractures in the elderly is not related to fixation failure. The reason for this discrepancy is not clear, but may be related to the functional demand of the patient, because patients with a lower ASA grade have an earlier return to full weight bearing and independent living [27]. This is supported by the fact that patients with a shorter length of hospital stay, being a marker of independence, were associated with an increased risk of failure of fixation for our cohort. This early mobilisation may increase the stress upon the fixation and result in its failure. Hence, it may be prudent to advise such patients to touch weight bear in the first 6 weeks, as would be advised for patients who have the same fixation for a displaced intracapsular hip fracture [26].
We have confirmed that posterior tilt (anterior angulation) on the lateral radiograph of the hip was an independent predictor of fixation failure, this was previously identified as a risk factor by Conn and Parker [8] for undisplaced intracapsular hip fractures. The presence of posterior tilt probably relates to comminution of the posterior aspect of the femoral neck. This is associate with an inferior biomechanical construction when using cannulated screws [28]. Patients with posterior tilt may benefit from the biomechanical advantage of either four screws or a fixed-angle device, for example a sliding hip screw, which could potentially improve their survival [29]. According to recent evidence from the Norwegian hip fracture register, however, patients with displaced intracapsular hip fractures experienced greater satisfaction, pain relief, and better functional results than patients who had sustained undisplaced intracapsular hip fractures managed with internal fixation [7]. Gjertsen et al. [7] hypothesize this difference in outcome may relate to the higher re-operation rate associated with internal fixation (10 %) compared with hemiarthroplasty (3 %). This would suggest patients with a high risk of failure of internal fixation, lower ASA grade, and posterior tilt on the lateral radiograph may be a specific subgroup that would benefit from a hemiarthroplasty.
The 1-year unadjusted mortality we observed, 19 %, is similar to that in previous reports [8], which is approximately 10 % less than for other types of hip fracture [11]. Patients’ age and gender have previously been shown to be independent predictors of mortality for hip fracture [2, 13]; this was not the case for our cohort. This may be related to the specific subgroup we analysed, including only elderly patients with undisplaced intracapsular fractures, which, as we have shown, have a different outcome relative to other hip fractures. The ASA grade was designed to predict peri-operative mortality, which has previously been shown to be an independent predictor of early mortality for hip fracture patients [2]. We have also confirmed the predictive effect of the ASA grade into the long-term. Patients with a lower ASA grade, predicting longevity, but with risk factors for failure of internal fixation may benefit from a primary total hip replacement if we apply the rationale discussed above [10].
We are unaware of any previously published study identifying younger age as being associated with a large SMR, as we have illustrated, after a hip fracture. Most studies analysing survival identify increasing age as a predictor of mortality [2, 11, 13]. These studies, however, did not use aged and gender-standardised methodology. Patients sustaining an undisplaced intracapsular hip fracture aged 65–79 years, with the greatest SMR, may benefit from early ortho-geriatric review and medical optimisation which may improve their survival [30].
Socially deprived patients in our cohort sustained their hip fracture at a younger age than more affluent patients, which has been established previously by Quah et al. [15]. However, we did not find any variance according to deprivation in the incidence, level of comorbidity, or mortality, which where demonstrated to differ by Quah et al. In contrast our cohort had a 7-year age difference between the most and least deprived, which was greater than that demonstrated by Quah et al. [15] (1 year). Although mortality, both unadjusted and SMR, was not significantly different, deprived patients sustained a morbid fracture some 7 years earlier than the least deprived. The reason for this disparity is not clear, but further work should be undertaken to investigate this social discrepancy, with the purpose of improving outcome for the most deprived in our society.
Management of elderly patients with an undisplaced fractured neck of femur with a high risk of fixation failure is difficult, and future randomised control trials are required to compare the outcome of alternative methods of internal fixation and/or arthroplasty for these patients.
References
Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37:691–7.
Holt G, Smith R, Duncan K, Finlayson DF, Gregori A. Early mortality after surgical fixation of hip fractures in the elderly: an analysis of data from the Scottish hip fracture audit. J Bone Joint Surg Br. 2008;90:1357–63.
Kannus P, Niemi S, Parkkari J, Palvanen M, Vuori I, Jarvinen M. Nationwide decline in incidence of hip fracture. J Bone Miner Res. 2006;21:1836–8.
Parliament UK. http://www.parliament.uk/documents/commons/lib/research/key_issues/Key%20Issues%20The%20ageing%20population2007.pdf. (2011). Accessed 10th Dec 2011.
Holt G, Smith R, Duncan K, Hutchison JD, Gregori A. Gender differences in epidemiology and outcome after hip fracture: evidence from the Scottish Hip Fracture Audit. J Bone Joint Surg Br. 2008;90:480–3.
Gjertsen JE, Engesaeter LB, Furnes O, Havelin LI, Steindal K, Vinje T, Fevang JM. The Norwegian hip fracture register: experiences after the first 2 years and 15,576 reported operations. Acta Orthop. 2008;79:583–93.
