Abstract
Despite the presence of vitamin D receptor (VDR) in skeletal muscle cells, the relationship between VDR expressions and muscle mass or function has not been well studied. The purpose of this study was to compare VDR gene and protein expression in the forearm muscle between sarcopenic and non-sarcopenic individuals who have sustained distal radius fractures. Twenty samples of muscle tissue from sarcopenic patients (mean age 63.4 ± 8.1 years) and 20 age- and sex-matched control tissues (62.1 ± 7.9 years) were acquired from the edge of dissected pronator quadratus muscle during surgery for distal radius fractures. The mRNA expression levels of VDR as well as the myokines of interest that may be associated with muscle mass change (myogenin and myostatin) were analyzed with real-time quantitative reverse transcription polymerase chain reaction (qRT-PCR). In addition, Western blot assay and immunohistochemistry for VDR were performed. Sarcopenic patients showed a significantly lower level of gene expression for VDR and myogenin, but a greater level of gene expression for myostatin than the controls according to qRT-PCR analysis. The density of VDR protein expressions was 2.1 times greater, while that of myostatin was 2.6 times lower, in the control group than in the sarcopenic group according to Western blot analysis. On immunohistochemical analysis, the density of the cells expressing VDR was significantly decreased in the sarcopenic patients. Sarcopenic patients who sustained distal radius fractures presented lower vitamin D receptor gene and protein expression in skeletal muscles compared to non-sarcopenic individuals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Aging is associated with a progressive decline of muscle mass, muscle quality, and muscle strength, which is a condition known as sarcopenia [1]. The decline in total muscle mass between the ages of 40 and 80 has been estimated to range from 30 to 60% [2, 3]. Although sarcopenia denotes loss of muscle mass clinically, it is often used to describe both a set of cellular processes (including hormonal changes, inflammation, and mitochondrial dysfunction) and a set of outcomes such as decreased muscle strength, mobility, and a greater risk of falls [4, 5]. Sarcopenia reportedly occurs in up to 40% of patients sustaining fragility fractures [6, 7]. Among these fractures, distal radius fracture (DRF) is the most common upper-extremity fracture in older people, the incidence of which appears to have increased in recent decades [8, 9]. Patients with DRF have a higher incidence of underlying osteoporosis [10], a low serum vitamin D [11], and a high prevalence of sarcopenia [12]. The occurrence of DRF can reflect early change of bone and muscle fragility because it typically occurs earlier than hip fracture by about 15 years [13].
Some observational studies have demonstrated an association between vitamin D level and muscle strength/physical performance in older adults [14, 15]. The muscle strength and performance of individuals with a low vitamin D status improve with vitamin D supplements. Recent studies show the presence of vitamin D receptor (VDR) in skeletal muscle cells, showing contradictory effects of serum vitamin D on the expression of intramuscular VDR [16,17,18,19,20]. VDR is a member of the nuclear receptor superfamily that regulates the expression of many genes, while the vitamin D-VDR complex exerts non-genomic effects on intracellular signaling and calcium influx [21]. Despite the possible association between VDR expression and muscle mass change, the change of VDR gene or protein expressions in sarcopenic patients has not been well studied. The purpose of this study was to compare VDR gene and protein expression in the muscle between sarcopenic and non-sarcopenic individuals who sustained distal radius fractures.
Materials and methods
Subjects
This study was approved by our institutional review board, and all patients provided informed consent. We prospectively recruited 85 patients with DRF who were treated surgically at our institution from March 2017 to April 2018. These patients were recruited from a tertiary care university hospital serving as a regional emergency trauma center. Inclusion criteria were acute DRF treated within 2 weeks after injury caused by minor trauma such as a fall on an outstretched hand, older than 50 years of age, and those who agreed to participate in the study. Patients were excluded if they had associated systemic or multiorgan injuries, cognitive impairment, or medical conditions such as neuromuscular disease of chronic debilitating disease that might affect muscle strength (renal insufficiency, adrenal insufficiency, rheumatoid arthritis, thyroid disease, parathyroid disease or Parkinson disease). Among the 76 patients without these conditions, we identified 20 DRF patients with sarcopenia who were matched for age and gender with 20 controls without sarcopenia.
