Abstract
Hypophosphatasia (HPP) is a rare inherited metabolic bone disease due to a deficiency of the tissue nonspecific alkaline phosphatase isoenzyme (TNSALP) encoded by the ALPL gene. Patients have consistently low serum alkaline phosphatase (AP), so that this parameter is a good hallmark of the disease. Adult HPP is heterogeneous, and some patients present only mild nonpathognomonic symptoms which are also common in the general population such as joint pain, osteomalacia and osteopenia, chondrocalcinosis, arthropathy and musculoskeletal pain. Adult HPP may be recessively or dominantly inherited; the latter case is assumed to be due to the dominant negative effect (DNE) of missense mutations derived from the functional homodimeric structure of TNSALP. However, there is no biological argument excluding the possibility of other causes of dominant HPP. Rheumatologists and endocrinologists are increasingly solicited for patients with low AP and nonpathognomonic symptoms of HPP. Many of these patients are heterozygous for an ALPL mutation and a challenging question is to determine if these symptoms, which are also common in the general population, are attributable to their heterozygous ALPL mutation or not. In an attempt to address this question, we reviewed a cohort of 61 adult patients heterozygous for an ALPL mutation. Mutations were distinguished according to their statistical likelihood to show a DNE. One-half of the patients carried mutations predicted with no DNE and were slightly less severely affected by the age of onset, serum AP activity and history of fractures. We hypothesized that these mutations result in another mechanism of dominance or are recessive alleles. To identify other genetic factors that could trigger the disease phenotype in heterozygotes for potential recessive mutations, we examined the next-generation sequencing results of 32 of these patients for a panel of 12 genes involved in the differential diagnosis of HPP or candidate modifier genes of HPP. The heterozygous genotype G/C of the COL1A2 coding SNP rs42524 c.1645C > G (p.Pro549Ala) was associated with the severity of the phenotype in patients carrying mutations with a DNE whereas the homozygous genotype G/G was over-represented in patients carrying mutations without a DNE, suggesting a possible role of this variant in the disease phenotype. These preliminary results support COL1A2 as a modifier gene of HPP and suggest that a significant proportion of adult heterozygotes for ALPL mutations may have unspecific symptoms not attributable to their heterozygosity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypophosphatasia (HPP) is a rare inherited metabolic bone disease due to a deficiency of the tissue nonspecific alkaline phosphatase isoenzyme (TNSALP) encoded by the ALPL gene. Although its clinical spectrum is a continuum, HPP has been divided into six clinical subtypes that may significantly overlap [1]. Perinatal HPP is the most severe form and is almost always lethal, presenting with hypoplastic lungs, extensive hypomineralization, rachitic bone deformities and disturbances of calcium and phosphate metabolism. In contrast, the prenatal benign (PB) form is characterized by prenatal symptoms that spontaneously improve, resulting in non-lethal HPP [2]. Clinical signs of the infantile form appear during the first 6 months of life and include rickets, premature craniosynostosis, irritability, seizures and nephrocalcinosis due to hypercalciuria. This form is lethal in approximately 50% of the cases. Childhood HPP is heterogeneous. It occurs after 6 months of age and is characterized by delayed walking, a waddling gait, and rickets that may cause short stature. Premature loss of primary teeth leads to the diagnosis [3]. Adult HPP is also heterogeneous, with patients presenting recurrent stress fractures and low mineral density during middle age and patients presenting only mild nonpathognomonic symptoms such as joint pain, osteomalacia and osteopenia, chondrocalcinosis, arthropathy and musculoskeletal pain [4,5,6]. Odontohypophosphatasia (odontoHPP) is characterized by dental manifestations of HPP not associated with abnormalities of the skeletal system. Patients with severe or moderate HPP have consistently low serum alkaline phosphatase (AP), so that this parameter is a good hallmark of the disease [7]. A treatment with enzyme replacement therapy has been shown to be efficient [8] and is now available for pediatric-onset HPP.
TNSALP is a central actor of bone mineralization [9]. The enzyme catalyzes the hydrolysis of various phosphomonoesters among which are inorganic pyrophosphate, pyridoxal-5′-phosphate and nucleotides. This catalytic activity depends on a homodimeric configuration from which the dominant negative effect (DNE) of some ALPL mutations likely derive. Five functional domains have been identified in the three-dimensional (3D) structure of TNSALP modeled from the crystal structure of human placental AP [10,11,12]. The active site is the center of catalytic activity. The calcium site is highly conserved in vertebrates, but its function remains to be elucidated. The homodimer interface is crucial because dimerization is indispensable for allostery. The crown domain is a key factor of uncompetitive inhibition, heat stability and allosteric behavior and, together with the N-terminal alpha helix, contributes to stabilization of the dimeric structure. The crown domain has also been shown to bind collagen [13, 14].
