Abstract
The “mitochondrial amidoxime reducing component” (mARC) is the most recently discovered molybdenum-containing enzyme in mammals. All mammalian genomes studied to date contain two mARC genes: MARC1 and MARC2. The proteins encoded by these genes are mARC-1 and mARC-2 and represent the simplest form of eukaryotic molybdenum enzymes, only binding the molybdenum cofactor. In the presence of NADH, mARC proteins exert N-reductive activity together with the two electron transport proteins cytochrome b5 type B and NADH cytochrome b5 reductase. This enzyme system is capable of reducing a great variety of N-hydroxylated substrates. It plays a decisive role in the activation of prodrugs containing an amidoxime structure, and in detoxification pathways, e.g., of N-hydroxylated purine and pyrimidine bases. It belongs to a group of drug metabolism enzymes, in particular as a counterpart of P450 formed N-oxygenated metabolites. Its physiological relevance, on the other hand, is largely unknown. The aim of this article is to summarize our current knowledge of these proteins with a special focus on the mammalian enzymes and their N-reductive activity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Molybdenum is an essential trace element in nearly all organisms [1, 2]. Molybdenum-containing enzymes are redox active and catalyze metabolic reactions in nitrogen, sulfur, and carbon cycles [3]. Initially, only three molybdenum enzymes, e.g., sulfite oxidase (SO), xanthine oxidoreductase, and aldehyde oxidase, were known in mammals and other animals. Investigation of the aerobic reduction of amidoxime structures led to the discovery of the fourth mammalian molybdenum enzyme mitochondrial amidoxime reducing component (mARC) in our laboratory [4]. mARC belongs to the SO family of molybdenum-containing enzymes [5, 6]. It is part of an N-reductive enzyme system consisting of mARC, cytochrome b5 type B and NADH cytochrome b5 reductase [4, 7, 8] (Fig. 1).
Mitochondrial amidoxime reducing component proteins represent the simplest mammalian molybdenum enzymes. Heterologous human proteins expressed in Escherichia coli are purified as monomers [9]. A recent study proposed that human mARC-1 might reside in three main high oligomer protein complexes of more than 350 kDa in size [10].
To our knowledge, no additional prosthetic groups or cofactors besides molybdenum cofactor (Moco) are known for both mARC proteins and no crystal structures of these proteins are available. All mammalian genomes studied to date contain two mARC genes: MARC1 and MARC2. In humans, they are organized in tandem arrangement on chromosome 1 (1q41) with an interspace of only 5,044 base pairs and show an overall sequence identity/similarity of 66/80 % [9]. Human MARC1 (NM_022746.3) contains a predicted open reading frame (ORF) of 1,011 base pairs and encodes a mARC-1 protein consisting of 337 amino acids. The predicted and verified ORF of human MARC2 (NM_017898.3) contains 1,005 base pairs and encodes a mARC-2 protein consisting of 335 amino acids. Based on computational analysis, both proteins contain an amino-terminal mitochondrial signal sequence, a predicted β-barrel domain and a MOSC domain near the carboxyl-terminus [11]. The carboxyl-terminal domain of Moco-sulfurase was the eponym of this superfamily: “MOSC” refers to “Moco-sulfurase carboxy-terminal domain” [11]. The C-terminal domain of the human Moco-sulfurase shows an overall sequence identity/similarity of 25/47 % to human mARC-1 and 26/47 % to human mARC-2, respectively.
Besides mARC-1 and mARC-2, the MOSC superfamily comprises in eukaryotes solely the Moco-sulfurase which is involved in molybdenum cofactor maturation [12] and in prokaroytes among others the proteins YcbX and YiiM [11]. The MOSC domain is further characterized by an absolutely conserved “MOSC-cysteine” in positions 273 in case of human mARC-1 and 272 in case of human mARC-2 [11, 12]. In addition to that, all investigated proteins of the MOSC superfamily bind the Moco [9, 13, 14].
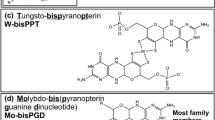
Molybdenum cofactor of mARC
With the exception of bacterial molybdenum nitrogenase, all known molybdenum-dependent enzymes harbor a pterin-based Moco in their active site. According to their fivefold coordination around the molybdenum center eukaryotic molybdenum enzymes are classified into two families: The di-oxo molybdenum enzymes of the SO family contain a cysteine-derived sulfur, while remaining molybdenum coordination spheres are occupied by two oxygen atoms and two dithiolene sulfurs of the pterin. In contrast, the mono-oxo molybdenum enzymes of xanthine oxidase (XO) family do not display any protein-dependent molybdenum coordination. In this family, the transition element coordinates dithiolene sulfurs of the pterin moiety, two oxygen and the so-called inorganic “terminal sulfur” [12]. The latter one is essential for catalytic activity and is inserted enzymatically by the aforementioned Moco-sulfurase [15].
Up to now, several approaches were taken to characterize the molybdenum center of mARC and the following section shall provide a chronological report of the respective findings:
Initially, membership to the XO family could be excluded for human mARC by biochemical methods. A major feature of enzymes of the XO family is that the terminal sulfur atom can easily be abstracted from the molybdenum center by cyanide treatment, which leads to inactivation of the respective enzyme [16, 17]. Yet, cyanide treatment of human mARC proteins neither released sulfur (as thiocyanate) nor significantly affected the activities, indicating that mARC proteins either do not represent members of the XO family or the terminal sulfur ligand is bound to their molybdenum center in an extremely robust and cyanide-insensitive manner [9]. By co-incubation of mARC apoproteins with sulfur-free cofactor, however, the latter alternative was undoubtedly excluded as the reductive activity of mARCs was readily reconstituted [9]. To prove whether or not mARC enzymes rather belong to the SO family of molybdenum enzymes, the same researchers substituted each of the nine cysteines of human mARC-1 (and an additional one for human mARC-2) for serine and looked for a possible aberration from the wild-type EPR spectrum as has been found earlier for other SO family enzymes [18]. Even though both mARC wild-type proteins presented spectra very similar to those known from SO family enzymes, the authors concluded that the Moco inserted in mARC enzymes possesses a ligation sphere markedly different from SO family enzymes due to the fact that the spectra of all cysteine variants appeared to be indistinguishable from the wild-type spectrum [9].