The definition of sarcopenia was based on the proposal from the Asian Working Group for Sarcopenia (AWGS) [22]. Participants were classified as sarcopenic if they had low lean mass plus slowness (classified according to gait speed) or weakness (assessed according to grip strength). Low lean mass was defined by adjusting the appendicular lean mass (the sum of muscle mass in arms and legs) by the height (ASM/Ht2, kg/m2). AWGS [22] suggested the cut-off points of ASM/Ht2 for people of Asian origin to be 7.0 kg/m2 in men and 5.4 kg/m2 in women. Walking speed was calculated as the average of two usual-walking pace attempts over 6 m and expressed as m/s. Slowness was defined as a gait speed slower than 0.8 m/s [22]. The grip strength of the unaffected hand was measured with a Jamar dynamometer (Asimow Engineering, Los Angeles, CA, USA) with the elbow flexed at 90° and the forearm in a neutral rotation. The mean values of three trials were recorded in kilograms. Weak hand grip strength is suggested to be defined as < 26 kg for men and < 18 kg for women [22].
Tissue acquisition
A single surgeon performed the standard open reduction and internal fixation of DRF using a volar approach. A small part of the pronator quadratus muscle (1 cm3) was collected from the surgical field during the operations. Muscles comprise different proportions of slow twitch and fast twitch fibers, and fast twitch fibers are known to be predominantly lost in sarcopenia [23]. Although there is no biopsy study examining fiber-type proportions of the forearm rotation muscles, the endurance data suggest that the prime supination torque muscle comprises greater proportions of slow twitch fibers, while the pronation muscles are faster fatiguing and may comprise a greater proportion of fast twitch fibers [24]. Two tissue samples were acquired using a Metzenbaum scissor from the edge of the dissected pronator quadratus muscle. One sample was frozen immediately at − 80 °C for the polymerase chain reaction (PCR) analysis and later Western blot analysis. Another sample was fixed in fresh 10% buffered formalin for 16–24 h at 4 °C and then subsequently dehydrated and paraffin embedded for immunohistochemical analysis.
Reverse transcription-quantitative PCR (RT-qPCR) analysis
The mRNA expression levels of VDR and some myokine of interest that may be associated with muscle mass change (myogenin and myostatin) were evaluated using real-time quantitative reverse transcription PCR (qRT-PCR) analyses. The tissue samples from the isolated pronator quadratus muscles were immediately frozen at − 80 °C until RNA extraction. Total RNA was isolated from Trizol extract (Invitrogen, Carlsbad, CA, USA), according to the manufacturer’s instructions, and complementary DNA was synthesized using a Maxime RT PreMix Kit (iNtRON Biotechnology, Seongnam, Korea).
Amplification was performed by real-time qPCR using the Light Cycler 480 System (Roche Diagnostics, Basel, Switzerland) with 2× qPCRBIO SyGreen Mix Lo-ROX (PCR Biosystems, London, UK). Measurements were performed using the Light Cycler quantification software version 1.5 (Roche Diagnostics). The real-time Cycler 480 Multiwell Plate 96 contained 0.5 mM of each primer, 0.25 mM of the probe, 10-mL FastStart Essential DNA Probes Master (Roche Diagnostics), and 2 mL of DNA template, in a final reaction volume of 20 mL. The thermal cycling conditions on the Light-Cycler 480 System were as follows: enzyme activation, 95 °C for 10 min; 45 cycles of amplification, 95 °C for 10 s; and 60 °C for 30 s. Each quantitative real-time PCR analysis was performed in triplicate for both target genes and internal control, and the gene expression levels were reported as the relative ratio to the internal control of the β-actin gene.
Western blot analysis and immunofluorescence microscopy
Western blot analyses were performed for the protein targets, which were VDR, myostatin, and myogenin. Whole cell extracts from the forearm muscle were prepared using radioimmunoprecipitation assay (RIPA) buffer (Elpis-Biotech, Daejeon, Korea). Proteins from the whole cell lysates were separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis on 10% gels and transferred to nitrocellulose membranes. The membranes were separately probed with an anti-VDR (D-6) (sc-13133, Santa Cruz Biotechnology, Dallas, TX, USA), anti-myogenin (5FD) (sc-52903, Santa Cruz Biotechnology), anit-myostatin (ab71808, Abcam, Cambridge, UK), and anti-Glyceraldehyde-3-phosphate dehydrogenase (GAPDH) (sc-47724, Santa Cruz Biotechnology) antibody. Bound antibodies were visualized using an Amersham ECL kit (GE Healthcare, Piscataway, NJ, USA) and an LAS-4000 Image Analyzer (Fujifilm, Tokyo, Japan). The band density was quantified by densitometry with the image analyzer ImageQuant LAS 4000 (GE Healthcare and Fujifilm, Taipei, Taiwan). The protein expression levels were reported as a relative ratio to the internal control of GAPDH.