Severe forms of HPP (perinatal and infantile) are almost always recessively inherited, while less severe forms (childhood, adult, odonto and PB) may be dominantly or recessively inherited [15,16,17]. The more severe the disease, the more often it is subject to recessive inheritance [15, 18]. Both dominant and recessive forms are due to loss-of-function mutations in the ALPL gene.
The prevalence of severe HPP was estimated at 1/100 000 in Canada based on pediatric registries [19], and more recently at 1/300 000 in Europe based on molecular diagnosis [20]. This corresponds to carrier frequencies of 1:160 and 1:270, respectively. Because heterozygotes can express the disease, mild HPP is expected to be more frequent, with its actual frequency depending on the proportion of dominant mutations and their penetrance [20]. The actual proportion of persons with repeatedly low AP in the population is unknown. According to recent reports it might range from 1/1544 [21] to 1/81 [22], and 50−84% of them could harbor pathogenic ALPL mutations [23, 24]. Even with a low penetrance, these mutations may account for the high incidence of mild forms of HPP. However, symptoms such as musculoskeletal pain, dental problems such as carries, osteomalacia and osteopenia or symptoms resembling osteoporosis are very common in the general adult population including heterozygotes for a recessive ALPL mutation. More simply, low serum AP levels indicate an ALPL mutation [21, 23, 25, 26], but an ALPL mutation does not necessarily indicate HPP. Rheumatologists and endocrinologists are increasingly solicited for patients with low AP and nonpathognomonic symptoms of HPP. Many of these patients are heterozygous for an ALPL mutation and a challenging question is to determine if these symptoms, which are also common in the general population, are attributable to their heterozygous ALPL mutation or not.
In the attempt to address this question, we studied a cohort of 61 adult patients heterozygous for an ALPL mutation. To distinguish heterozygotes for dominant and recessive mutations, respectively, we classified the ALPL mutations according to their statistical likelihood to show a DNE and identified potential recessive ALPL mutations. To identify other genetic factors that could trigger the HPP phenotype in heterozygotes for a recessive mutation, we examined the next-generation sequencing (NGS) results of 32 of these patients for a panel of 12 genes involved in the differential diagnosis of HPP or candidate modifier genes of HPP. A coding SNP in COL1A2 was found to be associated with markers of severity.
Materials and methods
Patients and ALPL gene sequencing
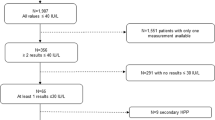
With the exception of patient 51 who was studied at the Universitätsklinikum Freiburg, Germany, all patients were tested for diagnostic purposes in our laboratory and signed a consent form. All the patients were unrelated excepted patients 8 (daughter) and 9 (mother). Seventy-two percent of the 61 patients were ascertained in France, while the others were from European countries, the USA or Australia. Eighty percent of the patients were female. They presented various features ranging from recurrent fractures and bone fragility to mild and nonpathognomonic symptoms such as musculoskeletal pain, diffuse pain, osteomalacia and osteopenia or symptoms resembling osteoporosis, calcifications and chondrocalcinosis. Patients were included in the study if they were found to carry only one heterozygous mutation after the entire coding sequence of the ALPL gene and intron/exon borders were analyzed by Sanger methodology or NGS. Mutations detected by NGS were confirmed by Sanger methodology. The patients were also screened for large deletions by either semi-quantitative polymerase chain reaction (PCR), quantitative PCR, arrayCGH or by NGS with the software CovCop [27]. Although none of these methodologies detect deletions exhaustively, we considered that these patients did not carry a large heterozygous deletion.
Classification of mutations
Mutations were classified according to their localization in TNSALP. The 3D structure was previously modeled from the crystal structure of the human placental AP [10, 11]. It allows the localization of residues affected by mutations in five crucial domains (active site, homodimer interface, crown domain, calcium site, N-terminal alpha helix) or in other regions of the protein. The model was visualized using the open source software PyMol version 0.98 (Delano Scientific LLC).
DNE of mutations
Mutations were assumed to have a DNE if they were previously shown to have this effect by coexpression studies, i.e., the residual enzymatic activity of cotransfected cells is <50% of wild-type (WT) activity, the value expected in the recessive model [15, 28,29,30,31,32,33,34,35]. The cut-off dominant effect/no dominant effect was set to 45% of WT activity for mutations with no residual activity. For mutations with residual activity, the cut-off was 0.90 (100 + activity)/2 expressed as % of WT. For instance, a mutation with 25% of residual activity will have a DNE if the residual activity of cotransfected cells is less than the cut-off 0.9(100 + 25)/2 = 56.25% (instead of 45% for a mutation with no residual activity). Insertions/deletions, splice site and nonsense mutations were assumed to have no DNE.