Only 1 year later, structural studies using pulsed EPR spectroscopy and 17O-labeling were performed to determine the nature of the remaining ligands besides the dithiolene sulfurs of the pterin in the Mo(V) state of human mARC-2 [19]. Besides an equatorial hydroxyl group and an apical oxo ligand, the equatorial fifth ligand was proposed to derive from the protein and to be represented most likely by serine, cysteine or methionine. In accordance with these findings, substitution of the absolutely conserved “MOSC-cysteine” to alanine in the corresponding enzyme of green alga abrogated the reductive activity completely, suggesting that this cysteine is indeed part of the active site [5]. In light of these observations, Wahl and coworkers reinvestigated the variant in which the “MOSC-cysteine” of hmARC-1 has been changed to serine and whose EPR spectrum did not differ from that of the wild-type protein. In fact, sequencing of the plasmid DNA isolated from the bacterial culture used for expressing this particular variant demonstrated that bacteria of the “MOSC-cysteine” variant were contaminated with bacteria carrying the DNA of one of the wild-type-like variants, thus covering the true identity of the “MOSC-cysteine” variant (Wahl, Reichmann, Mendel, Bittner, personal communication). When analyzing the protein derived from a “clean” expression culture, however, it became obvious that mutation of the MOSC-typical cysteine residue indeed results in abrogation of the enzymatic activity and significant perturbation of the EPR spectrum (Reichmann, Hille, Niks, Mendel, and Bittner, personal communication, and own observation; Erratum to be submitted to J. Biol. Chem. soon). This indicates that a sulfur derived from a proteinogenic cysteine, namely of the “MOSC cysteine”, is indeed part of the molybdenum active site in mARCs, most likely by coordinating the metal in Moco. A recently performed X-ray absorption structure analysis likewise indicates the presence of a dioxo Mo(VI)-site with a sulfur representing an equatorial ligand of Mo, as typical for SO family enzymes [20].
The localization of mARC
All mammalian genomes encode two mARC proteins. These molybdoproteins are widely expressed in different tissues. Human mARC-1 shows highest mRNA expression levels in adipocytes. Highest expression levels of human mARC-2 are found in kidney, the thyroid gland, liver, and small intestine [21, 22]. Immunoblotting with antibodies directed to human mARC-1 and mARC-2 confirmed this tissue distribution on the protein level in porcine mitochondria, with high mARC-1 levels found in pancreas, liver and kidney while high mARC-2 levels were found in kidney, liver, and thyroid gland [23]. Interestingly, in most human cell lines and tissues, only mARC-1 is highly abundant [24].
Mitochondrial amidoxime reducing component proteins, as indicated by their names, are localized in mitochondria [9]. In mouse mitochondria of various tissues, either mARC-2 [9, 25] or both isoforms [26, 27] were found.
Studies with porcine and murine tissue found high protein levels of mARC-1 in mitochondrial subcellular fractions of liver, kidney, and pancreas; whereas mARC-2 was abundant in liver, kidney, thyroid gland, lung, small intestine, and pancreas which is in good agreement with high N-reductive activity in mitochondrial fractions obtained from these tissues. All tissues investigated so far showed N-reductive activity and expression of at least one mARC isoform [23].
The discovery of mARC was based on the isolation of mARC-2 from the outer mitochondrial membrane of porcine liver [4] and by now both mARC proteins were identified in the outer mitochondrial membrane of rat and porcine liver [10, 28, 29]. A recent study with human cell lines revealed that the mARC-1 protein is associated with the mitochondrial membrane with an N(in)–C(out) membrane orientation. The catalytic domain is localized at the C-terminus and exposed to the cytosol which is consistent with localization and orientation of cytochrome b5 type B and NADH cytochrome b5 reductase [30, 31]. This submitochondrial localization is in agreement with a maximum of N-reductive activity detectable in the outer mitochondrial membrane [29, 32, 33].
A dual localization in mitochondria and peroxisomes is described for only one of the two mARC proteins (mARC-2 in mice and rats) [34, 35]. It is very likely that mARC is a peroxisomal membrane protein. The peroxisomal targeting of matrix proteins depends on short sequences known as peroxisomal targeting signal type 1 and type 2 [36]. The mechanisms responsible for targeting of peroxisomal membrane proteins are still rather poorly understood. The peroxisomal sorting information is not linked to a specific amino acid sequence, but rather with physiochemical characteristics of the peroxisomal membrane targeting signal (mPTS) sequence [37]. It is assumed that mPTSs consist of short stretches of basic amino acids associated with hydrophobic transmembrane domains [36]. It is remarkable that the transmembrane domain of both mARC proteins is followed by such a short stretch of arginine residues. However, although this may be a hint of a potential mPTS in mARC, precise identification and analysis of peroxisomal targeting signals are not possible with the current state of research.
To our knowledge, there are no reports or indications for a peroxisomal localization of cytochrome b5 and its reductase. It seems that mitochondrial cytochrome b5 is exclusively localized in theses cell organelles [38]. Since specific knockdown of this mitochondrial heme protein dramatically reduces N-reductive activity [8, 28], one may speculate that the N-reductive enzyme system is exclusively localized in mitochondria. Thus, it is probable that a peroxisomal localized mARC has a different function than N-reductive activity. In peroxisomes, mARC seems to be involved in so far unknown redox reactions either as a stand-alone protein or with other electron transport proteins different from cytochrome b5 and its reductase. Due to the general function of peroxisomes, it is possible that mARC is involved in the cell response to oxidative stress [22] or in lipid metabolism [36].
mARC and its N-reductive enzyme system
Characterization of the heterologously expressed human mARC proteins and RNAi studies demonstrated that N-reductive activity depends on the presence of cytochrome b5 type B (CYB5B, NM_030579.2), NADH cytochrome b5 reductase (CYB5R3, NM_007326.4) and NADH under aerobic conditions [8, 28, 29, 39]. In addition to that, results of further studies demonstrated that the prosthetic groups Moco and heme are essential for N-reductive activity [8, 9].
