Abstract
Treatment strategies of medication-related osteonecrosis of the jaw (MRONJ) are controversial. Recently, surgical treatment has been reported as superior to nonsurgical treatment, but the contribution discontinued antiresorptive agent use during MRONJ treatment remains unclear. This study aimed to evaluate the efficacy of drug holidays and treatment strategies in MRONJ cases. Four-hundred and twenty-seven patients with MRONJ treated at nine hospitals from 2009 to 2017 were included in this multicenter retrospective study. Multivariate Cox regression analysis showed that the primary disease (osteoporosis or malignant tumor), diabetes, serum albumin, and treatment method (surgical or nonsurgical) were significantly correlated with the cure rate. The cumulative 1-year cure rates in the surgical and nonsurgical treatment groups were 64.7% and 18.2%, respectively. However, discontinuing antiresorptive agents did not influence the treatment outcome in the cohort overall, or in 230 patients after performing propensity score matching among the discontinuation and continuation groups. When stratifying by treatment method, antiresorptive agent discontinuation significantly increased the cure rate in patients with osteoporosis who underwent nonsurgical treatment. In patients with malignant tumors undergoing nonsurgical therapy, discontinuing the antiresorptive agent was associated with a better treatment outcome, but not with statistical significance. In contrast, drug holidays showed no effect on improving outcomes in patients with both osteoporosis and malignant tumors who underwent surgical therapy. Thus, regardless of the primary disease, discontinuing antiresorptive agents during treatment for MRONJ may not be necessary and may be helpful in some cases. Future prospective trials should examine this question further.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
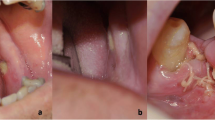
Medication-related osteonecrosis of the jaws (MRONJ) is a well-known adverse effect of antiresorptive agents, such as bisphosphonate (BP) and denosumab (Dmab). Whether to use nonsurgical treatment or surgery as a strategy for treating MRONJ is still controversial, since there have been no randomized controlled trials for treatment methods. The position paper of the American Association of Oral and Maxillofacial Surgeons (AAOMS) [1] and that of the Allied Task Force Committee of the Japanese Society for Bone and Mineral Research on bisphosphonate-related osteonecrosis of the jaw [2] recommended conservative therapy for stages 1–2 of MRONJ. On the other hand, some reviews [3,4,5] have reported that surgical treatment is more effective than nonsurgical treatment for MRONJ. We have also previously reported that extensive surgery was superior to conservative surgery or nonsurgical therapy in a multicenter retrospective study of 361 patients with MRONJ [6]. Additionally, not only the final cure rate, but also the time-to-cure is important, considering that many patients with MRONJ are elderly or have cancer.
Another unresolved issue is whether discontinuing antiresorptive agent treatment affects MRONJ treatment outcomes. Magopoulos et al. [7] reported that patients who underwent surgery after ceasing antiresorptive agent treatment for more than 6 months obtained better treatment outcomes than those who did not take a 6-months drug holiday. The Japanese position paper of 2016 [8] also recommended discontinuing BP or Dmab upon the diagnosis of MRONJ through the end of the MRONJ treatment, although supporting evidence for this approach is lacking. The position paper of AAOMS [1] also discusses drug holidays during invasive dental treatments in patients with osteoporosis, but drug holidays during treatment after an MRONJ diagnosis are not mentioned. In patients with malignant tumors, it is stated that Dmab may theoretically have an effect similar to a drug holiday, but there are no data to support it.
In view of the lack of evidence for the efficacy of a drug holiday, we considered that it may be inappropriate to discontinue BP or Dmab. The purposes of this large-scale, multicenter, retrospective cohort study were (1) to clarify which treatment is best, taking into consideration the treatment duration, and (2) to investigate whether a drug holiday contributes to improved MRONJ treatment outcomes.
Materials and methods
Patients
In total, 453 patients with MRONJ were treated at 9 university hospitals (Nagasaki University, Wakayama Medical University, Kobe University, Kansai Medical University, Nara Medical University, Nagoya City University, Osaka City University, Juntendo University, and Shinshu University) between 2009 and August 2017. Twenty-six patients who were not followed up for more than 3 months after treatment were excluded from the study and the remaining 427 patients were investigated in this retrospective, multicenter study (Fig. 1).