SNP genotyping
The COL1A2 SNP rs42524 (chr7:94043239; Hg19) [c.1645C > G (p.Pro549Ala)] was genotyped partly by NGS and partly by allelic discrimination with real-time PCR using a Taqman probe (Thermofisher).
Statistical calculations
Statistical calculations were performed using the open access calculator http://www.socscistatistics.com. Differences between distributions were assessed by chi-squared tests, comparison of means by t tests, and comparisons of proportions by Z tests.
Results
Mutations with a DNE
Among the 334 mutations reported in the ALPL gene mutation database (http://www.sesep.uvsq.fr/03_hypo_mutations.php, accessed on March 31, 2017), 46 missense mutations were tested for a DNE by various investigators [15, 28,29,30,31,32,33,34,35,36,37,38,39,40,41,42], and the results were listed in the database. We localized each tested mutation on the 3D model and found that 97% (29/30) of the mutations with a reported DNE were localized in the crown domain, the active site or its vicinity, or in the homodimer interface. In contrast, only 37% (6/16) of the mutations with no DNE were localized in these regions (p < 10−5, chi-squared test) that harbor 44% of all missense mutations listed in the database. This corroborates our previous results reporting that most of the amino acids affected by dominant mutations were clustered in these particular domains of the protein [15].
Statistical classification of mutations in adult patients heterozygous for an ALPL mutation
We localized where the 42 missense mutations that were found in the patients occurred in the protein (Table 1). The mutations were then divided into three classes. Class 1 includes missense mutations localized in the homodimer interface, the crown domain or the active site. This class was predicted to contain most of the missense mutations with a DNE but also possibly mutations with no DNE. Class 2 includes missense mutations localized in other regions and is statistically composed of mutations with no detectable DNE. These mutations may be recessive with the phenotype triggered by another factor in combination with the ALPL mutation, or may be responsible for another mechanism of dominance such as haploinsufficiency, or alternatively may constitute DNE not detectable by activity measurement [43]. Class 3 includes non-missense mutations, as well as the missense mutation c.791A > G (p.Lys264Arg), for which the major effect is to lead to the complete skipping of exon 7 [44]. These mutations are assumed to have no DNE. We found that only 27 (44%) of the patients carried a mutation of class 1, suggesting that, according to our statistical classification, over half (56%) of the patients carry an ALPL mutation that does not show a DNE. In contrast to the adult patients, the heterozygous patients with other clinical forms in our cohort were preferentially carrying class 1 mutations, from 76% in odontoHPP (n = 45) to 83% in childhood HPP (n = 18), and 100% in the PB form (n = 6) (not shown). When considering three parameters reflecting the severity of the phenotype (age of first symptoms, serum AP activity and history of fractures) we found that patients with class 1 mutations seem to be slightly more severely affected. The differences were statistically significant for serum AP and borderline for the age of diagnosis (Table 2). Among 22 informative cases, familial history was documented in 70% of class 1 and in 50% of classes 2 or 3 patients.
NGS analysis
We examined the NGS results of 32 patients tested for a panel of 12 genes involved in HPP (ALPL and promoter region), in the differential diagnosis of HPP (COL1A1, COL1A2, FGFR3 and SOX9) or candidates as modifier genes of HPP (ANKH, ENPP1, PHOSPHO1, PTH1R, PTH2R, SPP1 and TNFRSF11A) [45]. Among the 280 variants detected in these genes, three revealed statistically significant heterogeneity in their distribution depending on the class of mutation: rs2277632 in COL1A1 (p = 1.1 10−2), rs42524 in COL1A2 (p = 5.9 10−3) and rs42518 in COL1A2 (p = 7.2 10−3); the two latter variants were in strong linkage disequilibrium, and we finally focused on the variant rs42524 because it is coding and because it had the most significant p value. Genotyping of rs42524 was extended to other patients by allelic discrimination using a Taqman® probe, allowing confirmation that this variant statistically differed in its distributions in class 1 and classes 2 + 3 (chi-squared = 7.81, p = 5.2 10−3, Table 3). Fifty-six percent of patients with class 1 were found to carry the heterozygous genotype G/C, whereas only 21% of patients of class 2 or 3 carry this genotype. The latter were found to be under-represented when compared with a sample of 109 unrelated individuals from the general French population (Table 3). Thus, there is a relationship between the genotype at this locus and the class of ALPL mutation. As with class 1 mutations (Fig. 1a), the heterozygous genotype G/C is statistically associated with a more severe phenotype (Fig. 1b), suggesting that it could contribute to aggravation of the phenotype. The sample size was too small in some categories (especially G/C classes 2 and 3) to perform statistical analysis on split data; however, the age of onset was significantly lower in patients with G/C in class 1 than in classes 2 and 3 (32.3 ± 10.6 years vs 51.0 ± 12.1, respectively, p = 8.7 10−4), whereas there was no significant difference between the G/C and G/G genotypes in classes 2 and 3 and G/G in class 1 (51.0 ± 12.1, 51.4 ± 18.0 and 46.3 ± 18.6, respectively) (Fig. 1c). The same was observed for AP level where GC class 1 patients have significantly lower AP than others (50.1 ± 12 vs 64.5 ± 16; p = 4.6 10−3). This suggests that the possible aggravating role of G/C is conditioned on mutations with a DNE. Regarding the history of fractures, GC class 2 and 3 seem to be the most severe combination; however, the number of informative cases was very low in this category (n = 7). Finally, our results suggest that the rs42524 COL1A2 SNP could be a modifier gene of HPP at least in adults heterozygous for ALPL mutations.