For immunofluorescence microscopy, 0.5-μm fixed frozen muscle sections were labeled with primary antibody for VDR and the resulting immune complexes were visualized with a goat anti-rabbit IgG H&L (Alexa Fluor 488) (ab150077, Abcam) or goat anti-mouse IgG H&L (Alexa Fluor 594) (ab150116, Abcam) secondary antibody. Nuclei were stained with 4′,6-diamidino-2-phenylindole (VECTASHIELD Hardset Antifade Mounting Medium, H-1500, Vector Laboratories, Inc., Burlingame, CA, USA). Images were acquired with an upright fluorescence microscope (BX61-32FDIC, Olympus, Tokyo, Japan).
Statistical analyses
Power analysis indicated that a sample size consisting of 40 (20 per each group) would provide 80% statistical power with an α of 0.10 for a large effect size (Cohen’s d = 0.8) for the Student’s t test.
Descriptive statistics were calculated to determine patients’ demographics and clinical characteristics. A t test was conducted to determine any significant differences between the two groups in terms of continuous variables, and the chi-square or Fisher exact test was conducted to determine any significant differences in the categorical variables. Statistical significance was considered when the p value was less than 0.05. All statistical analyses were performed using SPSS for Windows (version 18.0, SPSS Inc., Chicago, IL, USA).
Results
Figure 1 shows a flowchart of the patient enrollment from 86 patients who were surgically treated for distal radius fractures at our institute in a study period. The demographic and clinical data of the 2 groups (sarcopenic and control groups) are described in Table 1. Sarcopenic patients had significantly decreased lean body mass index and grip strength compared to the controls, but gait speeds were similar in the 2 groups.
Reverse transcription-quantitative PCR (RT-qPCR) analysis
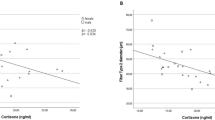
The mRNA expression levels of VDR were more significantly decreased in the sarcopenic group than in the control group (2.3-fold, p = .012). Similarly, the mRNA expression of myogenin was significantly decreased (2.1-fold, p = .017), but that of myostatin was increased (2.4-fold, p = .010) in the sarcopenic group compared to the control group. The target mRNA expression levels relative to the β-actin internal control gene in both groups are shown in Fig. 2.
Western blot and immunofluorescence analysis
The 48/53 kDa band, which corresponds to the VDR showed lower density in the sarcopenic group than in the control group. The mean optical density VDR was 2.1 times greater in the control group than in the sarcopenic group (p = .018). In addition, while the 43 kDa band, which corresponds to the myostatin, showed 2.6 times lower density in the control group (p = .015), the 34KDa band for myogenin did not significantly differ between the sarcopenic and non-sarcopenic groups (Fig. 3).
Relative protein expression levels of VDR, myogenin, and myostatin in forearm muscle between sarcopenic and control patients. The mean optical density VDR (48/53 kDa) was 2.1 times greater in the control group than in the sarcopenic group. While the 43 kDa band, which corresponds to the myostatin, showed higher density, the 34 KDa band for myogenin did not significantly differ between the sarcopenic and control patients, CTL control
The Western blotting results were also verified in the immunohistofluorescence analyses for VDR. The density of cells expressing VDR was clearly decreased in the pronator quadrate muscle of the sarcopenic patients compared with that in the control patients (Fig. 4).
Discussion
Despite the presence of the vitamin D receptor (VDR) in skeletal muscle cells, the relationship between VDR expressions and muscle mass or function has not been well studied. We compared VDR gene and protein expression in the forearm muscle between sarcopenic and non-sarcopenic individuals who sustained distal radius fractures. We found significantly under-expressed VDR in the forearm muscle of sarcopenic patients when compared with the control. Even though over-expression of myostatin and under-expression of myogenin genes were observed in the muscle of sarcopenic patients, only myostatin show increased protein expressions in sarcopenic patients on Western blot analysis.
