Abstract
Background
Vascular injury after femoral neck fracture can determine its prognosis. This study aimed to determine methods of evaluating femoral neck fracture and accurately predicting the prognosis.
Methods
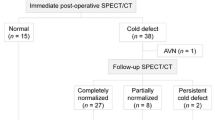
Forty-five patients with a single femoral neck fracture all underwent digital subtraction angiography (DSA) and were divided into three types by DSA. DSA showing three to six supporting band vascular images crossing the fracture line was classified as type I. DSA showing one to two supporting band vascular images crossing the fracture line was classified as type II. When DSA did not show vascular images crossing the fracture line, it was classified as type III. The 45 patients were divided according to age into elderly, middle-aged and youth groups. All cases were given internal fixation operations by a hollow screw under a C-brachial machine. After a follow-up of 6–60 months, avascular necrosis of the femoral head (ANFH) and fracture healing of different type and different ages of patients were evaluated according to symptoms and imaging examinations.
Results
(1) For DSA types I, II and III, the rates of ANFH were 0, 7.14 and 100 %, respectively, and the rates of fracture disunion were 13.3, 7.15 and 0 %, respectively. Therefore, the rate of ANFH is negatively related to the visible supporting band vascular amount on DSA. (2) In the young group, the proportions of types I, II and III were 6.7, 26.67 and 66.7 %, respectively, 18.18, 36.36 and 45.45 % in the middle-aged group and 63.16, 31.58 and 5.27 % in the elderly group. The rates of necrosis for elderly, middle-aged and youth were 10.53, 45.45 and 66.67 %, respectively, and the rates of fracture disunion were 0, 0 and 6.67 %, respectively. So we can draw the conclusion that the amount of supporting band vascular images is inversely proportional to age and the union is directly related to age, but independent of the supporting band vascular amount of DSA showing.
Conclusion
The new classification after superselective angiography is valuable for predicting the prognosis of femoral neck fractures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
For proximal femoral fractures, femoral neck fractures account for 53 %. For femoral neck fractures, nondisplacement fractures (including impacted fractures) account for 37 %, and displacement fractures account for 67 %. Femoral neck fractures occur most often in the elderly. Although the treatment methods are abundant, curative effects vary greatly [1–3]. Therefore, the treatment of femoral neck fractures is controversial.
Currently, femoral neck fracture classification is carried out by using X-ray. There are many types of classifications, summarized as follows: anatomic sites, direction of the fracture line (Pauwel’s classification) [4] and fracture displacement degree (Garden classification) [5]. Anatomic site classification, which relies more on X-ray projection angles, is currently not used very often. Pauwel’s classification is based on the angle of the fracture line and the horizontal line. The bigger the angle is, the bigger the shear force of the fracture site and the more unstable the fracture. However, this classification has two problems. First, there is overreliance on the X-ray projection angle. The fractured neck has to be parallel to the X-ray image. This is difficult to achieve because a femoral neck fracture is always at abduction. Second, some investigators consider that Pauwel’s classification shows no relationship to femoral neck fracture disunion and avascular necrosis of the femoral head (ANFH) [6, 7]. The Garden classification is one of the most widely used methods for classifying femoral neck fractures, and it is divided into types I–IV. It gradually increases from types I to IV with the fracture union rate and with the rate of ANFH. However, determination of displacement is closely related to subjective factors because classification coincidence is very low when different doctors classify one X-ray image [8]. These classification methods are subjective and blinded concerning judgment of femoral neck fracture outcome, and they are limited for guiding femoral neck fracture treatment.
Some investigators have used digital subtraction angiography (DSA) to examine changes in blood flow of the femoral head for determining the gold standard of classification after femoral neck fractures [9–11]. Since April 2004, we have used high selectivity vascular angiography for classification according to the amount of supporting band vascular images from DSA. We predicted the prognosis from the classification and obtained objective evidence from images for choosing treatment methods.