N-reductive activity can be achieved by reconstitution assays using either mARC-1 or mARC-2 as molybdenum enzyme with high overlapping substrate specifities [7, 9, 23, 29, 39] using different classes of N-hydroxylated substrates (N-hydroxylated amidinohydrazones, sulfhydroxamic acids, hydroxylamines, E-/Z-isomers of oximes). So far, only N-oxides are exclusively reduced by mARC-1 [40].
Cytochrome b5 and NADH cytochrome b5 reductase are important electron transport proteins involved in many physiological processes. The flavoenzyme NADH cytochrome b5 reductase is able to transfer electrons from NADH to the heme-containing cytochrome b5 [41–43].
Two isoforms of cytochrome b5, type A and type B, are encoded by different genes [30]. Type A is localized as a membrane-bound form in microsomes and as a soluble form in erythrocytes [30, 44]. Type B is localized at the outer mitochondrial membrane [31, 45, 46]. Although N-reductive activity can be achieved in an in vitro reconstitution assay with both cytochrome b5 isoforms [47], recently performed knockout and knockdown studies showed that only the mitochondrial isoform is involved in the N-reductive pathway [8, 28].
This composition of the N-reductive enzyme is identical with the domain structure of another eukaryotic molybdenum enzyme: nitrate reductase consists of a cytochrome b5-, a NADH cytochrome b5 reductase-, and a Moco-binding domain [48], but there are no sequence similarities between mARC and nitrate reductase. Therefore, it should be kept in mind that the mitochondrial N-reductive complex with its mARC protein represents the first case of a eukaryotic molybdenum enzyme consisting of separate proteins.
It is generally accepted that the mARC-containing enzyme system plays a major role in the reduction of N-hydroxylated substrates [7]. These substrates can be either part of the activation of N-hydroxylated prodrugs [39, 49, 50] of detoxification pathways [23] or in general as the reducing counterpart of N-oxygenated metabolites formed by P450 enzymes (Fig. 2).
N-oxygenation by P450 enzymes and reduction by mARC (bioreversible reaction). Examples of N-oxygenated structures see Fig. 3
It is supposed that N-hydroxylated substrates might be reduced at the molybdenum cofactor by cleavage of the N–O bond, in accordance with the described mechanism of nitrate reduction [51] and that molybdenum cycles between Mo(IV) and Mo(VI) oxidation state. Reducing equivalents are transferred from NADH via FAD (NADH cytochrome b5 reductase) to heme (cytochrome b5) and regenerate the catalytically competent Mo(IV) state.
mARC and the amidoxime prodrug strategy
Amidines are known as functional groups in drugs. They are used for the treatment of several different diseases and belong to the classes of trypsin-like serine protease inhibitors like factor Xa inhibitors, thrombin inhibitors [52], factor VIIa inhibitors [53], and urokinase-type plasminogen activators [54]. They are also used as anti-parasitic, anti-bacterial, and anti-malarial agents [55–58], or antiplatelet GPIIb/IIIa-receptor antagonists [59].
One problem of amidines concerning their use as approved drugs is their strong basicity. They are easily protonated at the sp2 hybridized nitrogen and form resonance-stabilized cations. Unfortunately, this protonation occurs under physiological conditions. Thus, amidines are poorly absorbed by diffusion from the gastrointestinal tract and show an insufficient oral absorption and an unacceptable bioavailability [60, 61].
This problem can be solved by the use of prodrugs, an established tool for improving oral bioavailability. Prodrugs are bioreversible derivatives of drug molecules that are converted enzymatically and/or chemically in vivo to release the active form of the parent drug [62]. The most promising approach for an improved bioavailability of the amidine moiety is the amidoxime prodrug strategy. Because of the electronegativity of the oxygenation these compounds are no longer protonated under physiological conditions as the basicity is extremely low. Thus, amidoximes (N-hydroxyamidines) exhibit good oral availability and are rapidly reduced to the pharmacologically active amidines by mARC.
The principle “amidoximes instead of amidines” was first developed for the aromatic diamidine pentamidine [63, 64], a drug with trypanocidal activity and efficacy towards pneumonia caused by Pneumocystis jirovecii [65]. Both amidine groups were replaced by amidoximes and the resulting prodrug showed a significant increase of oral bioavailability. Data obtained from several studies showed that the amidoxime prodrug is efficiently converted to its active amidine metabolite via a two-step reduction [64, 66].
This strategy was applied to many other anti-parasitic and anti-bacterial diamidine-type compounds, whose amidoxime prodrugs are converted to their active forms after oral administration [67–69]. A great field of application for amidoxime prodrugs is antithrombotics [61], some of them are tested in clinical trials. It is also possible to modify the amidoxime prodrug principle, e.g., by methylation [70–73] or esterification [73, 74].
A prominent example for a “double prodrug” (or pro-prodrug) is ximelagatran (Astra Zeneca), the first approved drug of an oral direct thrombin inhibitor [75]. This pharmacological inactive molecule is transformed in vivo by esterases and the mARC-containing N-reductive enzyme system to its active form melagatran [76]. Unfortunately, during clinical studies of long-term treatment elevated levels of a transaminase enzyme occurred in about 7–8 % of the patients [77]. No evidence was found for additional metabolism pathways or the formation of active metabolites [78]. A pharmacogenetic study suggested a possible immunogenetic pathogenesis of this adverse reaction and no connection to the prodrug principle [79].