Gjertsen JE, Fevang JM, Matre K, Vinje T, Engesaeter LB. Clinical outcome after undisplaced femoral neck fractures. Acta Orthop. 2011;82:268–74.
Conn KS, Parker MJ. Undisplaced intracapsular hip fractures: results of internal fixation in 375 patients. Clin Orthop Relat Res. 2004;421:249–54.
Lagerby M, Asplund S, Ringqvist I. Cannulated screws for fixation of femoral neck fractures. No difference between Uppsala screws and Richards screws in a randomized prospective study of 268 cases. Acta Orthop Scand. 1998;69:387–91.
Keating JF, Grant A, Masson M, Scott NW, Forbes JF. Randomized comparison of reduction and fixation, bipolar hemiarthroplasty, and total hip arthroplasty. Treatment of displaced intracapsular hip fractures in healthy older patients. J Bone Joint Surg Am. 2006;88:249–60.
Wiles MD, Moran CG, Sahota O, Moppett IK. Nottingham Hip Fracture Score as a predictor of one year mortality in patients undergoing surgical repair of fractured neck of femur. Br J Anaesth. 2011;106:501–4.
Avery PP, Baker RP, Walton MJ, Rooker JC, Squires B, Gargan MF, Bannister GC. Total hip replacement and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck: a seven- to ten-year follow-up report of a prospective randomised controlled trial. J Bone Joint Surg Br. 2011;93:1045–8.
Stewart NA, Chantrey J, Blankley SJ, Boulton C, Moran CG. Predictors of 5 year survival following hip fracture. Injury. 2011;42:1253–6.
Clement ND, Muzammil A, MacDonald D, Howie CR, Biant LC. Socioeconomic status affects the early outcome of total hip replacement. J Bone Joint Surg Br. 2011;93B:464–9.
Quah C, Boulton C, Moran C. The influence of socioeconomic status on the incidence, outcome and mortality of fractures of the hip. J Bone Joint Surg Br. 2011;93:801–5.
Garden RS. Low-angle fixation in fractures of the femoral neck. J Bone Joint Surg Br. 1961;43:647–63.
General Register Office for Scotland. http://www.gro-scotland.gov.uk/statistics/theme/population/estimates/mid-year/archive/2008/list-of-tables.html (2011). Accessed 11th Dec 2011.
The Scottish Government Scottish Index of Multiple Deprivation 2009: General Report. Vol 2010 ed Edinburgh: The Scottish Government; 2009.
Pauwels F. Der Schenkelhalsbruch: Ein mechaniisched problem. Stuttgart: Ferdinand Enke; 1935.
Garden RS. Malreduction and avascular necrosis in sub capital fractures of the femur. J Bone Joint Surg Br. 1971;53:183–97.
Scottish Intercollegiate Guidelines Network. Management of hip fracture in older people SIGN 111. http://www.sign.ac.uk (2010). Accessed 11th Dec 2011).
General Register Office for Scotland. http://www.gro-scotland.gov.uk (2011). Accessed 11th Dec 2011.
Cserhati P, Kazar G, Manninger J, Fekete K, Frenyo S. Non-operative or operative treatment for undisplaced femoral neck fractures: a comparative study of 122 non-operative and 125 operatively treated cases. Injury. 1996;27:583–8.
Barnes R, Brown JT, Garden RS, Nicoll EA. Subcapital fractures of the femur. A prospective review. J Bone Joint Surg Br. 1976;58:2–24.
Chiu FY, Lo WH, Yu CT, Chen TH, Chen CM, Huang CK. Percutaneous pinning in undisplaced subcapital femoral neck fractures. Injury. 1996;27:53–5.
Duckworth AD, Bennet SJ, Aderinto J, Keating JF. Fixation of intracapsular fractures of the femoral neck in young patients: risk factors for failure. J Bone Joint Surg Br. 2011;93:811–6.
Parker MJ, Palmer CR. Prediction of rehabilitation after hip fracture. Age Ageing. 1995;24:96–8.
Deneka DA, Simonian PT, Stankewich CJ, Eckert D, Chapman JR, Tencer AF. Biomechanical comparison of internal fixation techniques for the treatment of unstable basicervical femoral neck fractures. J Orthop Trauma. 1997;11:337–43.
Kauffman JI, Simon JA, Kummer FJ, Pearlman CJ, Zuckerman JD, Koval KJ. Internal fixation of femoral neck fractures with posterior comminution: a biomechanical study. J Orthop Trauma. 1999;13:155–9.
Kammerlander C, Roth T, Friedman SM, Suhm N, Luger TJ, Kammerlander-Knauer U, Krappinger D, Blauth M. Ortho-geriatric service–a literature review comparing different models. Osteoporos Int. 2010;21:S637–46.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Clement, N.D., Green, K., Murray, N. et al. Undisplaced intracapsular hip fractures in the elderly: predicting fixation failure and mortality. A prospective study of 162 patients. J Orthop Sci 18, 578–585 (2013). https://doi.org/10.1007/s00776-013-0400-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00776-013-0400-7