Materials and methods
Materials
Forty-five patients, 26 males and 19 females, all had unilateral femoral neck fractures. Fifteen patients were aged from 26 to 44 years, 11 patients were aged from 45 to 55 years, and 19 patients were aged from 56 to 65 years. The mean age was 45.4 years (45.4 ± 14.2). Twenty-two patients had a fracture on the left side, and 23 had a fracture on the right side. Considering external force, 15 patients had a slight external force and 30 had a violence force. According to the Garden classification, 20 cases were classified as types I and II and 24 as types III and IV. The time from fracture to DSA was 6–18 h. The mean time was 12.7 ± 3.2 h. DSA has a certain operation risk, and this increases treatment fees. DSA was carried out after obtaining patients' informed consents and signed agreements, and institutional review board (IRB) approval from the Institute Research Committee of our University was obtained. The patients were informed that data from the case would be submitted for publication and gave their consent.
DSA methods
We applied a GE INNOVA 2100 digital broad angiography machine to investigate cardiac, hepatic and renal function, and an iodine allergy test was routinely performed preoperatively. Under local anesthesia, catheterization was performed through a femoral artery in a normal limb by using Seldinger technology; the medial and lateral femoral circumflex arteries in the affected limb were examinated by DSA. A 5F Yasiro tube was implanted, allowing selective entry to the medial and lateral femoral circumflex arteries. Angiography was then performed in a tension-free neutral position. The injection rate was 6 ml/s in the femoral circumflex artery (the total amount was 10–15 ml) and 1 ml/s in the retinacular artery (total amount was 1–2 ml). The capture rate was 6, 3 and 2 frames/s in an artery, capillary and vein, respectively. The display time was 2 s, and the capture time was 5, 10 and 15 s in an artery, capillary and vein, respectively, to dynamically observe the retinacular artery of the femoral neck.
Count of the retinacular artery
Femoral head blood supply is mainly derived from the retinacular artery, which arises from the medial and lateral circumflex femoral artery, especially the medial circumflex femoral artery. The retinacular artery courses along the intertrochanteric line, through the hip joint capsule and the synovial fold of the femoral neck, and mainly divides into three groups: the posterior superior retinacular artery, the posterior inferior retinacular artery and the anterior retinacular artery.
The posterior superior retinacular artery, which arises from the medial circumflex femoral artery and courses through the femoral head outside the junction of the femoral head and neck, supplies blood to the femoral head of the lateral 2/3–3/4. The posterior inferior retinacular artery, which arises from the medial circumflex femoral artery and courses through the femoral head along the lower edge of the femoral head cartilage, supplies 1/4–1/2 of the area under the femoral head. The anterior retinacular artery, which arises from the lateral circumflex femoral artery, does not always exist and only supplies a little blood to the femoral head. In this experiment, we mainly dynamically counted the posterior superior and inferior retinacular artery passing through the fracture line by DSA.
Intraobserver analysis of retinacular artery counting: At three different time points (interval >3 days), Dr. Yuan Xi repeatedly counted the number of retinacular arteries across the fracture line from the 45 DSA dynamic images, respectively, and also repeatedly carried out measurements by single factor analysis of variance. When P < 0.05, there were significant differences among the measurement results of the three different time points.
Interobserver analysis of retinacular artery counting: Giving the 45 DSA dynamic images respectively to the three doctors for counting, the number of retinacular arteries across the fracture line were then measured by single factor analysis of variance. When P < 0.05, there were significant differences among the measurement results from the three different doctors.
DSA classification
According to DSA results, fractures were classified as follows: three to six arteries passing through the fracture line were classified as type I; one to two arteries passing through the fracture line, type II; no arteries passing through the fracture line, type III (Fig. 1).
Therapy
With continuous epidural anesthesia or spinal anesthesia, the patient supine on the orthopedic base and straight limb abduction traction and pronation reduction, the successful reset or open reduction were proved by the C-arm X-ray machine. Garden classification of the line index was used to determine the reduction effect, requiring the trabecular bone angle of the femoral and the femoral head to be 160° on anteroposterior radiographs and 180° for the femoral and the femoral head on lateral radiographs. All patients received three 7.3-mm cannulated screw fixation. The hip incision was made at about 5–6 cm, and the locator and the first guide pins were placed, closing the medial cortex 3 cm below the greater trochanter and going through the femoral neck, the pressure trabecular bone and the fracture line, 0.5 cm below the femoral head; the angle between the femoral shaft and the guide wire was 150°. Another two needles went through the tension trabecular bone, above the first guide pin, 0.5 cm below the trochanter, and the three needles were evenly distributed in the femoral neck. Three cannulated screws of appropriate length were screwed into the femoral neck along the guide pin, respectively, and moderately pressured.