A recent study characterized the kinetic parameters for the activation of the model substrate benzamidoxime by protein variants encoded by single-nucleotide polymorphisms (SNPs). SNPs are one kind of short variations of DNA sequence. If they fall within coding sequences of genes they are able to change the amino acid sequence of the encoded protein (nonsynonymous SNPs) which can result in an altered function of the protein. SNPs are known for both human mARC genes. Currently, nonsynonymous SNPs are registered for 39 positions in MARC1 and for 26 positions in MARC2 [80]. Kinetic parameters of six protein variants of mARC-1 and two variants of mARC-2 were investigated by in vitro biotransformation studies. Statistically significant decreases of kinetic parameters were only detectable in variants of mARC-2. But genotyping of genetic variants in the mARC genes showed that these two variants of MARC2 were of low frequency in a cohort of 334 healthy Caucasians, carriers of the homozygous variant were not detectable. Inducing a loss of function in the mARC-1 protein was only possible after replacement of more than two amino acids. Because of their rareness these variants might not have any clinical relevance [81]. The same result provided a study analyzing four protein variants of cytochrome b5 type B [8].
The mARC-containing N-reductive enzyme system is responsible for activating all amidoxime prodrugs tested so far [39, 49, 50] (Fig. 3). Recently, the amidoxime prodrug strategy was applied to another serine protease inhibitor. Mesupron® (WX-671) is the orally available prodrug of the urokinase inhibitor WX-UK1 and is converted to its active form by the mARC-containing N-reductive enzyme system [50, 54]. It has successfully passed clinical phase II trials. Furthermore, participation of the mARC-containing N-reductive enzyme system in the reduction of N-oxides (amitriptyline-N-oxide, nicotinamide-N-oxide), oximes (2,4,6-trimethylacetophenone oxime) and N-hydroxyamidinohydrazones (guanoxabenz) is proven. Interestingly, N-oxides are solely reduced by mARC-1 [40].
The finding that mARC is predominantly involved in activation of N-hydroxylated prodrugs can be used for prodrug feasibility studies: Simple in vitro pilot studies using mitochondria or isolated enzymes can be performed to ensure prodrug activation before extensive in vivo studies are started. By doing so, time and costs during development of prodrugs can be reduced. For drug metabolism studies mitochondria should also be used to get a complete picture of nitrogen metabolism.
First indications for putatively physiological functions of mARC
Although there is no doubt about the N-reductive activity of mARC, the physiological function of mARC is not fully understood. In particular, it has to be questioned whether functions of mARC-1 and mARC-2 are either overlapping or distinct. In the following section, the current knowledge of possible physiological and pathophysiological roles of mARC is summarized.
Involvement in the NO pathway
A putative physiological substrate could be the NO precursor N ω-hydroxy-l-arginine, which can be reduced under aerobic conditions in vitro by mitochondrial fractions of different tissues and by the heterologously expressed enzyme system containing mARC-1 or mARC-2 [29]. Therefore, it might be possible that the N-reductive enzyme system acts as one key enzyme in the l-arginine-dependent biosynthesis of NO (Fig. 4). Recently, another study demonstrated that NO formation can also be catalyzed by the reduction of nitrite by the mARC-containing N-reductive enzyme system under anaerobic conditions [82].
Overview of the influence of the mARC-containing N-reductive enzyme system on NO biosynthesis according to [29] and [82]. In the arginine-to-NO pathway l-arginine is oxidized to l-citrulline and NO. This pathway is catalyzed by NOS via the NO precursor N ω-hydroxy-l-arginine (NOHA). On the one hand, the intermediate NOHA acts as an inhibitor of arginase leading to an enlarged substrate pool for NOS and therefore leading to an enhanced NO formation. On the other hand, the mARC-containing N-reductive enzyme system might have a putative physiological function in reducing NOHA to l-arginine and therefore lowering the endogenous NOHA and NO concentrations under aerobic conditions. In the inorganic nitrate–nitrite–NO pathway the mARC-containing N-reductive enzyme system can generate NO from nitrite under anaerobic conditions
Metabolic detoxification
Both human mARC proteins are involved in the reduction of N-hydroxylated nucleobases and nucleosides. Reduction of N-hydroxycytosine, N-hydroxyadenine, cytidine and adenine was investigated (Fig. 3) [9, 23]. In addition, two other Moco-binding MOSC proteins in prokaryotes have been found to participate in this detoxification pathway of mutagenic DNA bases as well [13, 83, 84]. This hypothesis of a mARC-mediated role in detoxification reactions is also supported by a study which describes a significant and progressively changed down-regulated expression of human mARC-2 in colon tumors in samples of human tissue [85]. Therefore, it appears likely that one of the physiological functions of mammalian mARC proteins could be the prevention of accumulation of mutagenic substances in the cell.
Furthermore, the mitochondrial enzyme system is involved in detoxification of hydroxylamines (Fig. 3) like sulfamethoxazole hydroxylamine. The sulfonamide sulfamethoxazole is metabolized by P450 to the toxic hydroxylamine metabolite [86]. This is the first step of a toxification pathway which is responsible for hypersensitivity reactions of this anti-infective drug [87]. Thus, mARC is the counterpart of P450 catalyzed N-oxygenation and the reducing partner in the metabolic cycle of N-oxygenation and N-reduction. RNAi studies in a human cell line confirmed that both mARC proteins were capable of reducing the toxic sulfamethoxazole metabolite in cell metabolism [88].
Diabetes mellitus
Expression of mARC-2 is up-regulated in diabetic kidneys of Goto-Kakizaki rats, a prototype for the study of non-overweight type 2 diabetes, and by glucose in human and rat renal cells [22, 89]. Therefore, it might be possible that there is a connection between only one specific mARC form and diabetes mellitus. This is supported by a further study describing that certain structural variations of DNA (copy number variations) in human MARC2 might be related with type 1 and type 2 diabetes [90].
Energy metabolism
High N-reductive activity was found in adipose tissue of rodents [32]. Expression of mARC-2 and N-reductive activity are significantly increased during differentiation of murine cells into mature adipocytes expression [28, 91], indicating that the enzyme is regulated under lipogenic conditions. Furthermore, down-regulation of murine mARC-2 caused impaired lipid synthesis [28]. In this context, it also has to be mentioned that genome-wide association studies suggested a possible association of one SNP in human MARC1 with plasma lipid traits [92] and altered lipid response to fenofibrate [93]. Another study demonstrated that expression and activity of the N-reductive enzyme system are affected by fasting and high-fat-diet in mice [94].