Age-related muscle loss is a result of reductions in the size and number of muscle fibers, possibly due to a multi-factorial process that involves physical activity, nutritional intake, metabolic homeostasis, oxidative stress, hormonal changes, and lifespan [25, 26]. The specific contribution of each of these factors is unknown, but emerging evidence suggests that the distribution of several positive or negative proteins in muscles is an important feature in the progression of sarcopenia [27,28,29]. However, contradictory results have been observed among various investigators regarding age-related changes in the levels of common regulatory factors [29,30,31].
Myogenic regulator factor (MRF) genes provide myogenic specificity for activated satellite cells [32]. The MRFs include myogenic differentiation 1 protein (MyoD), myogenic factor 5 (Myf5), myogenin (myogenic factor 4), and muscle-specific regulatory factor 4 (Mrf4) [33]. Myogenin, an important regulator for satellite cell (daughter cell) differentiation, is a muscle-specific basic helix–loop–helix (bHLH) transcription factor involved in the coordination of skeletal muscle development or myogenesis and repair [32]. In this study, while qRT-PCR revealed the under-expression of myogenin genes, but no significant differences were observed in the Western blot analysis between the sarcopenic and control patients. These findings are consistent with previous studies, suggesting that aging reduces the ability of muscles to increase myogenin protein levels [34]. The mRNA and protein levels may not always concur with each other due to many post-transcriptional modifications, post-translational modifications, and differential protein degradation (such as proteasome-mediated or autophagy-mediated protein breakdown).
Myostatin (growth and differentiation factor-8, GDF-8), a member of the transforming growth factor-β superfamily of secreted growth and differentiation factors, is a negative regulator of skeletal muscle growth [35]. Muscle is the primary source of myostatin in the body, and myostatin levels are downregulated both locally and in circulating form by physical exercise, which may thus account for some of the resultant muscle hypertrophy [36]. The absence or deficiency of myostatin significantly increases muscle mass in mice, cows, and humans, whereas treatment with myostatin causes muscle wasting [37]. Myostatin levels are elevated with disuse atrophy, cancer, and AIDS-related cachexia [37, 38]. Many researchers have investigated the effect of inhibiting myostatin to counteract sarcopenia in animals and have reported several positive effects of myostatin inhibitor. However, the role of myostatin in driving sarcopenia has been debated as specific force has been shown to reduce in myostatin null mice, although their muscle mass increased twofold [39, 40]. Our study demonstrated the over-expression of myostatin in sarcopenic individuals compared to non-sarcopenic controls. This result corroborates the results from the previous cross-sectional study, which suggested that serum myostatin levels increase with advancing age, are highest in physically frail older women, and are inversely associated with skeletal muscle mass [41].
In this study, sarcopenic patients had a decreased VDR expression compared to that of the controls in both Western blot and immunohistofluorescence. These findings are consistent with previous studies since the VDR expression in human muscle tissue decreases with age [20, 42]. Simpson et al. found that young cultured skeletal myocytes expressed more VDR than old myocytes [42] and Horst et al. found an association of age with diminished expression of the VDR in rat intestines and bone tissues [43]. Several previous studies investigating the effect of VDR expression on muscle mass suggested an incremental effect of VDR on muscle fibers [19, 44]. Mouse studies reported correlations between both vitamin D signaling and VDR expression with grip strength, fiber quality, and myostatin expression [44, 45]. VDR-null mice exhibited a clear muscle phenotype, with a small fiber size and an abnormal expression of all major muscle-specific genes [46]. Conversely, negative association between VDR expression and muscle mass was also reported [47], of which findings seem to be contradictory to our observation. The previous study showing negative association between VDR expression and muscle mass did not evaluate gene expression for VDR, and it was supposed that patients with a low lean mass increased the VDR expression and maximized the use of vitamin D to compensate for reduced muscle mass and strength [47]. This may be associated with non-genomic effects of vitamin D-VDR complex intracellular signaling. Although the reason for this discrepancy is unclear, the present study evaluates both gene and protein expression for VDR and it may reflect genomic mechanism of VDR signaling pathway.
Although the data of this study could not suggest the value of VDR on muscle function, recent studies suggest that vitamin D signaling via VDR plays a role in the regulation of myoblast proliferation and differentiation [48,49,50]. VDR-null mice showed aberrantly increased expression of embryonic and neonatal MyHC (myosin heavy-chain) isoforms but not type II (adult fast twitch) MyHC isoform [46]. Knockdown of VDR inhibits myotube formation concomitantly with downregulation of MyoD and myogenin [49]. These findings demonstrate that a substantial level of signaling via VDR is required for normal muscle development and myogenesis in vitro. Thus, it can be speculated that a decreased VDR expression in skeletal muscle leads lower muscle mass and function in this study. However, the detailed mechanisms of VDR signaling remain to be elucidated and further studies are necessary to determine the precise VDR signal pathway in the progression of sarcopenia.