Variables
Various clinical factors were examined retrospectively based on the patients’ medical records including age; sex; site of MRONJ (upper or lower jaw); stage of MRONJ [1]; MRONJ triggering event (tooth extraction or other); type of antiresorptive agent used (BP or Dmab); primary disease (osteoporosis or malignant tumor); duration of antiresorptive agent administration; discontinuation of antiresorptive agent for more than 90 days before MRONJ treatment; use of steroids; diabetes; levels of leukocytes, serum albumin, creatinine; and treatment method (surgical or nonsurgical). Patients who initially underwent nonsurgical treatment but later had surgery, as they were not cured, were also included in the surgical treatment group. Nonsurgical treatment included the use of an antiseptic mouth rinse, a systemic antimicrobial agent, or the removal of the sequester separated from the surface of the exposed bone without anesthesia or with local anesthesia, while the removal of deep sequesters under general anesthesia was considered surgical treatment.
Statistical analysis
All statistical analyses were performed using SPSS software (version 24.0; Japan IBM Co., Tokyo, Japan). First, the relationships between all independent variables and treatment outcomes in all 427 patients were analyzed by the Kaplan–Meier method and log rank test, followed by multivariate Cox proportional hazard model analyses. Next, the efficacy of discontinuing the antiresorptive agent was analyzed by the Kaplan–Meier method and the log rank test in all 427 patients. This analysis was also performed according to the primary disease (osteoporosis or malignancy) and by the treatment method used (surgical or nonsurgical).
Furthermore, a propensity score analysis [9] was performed to minimize selection biases, commonly associated with retrospective data analyses, between the discontinuation and continuation of the antiresorptive agent groups. For each patient, a propensity score for the drug holiday was calculated by a logistic regression analysis of all independent variables. In the propensity score-matched cases, the complete healing rate according to the drug holiday designation was then evaluated by Kaplan–Meier analysis and log rank testing. In all analyses, two-tailed p values < 0.05 were considered statistically significant.
Ethics
Ethical approval from the institutional review board of each University Hospital was obtained and the study conformed to the tenets of the Declaration of Helsinki.
Results
Demographic characteristics of the patients
Patient characteristics in the surgical and nonsurgical treatment groups are summarized in Table 1. Overall, 143 patients were male and 284 were female, with a median age of 75 years. The primary disease was osteoporosis in 191 patients and malignant tumor in 236 patients. In total, 320 patients received BP and 107 received Dmab. Surgical treatment was performed in 191 patients and nonsurgical treatment was given to 236 patients. The treatment method was not randomly distributed but was determined according to the standards of the individual hospitals.
Treatment methods and outcomes
The cumulative healing rates for MRONJ after 1 and 2 years were 64.7% and 81.3%, respectively; the rate was significantly higher in the surgical treatment group than the nonsurgical group (18.2% and 32.0%, respectively; Fig. 2). When assessed according to the primary disease, the surgical group showed significantly better treatment outcomes than the nonsurgical group, for both patients with osteoporosis and those with malignant tumors (Fig. 3).
The relationship between MRONJ cure rates between nonsurgical and surgical treatment strategies subcategorized according to the primary disease. a The healing rate in the nonsurgical and surgical treatment groups in 236 patients with malignant tumors. b The healing rate in the nonsurgical and surgical treatment groups in 191 patients with osteoporosis. MRONJ medication-related osteonecrosis of the jaw
Factors affecting treatment outcome
Multivariate Cox regression analysis revealed that four variables—primary disease, diabetes, serum albumin, and treatment method—were significantly correlated with the healing rate in the 427 patients overall (Table 2).
Relationship between a drug holiday and the treatment outcome
Figure 4 illustrates the cumulative healing rate in the 427 patients with discontinued or continued antiresorptive agent use; there was no significant difference between these two groups. Given the possibility of bias between the discontinuation and continuation groups, we performed propensity score matching analyses. The concordance index was 0.701 and the Hosmer–Lemeshow statistic was insignificant (p = 0.183). The propensity scores—which reflected the probability that a patient would have a drug holiday—ranged from 0.22218 to 0.88793 in the drug holiday group and from 0.13287 to 0.90877 in the no drug holiday group. Propensity score matching yielded 230 patients (115 patients in each group) (Tables 3 and 4). Univariate analysis of the propensity score-matched groups also revealed no significant difference between the outcomes of the two groups (p = 0.346; Fig. 5).
Furthermore, we investigated the efficacy of a drug holiday after cohort stratification according to the primary disease and the treatment method used. In the 236 patients with malignant tumors, discontinuing the antiresorptive agent was associated with better treatment outcomes when nonsurgical therapy was performed, although not significantly so. In contrast, drug holidays showed no effect on improving outcomes in patients who underwent surgical treatment (Fig. 6a, b). In the 191 patients with osteoporosis, those who underwent nonsurgical treatment while discontinuing antiresorptive agent use showed a significantly better outcome than those who underwent nonsurgical treatment without a drug holiday (Fig. 6c). In contrast, in those with osteoporosis who underwent surgery while discontinuing antiresorptive agent use, the time-to-cure was significantly longer than for those who did not take a drug holiday, although the final healing rate did not differ between the two groups (Fig. 6d).