Other possible functions
As mentioned before, MARC1 and MARC2 have been the subject of some genome-wide association studies, performed to search for genetic susceptibility to disease. Up to now, a causal link between the mARC genes and the investigated disease was not detected. However, three studies detected intronic SNPs in MARC1 and MARC2, which are located in the non-coding regions of the genes, and suggested a possible association with methamphetamine dependence in a Japanese and a Taiwan cohort [95] and with extrapyramidal side effects in samples of schizophrenia patients with antipsychotic medication [96].
Consequences of mARC deficiency
Knockout mice are used as animal models for studying the role of genes and for drawing conclusions about the probable function of the encoded protein. Interestingly, the mouse genome informatics (MGI) database reports about a MARC2 knockout mouse [97]. Male and female mice carrying the homozygous genotype are alive. The phenotype of the male mice is characterized by an increased startle reflex in their behavior, a decreased total body fat amount, and an increased lean body mass. The latter symptoms of the knockout mice seem to match to the recently observed finding that fasting affects mARC protein expression and N-reductive activity in wild-type mice [94]. Moreover, exaggerated startle reactions were described in a newborn with molybdenum cofactor deficiency as well [98]. The female mice exhibit an increased leukocyte cell number and an increased circulating glucose level. This observation is in good agreement with previous findings that there might be a link between mARC and diabetes [22, 89].
In humans, a heterozygous knockdown of MARC1 and MARC2 is only reported in connection with the 1q41q42 microdeletion syndrome. Children are alive and their phenotype is characterized by midline defects (cleft palate, diaphragmatic hernia), seizures, and mental retardation or developmental delay. Dysmorphic features are present in all patients at varying degrees. Of course, these observations are not solely attributed to the deletion of MARC1 and MARC2. Several other genes within the region, in which deletion of all patients is overlapping, possibly play a more important role on the phenotype [99–101].
In contrast, the deficiency in the biosynthesis of the Moco mentioned above results in the pleiotropic loss of all molybdenum-dependent enzymes (SO, xanthine oxidoreductase, aldehyde oxidase, and mARC) in human. The severe phenotype of Moco-deficient patients is characterized by progressive neurological damage leading in most cases to early childhood death, mainly caused by the deficiency of SO that protects the organism, in particular the brain, from elevated levels of toxic sulfite [102, 103].
Differences between mARC-1 and mARC-2
Up to now, all tested N-hydroxylated substrates were converted by mARC in reconstituted enzyme assays with cytochrome b5 and its reductase. Both recombinant mARCs catalyze the reduction of many substrates like benzamidoxime with similar efficiency and RNAi studies confirmed that both molybdoproteins are capable of reducing N-hydroxylated substrates in cell metabolism [8, 88]. It should be noted that some substrates like N 4-hydroxycytosine were clearly more efficiently reduced by human mARC-1 [23], whereas, e.g., sulfamethoxazole hydroxylamine was more efficiently converted by human mARC-2 [88]. Taken together, it is likely that although both mARCs act on the same substrates, each isoform has its own set of preferred substrates. Recently, it was reported that the N-oxides amitriptyline-N-oxide and nicotinamide-N-oxide are exclusively reduced by human mARC-1 [40]. These findings indicate structural differences in the catalytic centers of the two molybdoproteins, which would allow mARC-1 and mARC-2 to participate in different metabolic reactions.
Besides N-reductive metabolism, it is striking that in many cases the abundance/expression of either mARC-1 or mARC-2 correlates with the investigated traits, as describes above. In addition, only one mARC form could be detected in peroxisomes and it is very likely that this subcellular fraction shows no N-reductive activity. Thus, mARC might be an example for an “echoform” designation for a dually localized protein with totally different functions in each of the compartments—in contrast to the term “isoform”, which describes proteins with the same activity but different amino acid sequences [104].
In this context, it should be noted that classification of the terms “mARC-1” and “mARC-2” in different species is made on the basis of sequence alignments to the human proteins. However, one should be careful by using “form-1”/“form-2” assignment when results of different species are compared. It could be speculated that, e.g., the function of human mARC-1 is equated with the function of mARC-2 and vice versa in another species.
Conclusions
Investigation of the aerobic reduction of amidoxime structures led to the discovery of the molybdenum enzyme mARC. All mammalian genomes studied to date contain two mARC genes (MARC1 and MARC2) which encode the two proteins mARC-1 and mARC-2. Both mARC proteins show similar biochemical characteristics and are able to reduce several N-hydroxylated substrates together with mitochondrial cytochrome b5 and NADH cytochrome b5 reductase in the presence of NADH.
At present, there is convincing evidence to support the following key ideas: (i) The mitochondrial enzyme system is involved in N-reductive pathways in particular detoxification of toxic hydroxylamines. Besides, also activation of amidoxime prodrugs is catalyzed. (ii) The mARC-containing enzyme system is involved in the NO pathway by aerobic reduction of the NO-precursor NOHA and an aerobic nitrite reduction. (iii) There are noticeable differences in subcellular localization of the two molybdenum enzymes which indicates that the function of mARC is not necessarily associated with the N-reductive enzyme system in mitochondria. (iv) Expression of at least one mARC protein is affected by glucose. (v) mARC is linked to lipid metabolism.
Despite the established involvement of both mitochondrial localized mARC proteins in N-reductive metabolism, there are still some unanswered questions: Has the observed in vitro reduction of, e.g., DNA base analogs actually an impact on the cell viability and apoptosis? Is this protection mechanism mediated by both or only one mARC protein?
It was shown in vitro that NOHA is a possible endogenous substrate of the mARC-containing enzyme system. Has the reduction of this NO precursor an effect on cellular NO production?
The fact that only one mARC protein has a dual localization in mitochondria and peroxisomes is an interesting biological problem for investigation: Why is only one mARC protein directed to peroxisomes and which are the physiochemical characteristics of its mPTS sequence? What is the catalytic function of peroxisomal mARC and is mARC linked to other redox proteins in this organelle? Is there a link to the proposed connection of mARC with lipid metabolism and its peroxisomal localization?