This study has several limitations that need to be considered. First, the number of patients was relatively small, which may have reduced the statistical power of this study and increased the possibility of reporting false negative results. Second, the VDR evaluation was cross-sectional, so a causal relationship between the VDR and changes in skeletal muscles could not be determined. Further longitudinal studies on changes of VDR expression are necessary. Third, age-related muscle loss is a multi-factorial process that involves physical activity, nutritional intake, metabolic homeostasis, oxidative stress, hormonal changes, and lifespan, and we did not consider these potentially confounding variables in our analysis. The effects of these factors on the expression of VDR have not been determined. For instance, some investigators reported that serum 25-hydroxyvitamin D (25OHD) concentration stimulates intramuscular VDR expression [19], whereas others found that VDR expression in muscle was not associated with serum vitamin D level [20, 47]. In addition, we could not include sufficient cytokines or growth factors relevant to sarcopenia. Instead, we investigated the reference myokines that are of interest. Including more regulatory factors may allow us to detect other factors that may have a relationship with a muscle mass change. Finally, the DRF patients were relatively young to represent the typical characteristics of sarcopenia such as decreased activities of daily living and increased frailty; their characteristics and the study results may therefore differ from those in general populations.
In conclusion, sarcopenic patients had decreased VDR gene and protein expression in their skeletal muscles. We also found the over-expression of myostatin and under-expression of myogenin genes in sarcopenic patients, where only myostatin showed increased protein expressions. The under-expressions of VDR may be one of the signal pathways for the development or progression of sarcopenia. Further studies are necessary to explore the role of VDR in the progression of sarcopenia.
References
Candow DG, Chilibeck PD (2005) Differences in size, strength, and power of upper and lower body muscle groups in young and older men. J Gerontol A Biol Sci Med Sci 60:148–156
Clynes MA, Edwards MH, Buehring B, Dennison EM, Binkley N, Cooper C (2015) Definitions of sarcopenia: associations with previous falls and fracture in a population sample. Calcif Tissue Int 97:445–452
Trombetti A, Reid KF, Hars M, Herrmann FR, Pasha E, Phillips EM, Fielding RA (2016) Age-associated declines in muscle mass, strength, power, and physical performance: impact on fear of falling and quality of life. Osteoporos Int 27:463–471
von Haehling S, Morley JE, Anker SD (2010) An overview of sarcopenia: facts and numbers on prevalence and clinical impact. J Cachexia Sarcopenia Muscle 1:129–133
Melton LJ 3rd, Khosla S, Crowson CS, O’Connor MK, O’Fallon WM, Riggs BL (2000) Epidemiology of sarcopenia. J Am Geriatr Soc 48:625–630
Bokshan SL, DePasse JM, Daniels AH (2016) Sarcopenia in orthopedic surgery. Orthopedics 39:e295–e300
Hong W, Cheng Q, Zhu X, Zhu H, Li H, Zhang X, Zheng S, Du Y, Tang W, Xue S, Ye Z (2015) Prevalence of sarcopenia and its relationship with sites of fragility fractures in elderly Chinese men and women. PLoS ONE 10:e0138102
Nellans KW, Kowalski E, Chung KC (2012) The epidemiology of distal radius fractures. Hand Clin 28:113–125
MacIntyre NJ, Dewan N (2016) Epidemiology of distal radius fractures and factors predicting risk and prognosis. J Hand Ther 29:136–145
Koval KJ, Harrast JJ, Anglen JO, Weinstein JN (2008) Fractures of the distal part of the radius. The evolution of practice over time. Where’s the evidence? J Bone Jt Surg Am 90:1855–1861