After follow-up of 12–72 months, evaluation of femoral head necrosis and fracture disunion was based on the symptoms and images from X-rays, CT, MRI and DSA (Figs. 2, 3).
A 46-year-old male patient with type II DSA. a–d The lateral and medial circumflex femoral arteries all have a retinacular artery crossing the fracture line, and there was no necrosis of the femoral head as shown by CT, MRI and X-ray after 2 years. e The branch of the lateral circumflex femoral artery entering into the femoral head after 2 years. f The branch of the medial circumflex femoral artery entering into the femoral head after 2 years
Statistical
Comparing the rates of ischemic necrosis, fracture disunion of different DSA type patients and different ages using SPSS13.0 statistical software, P < 0.05 was considered statistically significant.
Results
DSA results
The femoral neck and head are mainly supported by two to five retinacular arteries that include three groups. Two to four arteries that are derived from the ascending branch of the medial femoral circumflex artery are the main supporting arteries, which recirculate to the medial and lateral femoral circumflex veins and obturator veins by the retinacular veins. DSA showed that the right and left femoral circumflex arteries have different initial positions and routes. For the right femoral circumflex artery, 41 cases originated from the deep femoral artery, and 4 cases originated from the femoral artery. For the left femoral circumflex artery, 36 cases originated from the deep femoral artery and 9 cases originated from the femoral artery. Thirty-two patients had hemorrhage of the hip joint capsule, and some of them displayed the phenomenon where radiopaque materials had accumulated in the capsule or were extravasated from the breakpoint of the artery. Thirteen patients had bone hemorrhage and DSA showed radiopaque accumulation or extravasation as shown by spots and patchs.
DSA showed that age was related to the number of retinacular vascular crossings of the fracture lines (Table 1). In the young group, the proportion of types I, II and III were 6.7, 26.67 and 66.7 %, respectively. In the middle-aged group, the proportions of types I, II and III were 18.18, 36.36 and 45.45 %, respectively. In the elderly group, the proportion of types I, II and III were 63.16, 31.58 and 5.27 %, respectively. Types I, II and III had equally distributed proportions of 33.33, 31.11 and 35.55 %, respectively. Type I, with a good blood supply, was the most common type in the elderly group. However, type III was more common in the young group.
Intraobserver analysis of retinacular artery counting: In three different time points (interval >3 days), Dr. Yuan Xi repeatedly counted the number of retinacular arteries across the fracture line from the 45 DSA dynamic images and also made repeated measurements by single factor analysis of variance, while the measurement results showed no significant difference (F = 0.673, P > 0.05) (Fig. 4).
Interobserver analysis of retinacular artery counting: Giving the 45 DSA dynamic images respectively to the three doctors for counting, the numbers of retinacular arteries across the fracture line were counted by the three doctors and were then measured by single factor analysis of variance. The results showed that P > 0.05 (F = 0.420, P > 0.05); therefore, we came to the conclusion that the three doctor’s counting results had no significant differences (Fig. 5).
Follow-up and prognosis
After the operation, the patients were followed up for 12 months to 6 years (mean, 39.8 months) to determine the final outcome. X-ray and MRI were performed during follow-up of these patients. Signs of ischemic necrosis appeared 6–27 months postoperatively (mean 15 months). X-rays showed signs of ischemic necrosis of the femoral head with irregular increased density and cystic degeneration, which subsequently subsided. By MRI, the zone of necrosis showed analogic liparoid signs. T1-weighted images showed high-signal intensity, and T2-weighted images showed equal signs, the string sign and double string sign. Nine months postoperatively, fractured lines were clearly seen on X-ray. Weight-bearing ambulation and percussion pain in the axial direction are the diagnostic standard disunion fractures.