Comparison of classes of mutations and rs42524 genotypes for three markers of phenotypic severity—age of onset (years), serum AP (% of the lower limit of the normal range), and absence of fractures (% of patients). The latter corresponds to the proportion of patients with no reported history of no traumatic fractures. a Classes of mutation, b COL1A2 rs42524 genotypes G/G and G/C, c classes of mutation and COL1A2 rs45524 genotypes taken together
Discussion
Classically, autosomal dominant inheritance may be due to negative interactions between WT and mutated proteins (DNE), addition of a new property of the protein (gain of function), or inability to produce enough protein with the WT allele (haploinsufficiency). Similar mechanisms are also found at the RNA level. Due to the homodimeric structure of functional TNSALP [9], dominant HPP is believed to result from the DNE of loss-of-function mutations, and this has been experimentally confirmed for many mutations. However, there is no biological argument excluding the possibility of other causes of dominant HPP. Here, we separated the ALPL mutations detected in adult heterozygotes in three groups according to their molecular consequence and their localization, and we found that only one-half of the patients carry a mutation with a predicted DNE. We hypothesized that class 2 and class 3 mutations had no DNE. This was expected for mutations c.187_205del and p.L6X resulting in early termination of translation, experimentally established for five missense mutations previously tested with site-directed mutagenesis (p.R136H, p.E191K, p.G249V, p.V431A, p.I490F), and predicted by 3D modeling for the remaining missense mutations. With respect to localization and molecular effect, the variety of class 2 and class 3 mutations does not support a mechanism of gain of function, although we do not exclude a particular mutation that could exhibit such a mechanism. Overall, however, we hypothesize that class 2 and class 3 mutations might not result in gain of function or in DNE defined here as the negative interaction between the WT and the mutated TNSALP monomers, which is experimentally detectable by the inhibition of WT AP activity. More likely, these mutations result in another mechanism of dominance. Most of the class 2 and 3 patients carry G/G suggesting an excess of this genotype or a lack of the G/C genotype when compared to the general population or to other patients with dominant HPP (childhood, odontoHPP and PB). All together, these data suggest that adults heterozygous for ALPL mutations may express a disease phenotype resulting from ALPL class 1 mutations, aggravated by COL1A2 G/C, or resulting from ALPL class 2 mutations, associated with COL1A2 G/G. Some patients with class 2 mutations and carrying COL1A2 G/C could be not symptomatic and therefore not ascertained, explaining their under-representation, or alternatively G/G could trigger the affected phenotype. An interesting example is patient 35 who was referred to us for hypercalcemia and low serum AP. She was found to carry the heterozygous class 2 mutation p.G491R and the COL1A2 G/C genotype. Finally the patient was diagnosed with primary hyperparathyroidism due to parathyroid hyperplasia which explained her hypercalcemia. In this scheme, the G/C genotype aggravates the DNE of class 1 mutations but has a neutral effect in patients with class 2 mutations. These results could marginally explain some cases of weak genotype–phenotype correlation in adult HPP [5, 46,47,48,49,50,51]. We are aware that these proposals, based on very preliminary results, remain speculative until the study of larger cohorts and/or coexpression of COL1A2 and TNSALP experiments will be performed.