Jang WY, Chung MS, Baek GH, Song CH, Cho HE, Gong HS (2012) Vitamin D levels in post-menopausal Korean women with a distal radius fracture. Injury 43:237–241
Roh YH, Koh YD, Noh JH, Gong HS, Baek GH (2017) Evaluation of sarcopenia in patients with distal radius fractures. Arch Osteoporos 12:5
Owen RA, Melton LJ 3rd, Ilstrup DM, Johnson KA, Riggs BL (1982) Colles’ fracture and subsequent hip fracture risk. Clin Orthop Relat Res 37–43
Visser M, Deeg DJH, Lips P (2003) Low vitamin D and high parathyroid hormone levels as determinants of loss of muscle strength and muscle mass (sarcopenia): the Longitudinal Aging Study Amsterdam. J Clin Endocrinol Metab 88:5766–5772
Snijder MB, van Schoor NM, Pluijm SMF, van Dam RM, Visser M, Lips P (2006) Vitamin D status in relation to one-year risk of recurrent falling in older men and women. J Clin Endocrinol Metab 91:2980–2985
Bouillon R, Gielen E, Vanderschueren D (2014) Vitamin D receptor and vitamin D action in muscle. Endocrinology 155:3210–3213
Girgis CM, Mokbel N, Cha KM, Houweling PJ, Abboud M, Fraser DR, Mason RS, Clifton-Bligh RJ, Gunton JE (2014) The vitamin D receptor (VDR) is expressed in skeletal muscle of male mice and modulates 25-hydroxyvitamin D (25OHD) uptake in myofibers. Endocrinology 155:3227–3237
Pike JW (2014) Expression of the vitamin D receptor in skeletal muscle: are we there yet? Endocrinology 155:3214–3218
Pojednic RM, Ceglia L, Olsson K, Gustafsson T, Lichtenstein AH, Dawson-Hughes B, Fielding RA (2015) Effects of 1,25-dihydroxyvitamin D3 and vitamin D3 on the expression of the vitamin d receptor in human skeletal muscle cells. Calcif Tissue Int 96:256–263
Bischoff-Ferrari HA, Borchers M, Gudat F, Durmuller U, Stahelin HB, Dick W (2004) Vitamin D receptor expression in human muscle tissue decreases with age. J Bone Miner Res 19:265–269
Girgis CM, Clifton-Bligh RJ, Hamrick MW, Holick MF, Gunton JE (2013) The roles of vitamin D in skeletal muscle: form, function, and metabolism. Endocr Rev 34:33–83
Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS, Chou MY, Chen LY, Hsu PS, Krairit O, Lee JS (2014) Sarcopenia in Asia: consensus report of the Asian Working Group for sarcopenia. J Am Med Dir Assoc 15:95–101
Walston JD (2012) Sarcopenia in older adults. Curr Opin Rheumatol 24:623–627
O’Sullivan LW, Gallwey TJ (2005) Forearm torque strengths and discomfort profiles in pronation and supination. Ergonomics 48:703–721
Demontis F, Piccirillo R, Goldberg AL, Perrimon N (2013) The influence of skeletal muscle on systemic aging and lifespan. Aging Cell 12:943–949
Roubenoff R, Hughes VA (2000) Sarcopenia current concepts. J Gerontol Ser A 55:M716–M724
Kunihiro S, Akihiko Y (2010) Molecular mechanisms in aging and current strategies to counteract sarcopenia. Curr Aging Sci 3:90–101
Zhou J, Freeman TA, Ahmad F, Shang X, Mangano E, Gao E, Farber J, Wang Y, Ma X-L, Woodgett J, Vagnozzi RJ, Lal H, Force T (2013) GSK-3α is a central regulator of age-related pathologies in mice. J Clin Investig 123:1821–1832
Kunihiro S, Akihiko Y (2012) Sarcopenia and cachexia: the adaptations of negative regulators of skeletal muscle mass. J Cachexia Sarcopenia Muscle 3:77–94
Wohlgemuth SE, Seo AY, Marzetti E, Lees HA, Leeuwenburgh C (2010) Skeletal muscle autophagy and apoptosis during aging: effects of calorie restriction and life-long exercise. Exp Gerontol 45:138–148
McKay BR, Ogborn DI, Bellamy LM, Tarnopolsky MA, Parise G (2012) Myostatin is associated with age-related human muscle stem cell dysfunction. FASEB J 26:2509–2521
Kim JS, Kosek DJ, Petrella JK, Cross JM, Bamman MM (2005) Resting and load-induced levels of myogenic gene transcripts differ between older adults with demonstrable sarcopenia and young men and women. J Appl Physiol (1985) 99:2149–2158