Follow-up showed that for type III, all cases had femoral head necrosis; however, none of the cases had disunion fractures. For type I, the rate of necrosis was 0 % and the rate of disunion was 13.34 %. Type II was in between these two types; the postoperative rate of necrosis was negatively correlated with the amount of blood vessels as shown by DSA (Table 2). Type III had the highest rate of necrosis and type I had the lowest. DSA typing was not related to the rate of fracture healing (Tables 2, 3).The rates of necrosis for elderly, middle-aged and youth were 66.67, 45.45 and 10.53 %, respectively, and the rates of fracture disunion were 0, 0 and 6.67 %, respectively. These data demonstrate that the rate of necrosis decreases with age. However, the rate of fracture disunion was directly related to age, but there was no relationship with the amount of blood vessels (Table 3; Fig. 6)
Discussion
Ischemic necrosis of the femoral head and fracture disunion are two of the most common complications of femoral neck fractures [1, 12], which are caused by many related factors. The key to reducing complications is the choice of reasonable treatment. Because of the special blood supply in the femoral head, the occurrence rate of ischemic necrosis in the femoral head is 20–30 % after factures [13], and it can even be as high as 40 % in children and youth. Fracture disunion can be as high as 2.2 % [14]. Our study showed that the average occurrence rate of ischemic necrosis in the femoral head was 37.78, and 66.67 % in youths, which is a little higher than previously reported rates [15–17]. The disunion rate was 6.67 % in middle-aged people, which is a little higher than that previously reported. This discrepancy is probably related to different sample sizes between studies.
The rotation angle of the femoral neck after fracture can affect the blood supply of the femoral head [18]. The pathological mechanism of femoral necrosis and fracture disunion in femoral neck fracture involves damaged blood vessels that cause blood supply deficit or loss.
The blood supply of the femoral head has three main sources as follows. (1) The arterial rings outside of the articular capsule lying in the femoral neck fundus and the femoral neck arterial system are mainly supplied by basilar arterial rings composed of the medial and lateral circumflex femoral artery. The retinacular artery courses along the intertrochanteric line, through the hip joint capsule and the synovial fold of the femoral neck, and it provides blood to the articular cartilage lying in the junction of the femoral head and neck. The femoral head blood supply is mainly derived from the medial circumflex femoral artery of the terminal branches. The superior posterior retinacular artery, which courses through the femoral head outside the junction of the femoral head and neck, supplies blood to the femoral head of the lateral 2/3–3/4. The inferior posterior retinacular artery arises from the medial circumflex femoral artery, which courses through the femoral head along the lower edge of the femoral head cartilage and supplies 1/4–1/2 of the area under the femoral head. (2) The intraosseous arterial system: the femoral shaft nutrient artery, derived from the top of the femur bone marrow, does not reach the head, which means it cannot supply the blood to the femoral head; (3) the teres ligament arterial system, derived from the obturator artery, which generally supplies the fovea of the femoral head section.
The prognosis of femoral neck fractures is related to the specialized vascular anatomical structure. Some investigators have applied DSA technology to analyze blood flow after femoral neck fractures to determine the relationship between the blood distribution and Garden classification [19–21]. Their results demonstrated that there are similarities between their prognosis judgments of femoral neck fractures.
Currently, there are many classifications and treatments for femoral neck fractures [22, 23]. Previously, orthopedics surgery has been used to assess whether femoral head necrosis occurs according to the area of femoral neck fracture or the classification. Many investigators consider that in the arterial circumflex femoral branch, injury of the blood supply is minimal, and the femoral head necrosis rate is lower compared with that in the two anterior types because the circumflex femoral branch travels into the femoral head crossing the articular capsule membrane; base fractures are extracapsular fractures, which are vascularized by the medial and lateral femoral circumflex arterial blood supply, so the blood supply interference is smaller and therefore the necrosis occurrence rate is the lowest. However, according to the anatomy, the Garden classification partly relies on the angle of X-ray projection, and classification is very subjective, so it is not often used to guide femoral neck fracture therapy in the clinic.