The relationship between antiresorptive agent use, the treatment method, and cure rates. a The MRONJ cure rates in the antiresorptive agent discontinuation and continuation groups in 152 patients with malignant tumors after nonsurgical treatment. b The MRONJ cure rates in the antiresorptive agent discontinuation and continuation treatment groups in 84 patients with malignant tumors after surgical treatment. c The MRONJ cure rates in the antiresorptive agent discontinuation and continuation groups in 84 patients with osteoporosis after nonsurgical treatment. d The MRONJ cure rates in the antiresorptive agent discontinuation and continuation groups in 107 patients with osteoporosis after surgical treatment. MRONJ, medication-related osteonecrosis of the jaw
Discussion
Opinions about the treatment strategy for MRONJ vary, but recently many authors have reported the superiority of surgery over conservative therapy [3,4,5,6]. Conservative therapy not only has a low cure rate, but also a very long time-to-cure, which may decrease the quality of life of the patients, although conservative therapy has some advantages in that it is less invasive. However, few studies have investigated the period required for healing in MRONJ patients. In the current study, we examined treatment outcomes for the time-to-cure using Cox regression analysis rather than performing a logistic regression analysis of the final cure rate. We found that the 1-year cumulative cure rate was 64.7% for surgical therapy and 18.2% for conservative therapy, which indicates that surgery is superior to nonsurgical therapy both in terms of a higher cure rate and a shorter healing duration.
Another unresolved issue had been whether discontinuing antiresorptive agent use during MRONJ therapy was effective for improving the treatment outcome. Martins et al. [8] reported that taking a drug holiday for a longer time contributed to a shorter treatment period, based on a retrospective cohort study of 77 patients; however, they did not compare the drug holiday group with a group that did not discontinue medication. Kim et al. [10] reported that cessation of antiresorptive agent use was not related to treatment outcomes in patients receiving nonsurgical treatment, but it was a significant factor for healing in the group receiving surgical treatment. Hinson et al. [11] and Magopoulos et al. [7] also described some advantages of discontinuing antiresorptive agent treatment to achieve a better MRONJ treatment outcome. However, these reports were on retrospective studies involving a small number of patients, and it remained controversial whether antiresorptive agent use should be discontinued during MRONJ treatment, considering the risks associated with such a drug holiday. It was unclear about the influence of discontinuing antiresorptive agent on the primary disease. That is because even if fractures and bone pain appear, it is difficult to determine whether it is due to drug withdrawal or progression of the primary disease. However, we think that it cannot be ruled out that drug withdrawal may cause some physiological changes such as changes in bone metabolic markers and changes in bone density. In the current study, discontinuing antiresorptive agents showed no significant effects on increasing the cure rate in 427 MRONJ patients.
The effectiveness of antiresorptive agents in patients with malignant tumors and osteoporosis is well known, and the evidence is sound. BP and Dmab play important roles not only in preventing skeletal-related events [12,13,14,15], but also in controlling bone metastasis in patients with malignant tumors [16, 17]. The use of BP/Dmab in the treatment of osteoporosis decreases the fracture rate and affects survival [18,19,20,21,22,23]. On the other hand, there is no evidence that discontinuing antiresorptive agent use improves the outcome of treatment for MRONJ, except in patients with osteoporosis who underwent nonsurgical treatment.
In the present study, we investigated a large number of MRONJ patients in a multicenter study. In a total of 427 cases, a drug holiday did not increase the cure rate based on multivariate Cox regression or on propensity score-matching analysis. Our results revealed BP deposits in the bone long after the blood concentration decreases [24]. In contrast, Dmab has no binding affinity for bone matrices and, unlike BP, the antiresorptive effects of Dmab should mostly dissipate within 6 months of drug discontinuation [1]. Therefore, we examined the effects of drug holidays separately for the BP group and Dmab group, but no effects were observed in either group. We think that the drug holiday had no effect because the holiday period was too short to reduce the antiresorptive effects of BP and Dmab.
Furthermore, we examined the effect of discontinuing antiresorptive agent treatment according to the primary disease (osteoporosis and malignant tumor) and the treatment strategy (nonsurgical and surgical). In patients with malignant tumors undergoing surgery, a drug holiday did not affect the treatment outcome; those with malignant tumors who underwent nonsurgical treatment showed a slight effect due to a drug holiday, but it was not significant. In osteoporosis patients, a drug holiday improved the outcome for nonsurgical treatment methods, although the outcome was still considerably inferior to that achieved by surgery. Conversely, treatment outcomes were poorer in those who underwent surgery while discontinuing antiresorptive agent treatment than in those without such a drug holiday, yet the final cure rate was almost equal for those receiving surgical treatment while continuing or discontinuing antiresorptive agent treatment. The reason for this may be that surgery tended to be delayed in the discontinuation group.