A major goal is the creation of the missing mARC knockout mice (mARC-1−/− and mARC-1−/−/mARC-2−/−double knockout) and long-term phenotypic characterization of all kinds of knockout. Are the double knockout mice viable? Do these animal models develop cancer and diabetic mellitus or do they have an unbalanced lipid metabolism or cardiovascular diseases? Can differences between mARC-1 and mARC-2 knockout be observed? The elucidation of the three-dimensional structure of the mARC proteins is also a big challenge for the future.
Analyses of these topics are the major challenge of future research and will help us to elucidate the physiological function of mARC-1 and mARC-2.
Abbreviations
- Cyt b5 :
-
Cytochrome b5 type B
- Cyt b5 R:
-
NADH cytochrome b5 reductase
- mARC:
-
Mitochondrial amidoxime reducing component
- Moco:
-
Molybdenum cofactor
- MOSC:
-
Moco-sulfurase C-terminal domain
- mPTS:
-
Peroxisomal membrane targeting signal
- NO:
-
Nitric oxide
- NOHA:
-
N ω-hydroxy-l-arginine
- SO:
-
Sulfite oxidase
- SNP:
-
Single-nucleotide polymorphism
- XO:
-
Xanthine oxidase
References
Truong HN, Meyer C, Daniel-Vedele F (1991) Biochem J 278:393–397
Zhang Y, Gladyshev VN (2008) J Mol Biol 379:881–899
Hille R (1996) Chem Rev 96:2757–2816
Havemeyer A, Bittner F, Wollers S, Mendel R, Kunze T, Clement B (2006) J Biol Chem 281:34796–34802
Chamizo-Ampudia A, Galvan A, Fernandez E, Llamas A (2011) Eukaryot Cell 10:1270–1282
Hille R, Hall J, Basu P (2014) Chem Rev 114:3963–4038
Havemeyer A, Lang J, Clement B (2011) Drug Metab Rev 43:524–539
Plitzko B, Ott G, Reichmann D, Henderson CJ, Wolf CR, Mendel R, Bittner F, Clement B, Havemeyer A (2013) J Biol Chem 288:20228–20237
Wahl B, Reichmann D, Niks D, Krompholz N, Havemeyer A, Clement B, Messerschmidt T, Rothkegel M, Biester H, Hille R, Mendel RR, Bittner F (2010) J Biol Chem 285:37847–37859
Klein JM, Busch JD, Potting C, Baker MJ, Langer T, Schwarz G (2012) J Biol Chem 287:42795–42803
Anantharaman V, Aravind L (2002) FEMS Microbiol Lett 207:55–61
Hille R, Nishino T, Bittner F (2011) Coord Chem Rev 255:1179–1205
Kozmin SG, Leroy P, Pavlov YI, Schaaper RM (2008) Mol Microbiol 68:51–65
Wollers S, Heidenreich T, Zarepour M, Zachmann D, Kraft C, Zhao Y, Mendel RR, Bittner F (2008) J Biol Chem 283:9642–9650
Bittner F, Oreb M, Mendel RR (2001) J Biol Chem 276:40381–40384
Massey V, Edmondson D (1970) J Biol Chem 245:6595–6598
Wahl RC, Rajagopalan KV (1982) J Biol Chem 257:1354–1359
George GN, Garrett RM, Prince RC, Rajagopalan KV (2004) Inorg Chem 43:8456–8460
Rajapakshe A, Astashkin AV, Klein EL, Reichmann D, Mendel RR, Bittner F, Enemark JH (2011) Biochemistry 50:8813–8822
Giles LJ, Ruppelt C, Yang J, Mendel RR, Bittner F, Kirk ML (2014) Inorg Chem 53:9460–9462
Su AI, Wiltshire T, Batalov S, Lapp H, Ching KA, Block D, Zhang J, Soden R, Hayakawa M, Kreiman G, Cooke MP, Walker JR, Hogenesch JB (2004) PNAS 101:6062–6067
Malik AN, Rossios C, Al-Kafaji G, Shah A, Page RA (2007) Biochem Biophys Res Commun 357:237–244
Krompholz N, Krischkowski C, Reichmann D, Garbe-Schönberg D, Mendel R, Bittner F, Clement B, Havemeyer A (2012) Chem Res Toxicol 25:2443–2450
BioGPS (2014) The Scripps Research Institute, La Jolla. http://biogps.org. Accessed 17 June 2014
Mootha VK, Bunkenborg J, Olsen JV, Hjerrild M, Wisniewski JR, Stahl E, Bolouri MS, Ray HN, Sihag S, Kamal M, Patterson N, Lander ES, Mann M (2003) Cell 115:629–640
Da Cruz S, Xenarios I, Langridge J, Vilbois F, Parone PA, Martinou J (2003) J Biol Chem 278:41566–41571
Pagliarini DJ, Calvo SE, Chang B, Sheth SA, Vafai SB, Ong S, Walford GA, Sugiana C, Boneh A, Chen WK, Hill DE, Vidal M, Evans JG, Thorburn DR, Carr SA, Mootha VK (2008) Cell 134:112–123
Neve EPA, Nordling A, Andersson TB, Hellman U, Diczfalusy U, Johansson I, Ingelman-Sundberg M (2012) J Biol Chem 287:6307–6317
Kotthaus J, Wahl B, Havemeyer A, Kotthaus J, Schade D, Garbe-Schönberg D, Mendel R, Bittner F, Clement B (2011) Biochem J 433:383–391
Borgese N, D’Arrigo A, de Silvestris M, Pietrini G (1993) FEBS Lett 325:70–75
D’Arrigo A, Manera E, Longhi R, Borgese N (1993) J Biol Chem 268:2802–2808
Andersson S, Hofmann Y, Nordling A, Li X, Nivelius S, Andersson TB, Ingelman-Sundberg M, Johansson I (2005) Drug Metab Dispos 33:570–578