Kadakia and Langkamer [24] consider that the Garden classification is an accurate method to predict the rate of fracture disunion and femoral head necrosis. However, it has some disadvantages. For example, it is strongly subjective, and it is difficult to classify types. Therefore, determining prognosis with only X-rays is somewhat subjective.
We were able to clearly observe the dynamic blood supply using DSA to examine the medial and lateral circumflex femoral arteries. It is simple to use, and the patient feels no pain. One person can complete the entire procedure. DSA results can clearly show the extent of arterial injury and the quality of the major blood supply to an artery. DSA is a direct method to determine blood distribution of the femoral head. Femoral neck fracture treatment can be selected according to classification by the amount of remnant artery that penetrates the fracture line.
Our results showed that the quantities of the retinacular artery crossing the fractures is related to patient age. In younger people, damage to the surrounding blood vessels is greater because a greater force is required to fracture the femoral neck. In contrast, in older people, damage to the vascular system is relatively small. Therefore, the incidence of necrosis of the femoral head in elderly patients was lower than that in young adults after a fracture. Our results showed that the amount of vascular injury after femoral neck fracture was negatively correlated with the necrosis rate of the femoral head. Therefore, we can choose an early reduction and internal fixation to DSA types I and II of patients. However, total hip replacement or other early intervention measures that can increase the femoral head blood supply and avoid femoral head necrosis could be applied to DSA type III.
In addition to the severity of femoral head fractures, the routine use of traction and limb positioning in internal rotation also may affect the blood supply to the femoral head. Some investigators [25–27] have found that the retinacular arteries, in addition to the inferior retinacular artery, have varying degrees of occlusion; the femoral head and neck have almost no or poor perfusion, especially the medial circumflex femoral artery. The blood supply of most regions of the femoral head is reduced, and the venous circulation is obstructed if a femoral neck fracture is in an internal rotation position. Therefore, the position of the limb after fracture and the routine use of preoperative traction are questionable. Traction should be performed in an orthopedic bed in the short term if the reduction is to be completed by traction.
DSA after femoral neck fracture is able to define the degree of vascular injury and the status of the blood supply of the femoral head. Therefore, it can be used to enable orthopedic surgeons to perform timely interventions and to improve blood circulation and individualized surgical treatment options. DSA also has some disadvantages, such as expensive inspection fees and surgical risks. Further study is required to reduce inspection costs and surgical risks.
References
Liporace F, Gaines R, Collinge C, Haikewych GJ. Results of internal fixation of Pauwels type-3 vertical femoral neck fractures. J Bone Joint Surg Am. 2008;90:1654–9.
Rogmark C, Flensburg L, Fredin H. Undisplaced femoral neck fractures—no problems? A consecutive study of 224 patients treated with internal fixation. Injury. 2009;40:274–6.
Buord JM, Flecher X, Parratte S, Boyer L, Aubaniac JM, Argenson JN. Garden I femoral neck fractures in patients 65 years old and older: is conservative functional treatment a viable option? Orthop Traumatol Surg Res. 2010;96:228–34.
Pauwels F. Der. Schenkelbalsbrucb: Ein mecbaniscbes problem stutt:Ferdinand Enke Verlag, 1935.
Garden RS. Malreduction and avascular necrosis in subcapital. Fractures of the femur. J Bone Joint Surg (Br). 1971;53:179–83.
Schwarz N. Actual relevance of Pauwels’ classification of femoral neck fractures—a critical review. Z Orthop Unfall. 2010;148:191–7.
Parker MJ, Dynan Y. Is Pauwels classification still valid? Injury. 1998;29:521–3.
Frandsen PA, Andersen E, Madsen F, Skjodt T. Garden’s classification of femoral neck fractures. An assessment of inter-observer variation. J Bone Joint Surg. 1988;70:588–90.
Bonnaire F, Lein T, Engler KJ. Treatment of femoral neck fractures. Chirurg. 2008;79:595–611.