This study suggests that discontinuing antiresorptive agent use while undergoing MRONJ treatment does not improve outcomes, with the exception of osteoporosis patients who received nonsurgical therapy; in these cases, a drug holiday may increase the cure rate. However, since nonsurgical treatment generally takes a long time, the drug holiday period is long and, consequently, the risk of a drug holiday needs to be prudently considered. Since the cure rate is clearly higher in surgical treatment cases than in nonsurgical treatment cases, we propose that it is better to perform surgery without discontinuing antiresorptive agent use than to take the risks associated with long-term drug holidays.
This study had some limitations, since it is a retrospective cohort study and selection bias exists because the treatment policies and surgery methods do not always match in each facility. Therefore, it cannot prove causation, and generalization of the results may be difficult. However, the significance of a drug holiday had not been reported previously in a study of a large number of MRONJ patients. We think that prospective studies are necessary in the future to draw more clear conclusions.
Conclusion
Our research suggests that regardless of the primary disease, discontinuing antiresorptive agents when performing surgical treatment for MRONJ is unnecessary. Also, surgical treatment should be considered as the first method of treatment for MRONJ. Further prospective trials are necessary to substantiate these retrospective findings.
References
Ruggiero SL, Dodson TB, Fantasia J, Goodday R, Aghaloo T, Mehrotra B, O’Ryan F (2014) American association of oral and maxillofacial surgeons position paper on medication-related osteonecrosis of the jaw–2014 update. J Oral Maxillofac Surg 72:1938–1956
Yoneda T, Hagino H, Sugimoto T, Ohta H, Takahashi S, Soen S, Taguchi A, Toyosawa S, Nagata T, Urade M (2010) Bisphosphonate-related osteonecrosis of the jaw: position paper from the Allied Task Force Committee of Japanese Society for Bone and Mineral Research, Japan Osteoporosis Society, Japanese Society of Periodontology, Japanese Society for Oral and Maxillofacial Radiology and Japanese Society of Oral and Maxillofacial Surgeons. J Bone Miner Metab 28:365–383
Rupel K, Ottaviani G, Gobbo M, Contardo L, Tirelli G, Vescovi P, Di Lenarda R, Biasotto M (2014) A systematic review of therapeutical approaches in bisphosphonates-related osteonecrosis of the jaw (BRONJ). Oral Oncol 50:1049–1057
Fliefel R, Tröltzsch M, Kühnisch J, Ehrenfeld M, Otto S (2015) Treatment strategies and outcome of bisphosphonate-related osteonecrosis of the jaw (BRONJ) with characterization of patients: a systematic review. Int J Oral Maxillofac Surg 44:568–585
Khan AA, Morrison A, Hanley DA, Felsenberg D, McCauley LK, O’Ryan F, Reid IR, Ruggiero SL, Taguchi A, Tetradis S, Watts NB (2015) Diagnosis and management of osteonecrosis of the jaw: a systematic review and international consensus. J Bone Miner Res 30:3–23
Hayashida S, Soutome S, Yanamoto S, Fujita S, Hasegawa T, Komori T, Kojima Y, Miyamoto H, Shibuya Y, Ueda N, Kirita T (2017) Evaluation of the treatment strategies for medication-related osteonecrosis of the jaws (MRONJ) and the factors affecting treatment outcome: a multicenter retrospective study with propensity score matching analysis. J Bone Miner Res 32:2022–2029
Magopoulos C, Karakinaris G, Telioudis Z, Vahtsevanos K, Dimitrakopoulos I, Antoniadis K, Delaroudis S (2007) Osteonecrosis of the jaws due to bisphosphonate use. A review of 60 cases and treatment proposals. Am J Otolaryngol 28:158–163
Martins AS, Correia JA, Salvado F, Caldas C, Santos N, Capelo A, Palmela P (2017) Relevant factors for treatment outcome and time to healing in medication-related osteonecrosis of the jaws—A retrospective cohort study. J Craniomaxillofac Surg 45:1736–1742
Rosenbaum PR, Rubin DB (1983) The central role of the propensity score in observational studies for causal effects. Biometrika 70:41–55