Clement B, Mau S, Deters S, Havemeyer A (2005) Drug Metab Dispos 33:1740–1747
Islinger M, Lüers GH, Li KW, Loos M, Völkl A (2007) J Biol Chem 282:23055–23069
Wiese S, Gronemeyer T, Ofman R, Kunze M, Grou CP, Almeida JA, Eisenacher M, Stephan C, Hayen H, Schollenberger L, Korosec T, Waterham HR, Schliebs W, Erdmann R, Berger J, Meyer HE, Just W, Azevedo JE, Wanders RJA, Warscheid B (2007) Mol Cell Proteomics 6:2045–2057
Pieuchot L, Jedd G (2012) Annu Rev Microbiol 66:237–263
Van Ael E, Fransen M (2006) Biochim Biophys Acta 1763:1629–1638
Ru Y, Yin L, Sun H, Yin S, Pan Q, Wei H, Wu L, Liu S (2012) Anal Biochem 421:219–226
Gruenewald S, Wahl B, Bittner F, Hungeling H, Kanzow S, Kotthaus J, Schwering U, Mendel RR, Clement B (2008) J Med Chem 51:8173–8177
Jakobs HH, Froriep D, Havemeyer A, Mendel RR, Bittner F, Clement B (2014) ChemMedChem 9:2381–2387
Iyanagi T, Watanabe S, Anan KF (1984) Biochemistry 23:1418–1425
Strittmatter P, Hackett CS, Korza G, Ozols J (1990) J Biol Chem 265:21709–21713
Kimura S, Kawamura M, Iyanagi T (2003) J Biol Chem 278:3580–3589
Slaughter SR, Williams CH, Hultquist DE (1982) Biochim Biophys Acta 705:228–237
Ito A (1980) J Biochem 87:63–71
Borgese N, Gazzoni I, Barberi M, Colombo S, Pedrazzini E (2001) Mol Biol Cell 12:2482–2496
Kurian JR, Bajad SU, Miller JL, Chin NA, Trepanier LA (2004) J Pharmacol Exp Ther 311:1171–1178
Campbell WH (1999) Annu Rev Plant Physiol Plant Mol Biol 50:277–303
Havemeyer A, Grünewald S, Wahl B, Bittner F, Mendel R, Erdélyi P, Fischer J, Clement B (2010) Drug Metab Dispos 38:1917–1921
Froriep D, Clement B, Bittner F, Mendel RR, Reichmann D, Schmalix W, Havemeyer A (2013) Xenobiotica 43:780–784
Fischer K, Barbier GG, Hecht H, Mendel RR, Campbell WH, Schwarz G (2005) Plant Cell 17:1167–1179
Abbenante G, Fairlie DP (2005) Med Chem 1:71–104
Shirk RA, Vlasuk GP (2007) Arterioscler Thromb Vasc Biol 27:1895–1900
Meyer JE, Brocks C, Graefe H, Mala C, Thäns N, Bürgle M, Rempel A, Rotter N, Wollenberg B, Lang S (2008) Breast Care 3:20–24
Fuller AT (1947) Biochem J 41:403–408
Salom-Roig XJ, Hamzé A, Calas M, Vial HJ (2005) Comb Chem High Throughput Screen 8:49–62
Werbovetz K (2006) Curr Opin Investig Drugs 7:147–157
Soeiro MNC, de Castro SL, de Souza EM, Batista DGJ, Silva CF, Boykin DW (2008) Curr Mol Pharmacol 1:151–161
Weller T, Alig L, Beresini M, Blackburn B, Bunting S, Hadváry P, Müller MH, Knopp D, Levet-Trafit B, Lipari MT, Modi NB, Müller M, Refino CJ, Schmitt M, Schönholzer P, Weiss S, Steiner B (1996) J Med Chem 39:3139–3147
Clement B (2002) Drug Metab Rev 34:565–579
Peterlin-Masic L, Cesar J, Zega A (2006) Curr Pharm Des 12:73–91
Rautio J, Kumpulainen H, Heimbach T, Oliyai R, Oh D, Järvinen T, Savolainen J (2008) Nat Rev Drug Discov 7:255–270
Clement B, Raether W (1985) Arzneimittelforschung 35:1009–1014
Clement B, Immel M, Terlinden R, Wingen FJ (1992) Arch Pharm 325:61–62
Molavi A (1989) Am Fam Physician 40:195–200
Clement B, Jung F (1994) Drug Metab Dispos 22:486–497
Hall JE, Kerrigan JE, Ramachandran K, Bender BC, Stanko JP, Jones SK, Patrick DA, Tidwell RR (1998) Antimicrob Agents Chemother 42:666–674
Patrick DA, Hall JE, Bender BC, McCurdy DR, Wilson WD, Tanious FA, Saha S, Tidwell RR (1999) Eur J Med Chem 34:575–583
Huang TL, Bacchi CJ, Kode NR, Zhang Q, Wang G, Yartlet N, Rattendi D, Londono I, Mazumder L, Vanden Eynde, Jean Jacques, Mayence A, Donkor IO (2007) Int J Antimicrob Agents 30:555–561
Wenzler T, Boykin DW, Ismail MA, Hall JE, Tidwell RR, Brun R (2009) Antimicrob Agents Chemother 53:4185–4192
Squizzato A, Dentali F, Steidl L, Ageno W (2009) Intern Emerg Med 4:479–484
Ansede JH, Voyksner RD, Ismail MA, Boykin DW, Tidwell RR, Hall JE (2005) Xenobiotica 35:211–226
Clement B, Bürenheide A, Rieckert W, Schwarz J (2006) ChemMedChem 1:1260–1267
Rahmathullah SM, Hall JE, Bender BC, McCurdy DR, Tidwell RR, Boykin DW (1999) J Med Chem 42:3994–4000
Gustafsson D, Elg M (2003) Thromb Res 109(Suppl 1):S9–S15
Clement B, Lopian K (2003) Drug Metab Dispos 31:645–651
Keisu M, Andersson TB (2010) Handb Exp Pharmacol 196:407–418
Kenne K, Skanberg I, Glinghammar B, Berson A, Pessayre D, Flinois JP, Beaune P, Edebert I, Pohl CD, Carlsson S, Andersson TB (2008) Toxicol In Vitro 22:730–746