Sim E, Erben W. Intravenous peripheral digital subtraction angiography after stabilization of medial femoral neck fractures. Results and value. Wien Klin Wochenschr. 1992;104:345–8.
Xi Y, Yang L, Jianzhang Z, Sulin X, Lin C, Fuxiang Z. Selective digital subtraction angiography in estimation of blood circulation of femoral head in young patients with femoral neck fracture. J New Med. 2009;19:105–8.
Ly TV, Swiontkowsld MF. Treatment of femoral neck fractures in young adults. Instr Course Lect. 2009;58:69–81.
Lu-Yao GL, Keller RB, Littenberg B, Wennberg LE. Outcomes after displaced fractures of the femoral neck. A meta-analysis of one hundred and six published reports. J Bone Joint Surg Am. 1994;76:15–25.
Togrul E, Bayram H, Gulsen M, Kalaci A, Ozbarlas S. Fractures of the femoral neck in children: long-term follow-up in 62 hip fractures. Injury. 2005;36:123–30.
Ye T, Lunhao B, Qin F. Comparison of related factors between fracture nonunion and avascular necrosis of femoral head after internal fixation with cannulated screws in femoral neck fractures. Chin J Bone Joint Injury. 2009;24:399–402.
Jie W, Li Z, Man-yi W. The incidence and prognosis of avascular necrosis of femoral head after operation of femoral neck fractures. Chin J Orthop. 2005;25:1–6.
Raaymakers EL. Fractures of the femoral neck: a review and personal statement. Acta Chir Orthop Traumatol Cech. 2006;73:45–59.
Jing-Guang Q, Yia-Wei S, Xiao T. Examination of femoral-neck structure using finite element model and bone mineral density using dual-energy X-ray absorptiometry. Clin Biomech. 2009;24:47–52.
Blomfeldt R, Tornkvist H, Ponzer S, Soderqvist A, Tidermark J. Internal fixation versus hemiarthroplasty for displaced fractures of the femoral neck in elderly patients with severe cognitive impairment. J Bone Joint Surg (Br). 2005;87:523–9.
Xiu-Jun Y, Xiang-Sheng X. The early influence of hip traction or internal rotating on blood circulation of femoral head with neck fracture: study by superselective digital subtraction arteriography. Chin J Radiol. 2005;39:812–6.
Yang L, Fang-zhou C, Xian-nian Z, Xi Y, Jian-zhang Z, Shu-lin X, Lin C. Cannulated screw fixation under C-arm guidance using digital subtraction angiography and Garden typing: therapeutic effect of femoral neck fracture. J Clin Rehabil Tissue Eng Res. 2009;13:6951–4.
Raaymaker ELFB.The non operative treatment of impacted femoral neck fractures. Injury. 2002;33: SC8–SCl4.
Liporace F, Gaines R, Collinge C, Haidukewych GJ. Results of internal fixation of Pauwels type-3 vertical femoral neck fractures. J Bone Joint Surg Am. 2008;90:1654–9.
Kadakia A, Langkamer VG. Cancellous screw fixation of undisplaced femoral neck fractures in over 70 years. Injury Extra. 2007;38:146–7.
Mao YJ, Wei J, Zhou L, Wang MY, Su JG. Related factor analysis of avascular necrosis of the femoral head after internal fixation with cannulated screws in femoral neck fractures. Zhong hua Yi Xue Za Zhi. 2005;85:3256–9.
Zhao DW, Wang BJ, Wang WM, Yu XG, Wang TN, Sun Q. Evaluation of hemodynamic changes by digital subtraction angiography after treatment of avascular osteonecrosis of femoral head with vascularized bone flaps. Zhonghua Yi Xue Za Zhi. 2006;86:438–41.
Dai P, Zheng Z, Sun S. Blood supply reestablishment of avascular necrosis of femoral head with digital subtraction angiography. Zhonghua Yi Xue Za Zhi. 1998;78:195–7.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Liu, Y., Li, M., Zhang, M. et al. Femoral neck fractures: prognosis based on a new classification after superselective angiography. J Orthop Sci 18, 443–450 (2013). https://doi.org/10.1007/s00776-013-0367-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00776-013-0367-4