A scaffold of fibrillar collagen type 1 is needed in the extracellular space to allow elongation of mineralization, and TNSALP is known to bind to collagen [52, 53]. In addition mutations in COL1A2 are responsible for osteogenesis imperfecta, the major differential diagnosis of HPP regardless of the clinical form considered [45, 54, 55]. The aggravating effect reported here was found only in patients with class 1 mutations. This suggests that the negative interaction between WT and mutated TNSALPs, i.e., the DNE, is potentiated by the collagen scaffold issued from the G/C genotype, whereas the collagen scaffold from the reference genotype G/G does not negatively interact with TNSALPs. Previous studies reported associations of this SNP with various phenotypes including low bone mineral density in the Swedish population [56] and neovascular macular degeneration [57] and hypertensive intracerebral hemorrhage [58] in Japanese and Chinese populations, respectively. In these studies, the G/C genotype was determined to be at risk. It has been suggested that this effect on the phenotype was due to disadvantageous protein interactions in G/C subjects during the formation of collagen helices [56]. The TNSALP-collagen binding site corresponds to the crown domain [13, 14, 52, 59], a region belonging to the area with class 1 mutations, making such a potentiating effect consistent. Class 1 mutations affecting the crown domain seem to be more severe than other class 1 mutations for AP (48.1 vs 56.1, not significant), but there is no difference for age (38.7 vs 41.2) or fractures (0.50 vs 0.47). Studies of TNSALP-COL1A2 interactions in patient-derived fibroblasts harboring various genotypes could provide an experimental confirmation of these results.
The patients studied here are at the mildest extremity of the HPP clinical spectrum. In this category, the disease and the normal phenotypes overlap, and it cannot be excluded that a portion of these patients are genuine heterozygotes for a recessive mutation not responsible for the symptoms. We noticed that the proportion of adult HPP patients referred to our laboratory who were heterozygous for a class 2 mutation increased from 25 to 50% before and after 2010, respectively, reflecting that although low AP is not well recognized by many clinicians [60], there is an increasing awareness among specialists regarding this warning sign. ALPL mutation testing is being increasingly requested, confirming the need to manage mutation findings by thorough clinical examination to distinguish HPP patients and simple carriers. Genotyping the rs42524 SNP as well could be useful to correlate the phenotype with the genotype.
In conclusion we found here that the rs42524 COL1A2 SNP modulates the phenotype of patients heterozygous for ALPL mutations. These findings and their resulting hypotheses remain very speculative and must be confirmed by testing more patients, and by coexpression experiments in order to confirm the hypotheses presented here.
Abbreviations
- ALPL:
-
Alkaline phosphatase liver-type
- AP:
-
Alkaline phosphatase
- DNE:
-
Dominant negative effect
- HPP:
-
Hypophosphatasia
- NGS:
-
Next-generation sequencing
- PB:
-
Prenatal benign
- TNSALP:
-
Tissue nonspecific alkaline phosphatase
References
Whyte MP (2017) Hypophosphatasia: an overview For 2017. Bone. https://doi.org/10.1016/j.bone.2017.02.011
Wenkert D, McAlister WH, Coburn SP, Zerega JA, Ryan LM, Ericson KL, Hersh JH, Mumm S, Whyte MP (2011) Hypophosphatasia: nonlethal disease despite skeletal presentation in utero (17 new cases and literature review). J Bone Miner Res 26:2389–2398
Bloch-Zupan A (2016) Hypophosphatasia: diagnosis and clinical signs − a dental surgeon perspective. Int J Paediatr Dent 26:426–438
Berkseth KE, Tebben PJ, Drake MT, Hefferan TE, Jewison DE, Wermers RA (2013) Clinical spectrum of hypophosphatasia diagnosed in adults. Bone 54:21–27
Briot K, Roux C (2016) Adult hypophosphatasia. Curr Opin Rheumatol 28:448–451
Shapiro JR, Lewiecki EM (2017) Hypophosphatasia in adults: clinical assessment and treatment considerations. J Bone Miner Res. https://doi.org/10.1002/jbmr.3226