Kindmark A, Jawaid A, Harbron CG, Barratt BJ, Bengtsson OF, Andersson TB, Carlsson S, Cederbrant KE, Gibson NJ, Armstrong M, Lagerström-Fermér ME, Dellsén A, Brown EM, Thornton M, Dukes C, Jenkins SC, Firth MA, Harrod GO, Pinel TH, Billing-Clason SME, Cardon LR, March RE (2008) Pharmacogenomics J 8:186–195
dbSNP: Database for Short Genetic Variations (2014) NCBI, Rockville. http://www.ncbi.nlm.nih.gov/SNP/. Accessed 8 Apr 2014
Ott G, Reichmann D, Boerger C, Cascorbi I, Bittner F, Mendel R, Kunze T, Clement B, Havemeyer A (2014) Drug Metab Dispos 42:718–725
Sparacino-Watkins CE, Tejero J, Sun B, Gauthier MC, Thomas J, Ragireddy V, Merchant BA, Wang J, Azarov I, Basu P, Gladwin MT (2014) J Biol Chem 289:10345–10358
Kozmin SG, Schaaper RM (2007) Mutat Res 619:9–15
Kozmin SG, Wang J, Schaaper RM (2010) J Bacteriol 192:2026–2033
Mikula M, Rubel T, Karczmarski J, Goryca K, Dadlez M, Ostrowski J (2010) Funct Integr Genomics 11:215–224
Cribb AE, Spielberg SP, Griffin GP (1995) Drug Metab Dispos 23:406–414
Lavergne SN, Kurian JR, Bajad SU, Maki JE, Yoder AR, Guzinski MV, Graziano FM, Trepanier LA (2006) Toxicology 222:25–36
Ott G, Plitzko B, Krischkowski C, Reichmann D, Bittner F, Mendel RR, Kunze T, Clement B, Havemeyer A (2014) Chem Res Toxicol 27:1687–1695
Page R, Morris C, Williams J, von Ruhland C, Malik AN (1997) Biochem Biophys Res Commun 232:49–53
Chen X, Li X, Wang P, Liu Y, Zhang Z, Zhao G, Xu H, Zhu J, Qin X, Chen S, Hu L, Kong X, Awadalla P (2010) PLoS One. doi:10.1371/journal.pone.0012185
Newton BW, Cologna SM, Moya C, Russell DH, Russell WK, Jayaraman A (2011) J Proteome Res 10:4692–4702
Teslovich TM, Musunuru K, Smith AV, Edmondson AC, Stylianou IM et al (2010) Nature 466:707–713
Aslibekyan S, Goodarzi MO, Frazier-Wood AC, Yan X, Irvin MR, Kim E, Tiwari HK, Guo X, Straka RJ, Taylor KD, Tsai MY, Hopkins PN, Korenman SG, Borecki IB, Chen Y-DI, Ordovas JM, Rotter JI, Arnett DK, Grant SFA (2012) PLoS One. doi:10.1371/journal.pone.0048663
Jakobs HH, Mikula M, Havemeyer A, Strzalkowska A, Borowa-Chmielak M, Dzwonek A, Gajewska M, Hennig EE, Ostrowski J, Clement B (2014) PLoS One. doi:10.1371/journal.pone.0105371
Uhl GR, Drgon T, Liu QR, Johnson C, Walther D, Komiyama T, Harano M, Sekine Y, Inada T, Ozaki N, Iyo M, Iwata N, Yamada M, Sora I, Chen CK, Liu HC, Ujike H, Lin SK (2008) Arch Gen Psychiatry 65:345–355
Aberg K, Adkins DE, Bukszar J, Webb BT, Caroff SN, del Miller D, Sebat J, Stroup S, Fanous AH, Vladimirov VI, McClay JL, Lieberman JA, Sullivan PF, van den Oord EJ (2010) Biol Psychiatry 67:279–282
Mouse Genome Database (MGD) Project (2014) The Jackson Laboratory. http://www.informatics.jax.org/allele/MGI:4435988. Accessed 22 May 2014
Macaya A, Brunso L, Fernández-Castillo N, Arranz JA, Ginjaar HB, Cuenca-León E, Corominas R, Roig M, Cormand B (2005) Neuropediatrics 36:389–394
Shaffer LG, Theisen A, Bejjani BA, Ballif BC, Aylsworth AS, Lim C, McDonald M, Ellison JW, Kostiner D, Saitta S, Shaikh T (2007) Genet Med. 9:607–616
Filges I, Röthlisberger B, Boesch N, Weber P, Wenzel F, Huber AR, Heinimann K, Miny P (2010) Am J Med Genet 152:987–993
Rosenfeld JA, Lacassie Y, El-Khechen D, Escobar LF, Reggin J, Heuer C, Chen E, Jenkins LS, Collins AT, Zinner S, Babcock M, Morrow B, Schultz RA, Torchia BS, Ballif BC, Tsuchiya KD, Shaffer LG (2011) Eur J Med Genet 54:42–49
Mendel RR (2013) J Biol Chem 288:13165–13172
Schwarz G, Belaidi AA (2013) Met Ions Life Sci 13:415–450
Yogev O, Pines O (2010) Biochim Biophys Acta 1808:1012–1020
Acknowledgments
We are very grateful to Dr. Florian Bittner for critical reviewing of this article and thank Dr. Markus Islinger for discussing peroxisomal localization of mARC. Financial support by the Deutsche Forschungsgemeinschaft [DFG, Cl 56/9-1, DFG, ME 1266/24-1] is greatly appreciated.
Conflict of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Author information
Authors and Affiliations
Corresponding author
Additional information
Responsible Editors: José Moura and Paul Bernhardt.
Rights and permissions
About this article
Cite this article
Ott, G., Havemeyer, A. & Clement, B. The mammalian molybdenum enzymes of mARC. J Biol Inorg Chem 20, 265–275 (2015). https://doi.org/10.1007/s00775-014-1216-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00775-014-1216-4