Kim YH, Lee HK, Song SI, Lee JK (2014) Drug holiday as a prognostic factor of medication-related osteonecrosis of the jaw. J Korean Assoc Oral Maxillofac Surg 40:206–210
Hinson AM, Siegel ER, Stack BC (2015) Temporal correlation between bisphosphonate termination and symptom resolution in osteonecrosis of the jaw: a pooled case report analysis. J Oral Maxillofac Surg 73:53–62
Rosen LS, Gordon D, Tchekmedyian S, Yanagihara R, Hirsh V, Krzakowski M, Pawlicki M, de Souza P, Zheng M, Urbanowitz G, Reitsma D (2003) Zoledronic acid versus placebo in the treatment of skeletal metastases in patients with lung cancer and other solid tumors: a phase III, double-blind, randomized trial-the Zoledronic Acid Lung Cancer and Other Solid Tumors Study Group. J Clin Oncol 21:3150–3157
Gnant M, Pfeiler G, Dubsky PC, Hubalek M, Greil R, Jakesz R, Wette V, Balic M, Haslbauer F, Melbinger E, Bjelic-Radisic V (2015) Ajuvant denosumab in breast cancer (ABCSG-18): a multicenter, randomized, double-blind, placebo-blind, placebo-controlled trial. Lancet 386:433–443
Smith MR, McGovern FJ, Zietman AL, Fallon MA, Hayden DL, Schoenfeld DA, Kantoff PW, Finkelstein JS (2001) Pamidronate to prevent bone loss during androgen-deprivantion therapy for prostate cancer. N Engl J Med 345:948–955
Smith MR, Egerdie B, Hernandez Toriz N, Feldman R, Tammela TL, Saad F, Heracek J, Szwedowski M, Ke C, Kupic A, Leder BZ (2009) Denosumab in men receiving androgen-deprivation therapy for prostate cancer. N Engl J Med 361:745–755
Early Breast Cancer Trialists’ Collaborative Group (2015) Adjuvant bisphosphonate treatment in early breast cancer: meta-analyses of individual patient data from randomized trials. Lancet 386:1353–1361
Morgan GJ, Davies FE, Gregory WM, Cocks K, Bell SE, Szubert AJ, Navarro-Coy N, Drayson MT, Owen RG, Feyler S, Ashcroft AJ (2010) First-line treatment with zoledronic acid as compared with clodronic acid in multiple myeloma (MRC Myeloma IX): a randomized controlled trial. Lancet 376:1989–1999
Mandema JW, Zheng J, Zheng J, Libanati C, Perez Ruixo JJ (2014) Time course of bone mineral density changes with denosumab compared with other drugs in postmenopausal osteoporosis: a dose-response based meta-analysis. J Clin Endocrinol Metab 99:3746–3755
Yang XC, Deng ZH, Wen T, Luo W, Xiao WF, Zhao RB, Li YS (2016) Network meta-analysis of pharmacological agents for osteoporosis treatment and fracture prevention. Cell Physiol Biochem 40:781–795
Wolfe F, Bolster MB, O’Connor CM, Michaud K, Lyles KW, Colõn-Emeric CS (2013) Bisphosphonate use is associated with reduced risk of myocardial infarction in patients with rheumatoid arthritis. J Bone Miner Res 28:984–991
Lyles KW, Colón-Emeric CS, Magaziner JS, Adachi JD, Pieper CF, Mautalen C, Hyldstrup L, Recknor C, Nordsletten L, Moore KA, Lavecchia C (2007) Zoledronic acid in reducing clinical fracture and mortality after hip fracture. N Eng J Med 357:1799–1809
Center JR, Bliuc D, Nguyen ND, Nguyen TV, Eisman JA (2011) Osteoporosis medication and reduced mortality risk in elderly women and men. J Clin Endocrinol Metab 96:1006–1014
Sambrook PN, Cameron ID, Chen JS, March LM, Simpson JM, Cumming RG, Seibel MJ (2011) Oral bisphosphonates are associated with reduced mortality in frail older people: a prospective five-year study. Osteoporos Int 22:2551–2556
Fleisch HA (1997) Bisphosphonates: preclinical aspects and use in osteoporosis. Ann Med 29:55–62
Acknowledgements
We thank Editage (www.editage.jp) for their English language editing services.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest.
Ethical approval
Ethical approval statement of Institutional Review Board of Nagasaki University Hospital was obtained and committee's reference number was No. 16020827-2.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Hayashida, S., Yanamoto, S., Fujita, S. et al. Drug holiday clinical relevance verification for antiresorptive agents in medication-related osteonecrosis cases of the jaw. J Bone Miner Metab 38, 126–134 (2020). https://doi.org/10.1007/s00774-019-01035-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-019-01035-7