Whyte MP (2010) Physiological role of alkaline phosphatase explored in hypophosphatasia. Ann N Y Acad Sci 1192:190–200
Whyte MP, Greenberg CR, Salman NJ, Bober MB, McAlister WH et al (2012) Enzyme-replacement therapy in life-threatening hypophosphatasia. N Engl J Med 366:904–913
Millan J (2006) Mammalian alkaline phosphatases: from biology to applications in medicine and biotechnology. Wiley-VCH Verlag GmbH, Weinheim
Le Du MH, Stigbrand T, Taussig MJ, Menez A, Stura EA (2001) Crystal structure of alkaline phosphatase from human placenta at 1.8 A resolution. Implication for a substrate specificity. J Biol Chem 276:9158–9165
Mornet E, Stura E, Lia-Baldini AS, Stigbrand T, Menez A, Le Du MH (2001) Structural evidence for a functional role of human tissue nonspecific alkaline phosphatase in bone mineralization. J Biol Chem 276:31171–31178
Mornet E (2008) Hypophosphatasia. Best Pract Res Clin Rheumatol 22:113–127
Vittur F, Stagani L, Moro L, de Bernard B (1984) Alkaline phosphatase binds to collagen: a hypothesis on the mechanism of extravesicular mineralization in epiphyseal cartilage. Experientia 40:836–837
Wu LN, Genge BR, Llyod GC, Wuthier RE (1991) Collagen-binding proteins in collagenase-released matrix vesicles from cartilage. Interaction between matrix vesicle proteins and different types of collagen. J Biol Chem 266:1195–1203
Fauvert D, Brun-Heath I, Lia-Baldini AS, Bellazi L, Taillandier A, Serre JL, de Mazancourt P, Mornet E (2009) Mild forms of hypophosphatasia mostly result from dominant negative effect of severe alleles or from compound heterozygosity for severe and moderate alleles. BMC Med Genet 10:51
Eberic FHS, Pralle H, Kabish A (1984) Adult hypophosphatasia without apparent skeletal disease: “ondotohypophosphatasia” in four heterozygote members of a family. Klin Wochenschr 62:371
Eastman JR, Bixler D (1983) Clinical, laboratory, and genetic investigations of hypophosphatasia: support for autosomal dominant inheritance with homozygous lethality. J Craniofac Genet Dev Biol 3:213–234
Whyte MP (2017) Hypophosphatasia: an overview For 2017. Bone 102:15–25. https://doi.org/10.1016/j.bone.2017.02.011
Fraser D (1957) Hypophosphatasia. Am J Med 22:730–746
Mornet E, Yvard A, Taillandier A, Fauvert D, Simon-Bouy B (2011) A molecular-based estimation of the prevalence of hypophosphatasia in the European population. Ann Hum Genet 75:439–445
McKiernan FE, Berg RL, Fuehrer J (2014) Clinical and radiographic findings in adults with persistent hypophosphatasemia. J Bone Miner Res 29:1651–1660
Nielson CM, Zmuda JM, Carlos AS, Wagoner WJ, Larson EA, Orwoll ES, K RF (2012) Rare coding variants in ALPL are associated with low serum alkaline phosphatase and low bone mineral density. J Bone Miner Res 27:93–103
Riancho-Zarrabeitia L, Garcia-Unzueta M, Tenorio JA, Gomez-Gerique JA, Ruiz Perez VL, Heath KE, Lapunzina P, Riancho JA (2016) Clinical, biochemical and genetic spectrum of low alkaline phosphatase levels in adults. Eur J Intern Med 29:40–45
McKiernan FE, Dong J, Berg RL, Scotty E, Mundt P, Larson L, Rai I (2017) Mutational and biochemical findings in adults with persistent hypophosphatasemia. Osteoporos Int 28:2343–2348
Tenorio J, Alvarez I, Riancho-Zarrabeitia L, Martos-Moreno GA, Mandrile G et al (2017) Molecular and clinical analysis of ALPL in a cohort of patients with suspicion of hypophosphatasia. Am J Med Genet A 173:601–610. https://doi.org/10.1002/ajmg.a.37991
Nielson CM, Zmuda JM, Carlos AS, Wagoner WJ, Larson EA, Orwoll ES, Klein RF (2012) Rare coding variants in ALPL are associated with low serum alkaline phosphatase and low bone mineral density. J Bone Miner Res 27:93–103
Derouault P, Parfait B, Moulinas R, Barrot CC, Sturtz F, Merillou S, Lia AS (2017) ‘COV’COP’ allows to detect CNVs responsible for inherited diseases among amplicons sequencing data. Bioinformatics 33:1586–1588. https://doi.org/10.1093/bioinformatics/btx017
Lia-Baldini AS, Muller F, Taillandier A, Gibrat JF, Mouchard M, Robin B, Simon-Bouy B, Serre JL, Aylsworth AS, Bieth E, Delanote S, Freisinger P, Hu JC, Krohn HP, Nunes ME, Mornet E (2001) A molecular approach to dominance in hypophosphatasia. Hum Genet 109:99–108