Sakuma K, Aoi W, Yamaguchi A (2014) The intriguing regulators of muscle mass in sarcopenia and muscular dystrophy. Front Aging Neurosci 6:230
Alway SE, Lowe DA, Chen KD (2001) The effects of age and hindlimb suspension on the levels of expression of the myogenic regulatory factors MyoD and myogenin in rat fast and slow skeletal muscles. Exp Physiol 86:509–517
Hamrick MW (2011) A role for myokines in muscle-bone interactions. Exerc Sport Sci Rev 39:43–47
Laurent MR, Dubois V, Claessens F, Verschueren SM, Vanderschueren D, Gielen E, Jardi F (2016) Muscle-bone interactions: from experimental models to the clinic? A critical update. Mol Cell Endocrinol 432:14–36
Lee SJ (2004) Regulation of muscle mass by myostatin. Annu Rev Cell Dev Biol 20:61–86
Elkasrawy MN, Hamrick MW (2010) Myostatin (GDF-8) as a key factor linking muscle mass and bone structure. J Musculoskelet Neuronal Interact 10:56–63
Amthor H, Macharia R, Navarrete R, Schuelke M, Brown SC, Otto A, Voit T, Muntoni F, Vrbova G, Partridge T, Zammit P, Bunger L, Patel K (2007) Lack of myostatin results in excessive muscle growth but impaired force generation. Proc Natl Acad Sci USA 104:1835–1840
Gentry BA, Ferreira JA, Phillips CL, Brown M (2011) Hindlimb skeletal muscle function in myostatin-deficient mice. Muscle Nerve 43:49–57
Yarasheski KE, Bhasin S, Sinha-Hikim I, Pak-Loduca J, Gonzalez-Cadavid NF (2002) Serum myostatin-immunoreactive protein is increased in 60-92 year old women and men with muscle wasting. J Nutr Health Aging 6:343–348
Simpson RU, Thomas GA, Arnold AJ (1985) Identification of 1,25-dihydroxyvitamin D3 receptors and activities in muscle. J Biol Chem 260:8882–8891
Horst RL, Goff JP, Reinhardt TA (1990) Advancing age results in reduction of intestinal and bone 1,25-dihydroxyvitamin D receptor. Endocrinology 126:1053–1057
Girgis CM, Cha KM, Houweling PJ, Rao R, Mokbel N, Lin M, Clifton-Bligh RJ, Gunton JE (2015) Vitamin D receptor ablation and vitamin D deficiency result in reduced grip strength, altered muscle fibers, and increased myostatin in mice. Calcif Tissue Int 97:602–610
Garcia LA, King KK, Ferrini MG, Norris KC, Artaza JN (2011) 1,25(OH)2vitamin D3 stimulates myogenic differentiation by inhibiting cell proliferation and modulating the expression of promyogenic growth factors and myostatin in C2C12 skeletal muscle cells. Endocrinology 152:2976–2986
Endo I, Inoue D, Mitsui T, Umaki Y, Akaike M, Yoshizawa T, Kato S, Matsumoto T (2003) Deletion of vitamin D receptor gene in mice results in abnormal skeletal muscle development with deregulated expression of myoregulatory transcription factors. Endocrinology 144:5138–5144
Kim K, Gong HS, Lim JY, Kim JH, Baek GH (2018) The vitamin D receptor expression in skeletal muscle of women with distal radius fracture. Arch Osteoporos 13:24
Srikuea R, Zhang X, Park-Sarge OK, Esser KA (2012) VDR and CYP27B1 are expressed in C2C12 cells and regenerating skeletal muscle: potential role in suppression of myoblast proliferation. Am J Physiol Cell Physiol 303:C396–C405
Tanaka M, Kishimoto KN, Okuno H, Saito H, Itoi E (2014) Vitamin D receptor gene silencing effects on differentiation of myogenic cell lines. Muscle Nerve 49:700–708
Girgis CM, Clifton-Bligh RJ, Mokbel N, Cheng K, Gunton JE (2014) Vitamin D signaling regulates proliferation, differentiation, and myotube size in C2C12 skeletal muscle cells. Endocrinology 155:347–357
Acknowledgements
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIP) (no. 2017R1C1B1002544).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Roh, Y.H., Hong, S.W., Chung, S.W. et al. Altered gene and protein expressions of vitamin D receptor in skeletal muscle in sarcopenic patients who sustained distal radius fractures. J Bone Miner Metab 37, 920–927 (2019). https://doi.org/10.1007/s00774-019-00995-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-019-00995-0