Numa-Kinjoh N, Komaru K, Ishida Y, Sohda M, Oda K (2015) Molecular phenotype of tissue-nonspecific alkaline phosphatase with a proline (108) to leucine substitution associated with dominant odontohypophosphatasia. Mol Genet Metab 115:180–185
Ishida Y, Komaru K, Ito M, Amaya Y, Kohno S, Oda K (2003) Tissue-nonspecific alkaline phosphatase with an Asp(289) → Val mutation fails to reach the cell surface and undergoes proteasome-mediated degradation. J Biochem (Tokyo) 134:63–70
Ishida Y, Komaru K, Oda K (2011) Molecular characterization of tissue-nonspecific alkaline phosphatase with an Ala to Thr substitution at position 116 associated with dominantly inherited hypophosphatasia. Biochim Biophys Acta 1812:326–332
Sultana S, Al-Shawafi HA, Makita S, Sohda M, Amizuka N, Takagi R, Oda K (2013) An asparagine at position 417 of tissue-nonspecific alkaline phosphatase is essential for its structure and function as revealed by analysis of the N417S mutation associated with severe hypophosphatasia. Mol Genet Metab 109:282–288
Yang H, Wang L, Geng J, Yu T, Yao RE, Shen Y, Yin L, Ying D, Huang R, Zhou Y, Chen H, Liu L, Mo X, Shen Y, Fu Q, Yu Y (2013) Characterization of six missense mutations in the tissue-nonspecific alkaline phosphatase (TNSALP) gene in Chinese children with hypophosphatasia. Cell Physiol Biochem 32:635–644
Muller HL, Yamazaki M, Michigami T, Kageyama T, Schonau E, Schneider P, Ozono K (2000) Asp361Val Mutant of alkaline phosphatase found in patients with dominantly inherited hypophosphatasia inhibits the activity of the wild-type enzyme. J Clin Endocrinol Metab 85:743–747
Zhu T, Gan YH, Liu H (2012) Functional evaluation of mutations in the tissue-nonspecific alkaline phosphatase gene. Chin J Dent Res 15:99–104
Makita S, Al-Shawafi HA, Sultana S, Sohda M, Nomura S, Oda K (2012) A dimerization defect caused by a glycine substitution at position 420 by serine in tissue-nonspecific alkaline phosphatase associated with perinatal hypophosphatasia. FEBS J 279:4327–4337
Mentrup B, Marschall C, Barvencik F, Amling M, Plendl H, Jakob F, Beck C (2011) Functional characterization of a novel mutation localized in the start codon of the tissue-nonspecific alkaline phosphatase gene (in eng). Bone 48:1401–1408. https://doi.org/10.1016//j.bone.2011.03.676
Taillandier A, Lia-Baldini AS, Mouchard M, Robin B, Muller F, Simon-Bouy B, Serre JL, Bera-Louville A, Bonduelle M, Eckhardt J, Gaillard D, Myhre AG, Kortge-Jung S, Larget-Piet L, Malou E, Sillence D, Temple IK, Viot G, Mornet E (2001) Twelve novel mutations in the tissue-nonspecific alkaline phosphatase gene (ALPL) in patients with various forms of hypophosphatasia. Hum Mutat 18:83–84
Takinami H, Goseki-Sone M, Watanabe H, Orimo H, Hamatani R, Fukushi-Irie M, Ishikawa I (2004) The mutant (F310L and V365I) tissue-nonspecific alkaline phosphatase gene from hypophosphatasia. J Med Dent Sci 51:67–74
Komaru K, Satou Y, Al-Shawafi HA, Numa-Kinjoh N, Sohda M, Oda K (2016) Glycosylation-deficient mutations in tissue-nonspecific alkaline phosphatase impair its structure and function and are linked to infantile hypophosphatasia. FEBS J 283:1168–1179
Hofmann C, Liese J, Schwarz T, Kunzmann S, Wirbelauer J, Nowak J, Hamann J, Girschick H, Graser S, Dietz K, Zeck S, Jakob F, Mentrup B (2013) Compound heterozygosity of two functional null mutations in the ALPL gene associated with deleterious neurological outcome in an infant with hypophosphatasia. Bone 55:150–157. https://doi.org/10.1016/j.bone.2013.02.017
Al-Shawafi HA, Komaru K, Oda K (2017) Molecular defect of tissue-nonspecific alkaline phosphatase bearing a substitution at position 426 associated with hypophosphatasia. Mol Cell Biochem 427:169–176. https://doi.org/10.1007/s11010-016-2908-6
Lia-Baldini AS, Brun-Heath I, Carrion C, Simon-Bouy B, Serre JL, Nunes ME, Mornet E (2008) A new mechanism of dominance in hypophosphatasia: the mutated protein can disturb the cell localization of the wild-type protein. Hum Genet 123:429–432
Brun-Heath I, Chabrol E, Fox M, Drexler K, Petit C, Taillandier A, De Mazancourt P, Serre JL, Mornet E (2008) A case of lethal hypophosphatasia providing new insights into the perinatal benign form of hypophosphatasia and expression of the ALPL gene. Clin Genet 73:245–250
Taillandier A, Domingues C, De Cazanove C, Porquet-Bordes V, Monnot S et al (2015) Molecular diagnosis of hypophosphatasia and differential diagnosis by targeted next generation sequencing. Mol Genet Metab 116:215–220
Mornet E (2017) The tissue nonspecific alkaline phosphatase gene mutations database. Université de Versailles Saint-Quentin en Yvelines. Accessed May 21, 2017
Whyte MP, Zhang F, Wenkert D, McAlister WH, Mack KE, Benigno MC, Coburn SP, Wagy S, Griffin DM, Ericson KL, Mumm S (2015) Hypophosphatasia: validation and expansion of the clinical nosology for children from 25 years experience with 173 pediatric patients. Bone 75:229–239
Hofmann C, Girschick H, Mornet E, Schneider D, Jakob F, Mentrup B (2014) Unexpected high intrafamilial phenotypic variability observed in hypophosphatasia. Eur J Hum Genet 22:1160–1164. https://doi.org/10.1038/ejhg.2014.10
Taketani T, Onigata K, Kobayashi H, Mushimoto Y, Fukuda S, Yamaguchi S (2014) Clinical and genetic aspects of hypophosphatasia in Japanese patients. Arch Dis Child 99:211–215
Moulin P, Vaysse F, Bieth E, Mornet E, Gennero I, Dalicieux-Laurencin S, Baunin C, Tauber MT, De Gauzy JS, Salles JP (2009) Hypophosphatasia may lead to bone fragility: don’t miss it. Eur J Pediatr 168:783–788
Hu JC, Plaetke R, Mornet E, Zhang C, Sun X, Thomas HF, Simmer JP (2000) Characterization of a family with dominant hypophosphatasia. Eur J Oral Sci 108:189–194
Bossi M, Hoylaerts MF, Millan JL (1993) Modifications in a flexible surface loop modulate the isozyme-specific properties of mammalian alkaline phosphatases. J Biol Chem 268:25409–25416
Cui L, Houston DA, Farquharson C, MacRae VE (2016) Characterisation of matrix vesicles in skeletal and soft tissue mineralisation. Bone 87:147–158. https://doi.org/10.1016/j.bone.2016.04.007
Mornet E, Beck C, Bloch-Zupan A, Girschick H, Le Merrer M (2011) Clinical utility gene card for: hypophosphatasia. Eur J Hum Genet 19(3). https://doi.org/10.1038/ejhg.2010.170
Byers PH, Krakow D, Nunes ME, Pepin M (2006) Genetic evaluation of suspected osteogenesis imperfecta (OI). Genet Med 8:383–388
Lindahl K, Rubin CJ, Brändström H, Karlsson MK, Holmberg A, Ohlsson C, Mellström D, Orwoll E, Mallmin H, Kindmark A, Ljunggren O (2009) Heterozygosity for a coding SNP in COL1A2 confers a lower BMD and an increased stroke risk. Biochem Biophys Res Commun 384:501–505
Zuo C, Wen F, Li M, Zhang X, Chen H, Wu K, Zeng R (2012) COL1A2 polymorphic markers confer an increased risk of neovascular age-related macular degeneration in a Han Chinese population. Mol Vis 18:1787–1793
Liu W, Pang B, Lu M, Song H, Sun B, Zhu Y, Pang Q (2012) The rs42524 COL1A2 polymorphism is associated with primary intracerebral hemorrhage in a Chinese population. J Clin Neurosci 19:1711–1714
Hoylaerts MF, Millan JL (1991) Site-directed mutagenesis and epitope-mapped monoclonal antibodies define a catalytically important conformational difference between human placental and germ cell alkaline phosphatase. Eur J Biochem 202:605–616
Maman E, Borderie D, Roux C, Briot K (2016) Absence of recognition of low alkaline phosphatase level in a tertiary care hospital. Osteoporos Int 27:1251–1254. https://doi.org/10.1007/s00198-015-3346-0
Acknowledgements
We thank Carole Charle, Nicole Lavaud and Fabienne Vallon for technical assistance, and the Centre Hospitalier de Versailles for contributing to a version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest statement
EM received honoraria from Alexion. CR received honoraria from Alexion and research grants from Ultragenix
About this article
Cite this article
Taillandier, A., Domingues, C., Dufour, A. et al. Genetic analysis of adults heterozygous for ALPL mutations. J Bone Miner Metab 36, 723–733 (2018). https://doi.org/10.1007/s00774-017-0888-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-017-0888-6