Abstract
Osteoporosis is a disease of poor bone quality. Bone mineral density (BMD) has limited ability to discriminate between subjects without and with poor bone quality, and assessment of bone microarchitecture may have added value in this regard. Our goals were to use 7 T MRI to: (1) quantify and compare distal femur bone microarchitecture in women without and with poor bone quality (defined clinically by presence of fragility fractures); and (2) determine whether microarchitectural parameters could be used to discriminate between these two groups. This study had institutional review board approval, and we obtained written informed consent from all subjects. We used a 28-channel knee coil to image the distal femur of 31 subjects with fragility fractures and 25 controls without fracture on a 7 T MRI scanner using a 3-D fast low angle shot sequence (0.234 mm × 0.234 mm × 1 mm, parallel imaging factor = 2, acquisition time = 7 min 9 s). We applied digital topological analysis to quantify parameters of bone microarchitecture. All subjects also underwent standard clinical BMD assessment in the hip and spine. Compared to controls, fracture cases demonstrated lower bone volume fraction and markers of trabecular number, plate-like structure, and plate-to-rod ratio, and higher markers of trabecular isolation, rod disruption, and network resorption (p < 0.05 for all). There were no differences in hip or spine BMD T-scores between groups (p > 0.05). In receiver-operating-characteristics analyses, microarchitectural parameters could discriminate cases and controls (AUC = 0.66–0.73, p < 0.05). Hip and spine BMD T-scores could not discriminate cases and controls (AUC = 0.58–0.64, p ≥ 0.08). We conclude that 7 T MRI can detect bone microarchitectural deterioration in women with fragility fractures who do not differ by BMD. Microarchitectural parameters might some day be used as an additional tool to detect patients with poor bone quality who cannot be detected by dual-energy X-ray absorptiometry (DXA).
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is defined as “a systemic skeletal disorder characterized by low bone mass and microarchitectural deterioration of bone tissue with a consequent increase in bone fragility and susceptibility to fracture” [1]. Because there is an association between areal bone mineral density (BMD) as measured by dual-energy X-ray absorptiometry (DXA) and fracture risk, DXA has become the standard-of-care test to diagnose osteoporosis [2, 3]. If a patient’s DXA-derived T-score (number of standard deviations below the mean BMD for a population of healthy young women) is less than −2.5, then the patient is considered as having osteoporosis [2]. A T-score less than −2.5 also serves as the threshold for treatment with osteoporosis medications [4].
However, there are limitations with the use of DXA to assess bone fragility and determine whether an individual has osteoporosis. First, factors other than BMD contribute to bone quality and risk of fracture [2, 5, 6]. For example, DXA does not assess bone microarchitecture, which is included in the definition of osteoporosis and is an important contributor to bone strength and quality [2, 7, 8]. Indeed, the addition of structural measures to BMD improves the prediction of bone strength in ex vivo studies [9–11]. Second, DXA has poor sensitivity for the detection of patients with bone fragility. There is a large overlap in the BMDs of patients with and without fragility fractures [3, 6, 12, 13], and approximately two-thirds of the patients who suffer low-energy, fragility fractures are misclassified as not having osteoporosis because they have BMD T-scores greater than −2.5 [14–17]. The limitations of DXA in this regard have sparked research into the use of other modalities to assess bone quality and strength in vivo [18, 19].
Over the last 15 years, there has been an increasing number of publications describing the in vivo assessment of bone microarchitecture, either by high-resolution magnetic resonance imaging (MRI) [7, 20], or most recently, high resolution peripheral quantitative computed tomography (HR-pQCT) [21–25]. These studies have been carried out predominantly at the distal radius or distal tibia, because imaging at other locations in the body has been too technically challenging. Via HRpQCT, the small scanner bore size precludes imaging anything but the wrist or ankle. And via MRI, it is challenging to image bone microarchitecture at more proximal locations because of signal-to-noise ratio (SNR) limitations. These SNR limitations arise because in more proximal skeletal locations, the bones are deeper within the body and thus more distant from the radiofrequency coil that is placed on the patient and used for MRI signal detection. For example, the distal radius and tibia are only 1–2 cm from the skin surface, but the distal femur is 2–5 cm from the skin surface, and the proximal femur is 5–8 cm from the skin surface. Since SNR decreases rapidly with increasing distance, imaging microarchitecture for deeper skeletal structures becomes challenging.
The goal of this study was to investigate if high-resolution, 7 T MRI is capable of extending the bone microarchitecture analysis previously only feasible at distal peripheral sites to a more proximal location (i.e., the distal femur), and able to differentiate women with and without osteoporotic fragility fracture. We hypothesized that: (1) subjects with fragility fractures would demonstrate deterioration in bone microarchitecture in the distal femur compared to controls, and (2) microarchitectural parameters could be used to discriminate between subjects with and without fragility fractures. We also examined: (1) differences in DXA-derived BMD T-scores between groups, and (2) the ability of BMD T-scores to discriminate between women with and without fragility fractures.
Materials and methods
Subject recruitment
This study had institutional review board approval, and we obtained written informed consent from all subjects. We followed a case–control study design of subjects with and without fragility fractures similar to the work of Melton and Nishiyama [22, 23, 26]. From the Osteoporosis Center at our institution, we recruited women with radiographically confirmed, low-energy fragility fractures (n = 31, age = 56.9 ± 17.2 years, body mass index (BMI) = 22.2 ± 3.6 kg/m2) and female controls without fragility fractures (n = 25, age = 50.0 ± 19.5 years, BMI = 20.5 ± 1.8 kg/m2). The type and distribution of fragility fractures were: spine = 16, forearm = 8, sacrum = 4, hip = 3. We excluded patients with a history of knee osteoarthritis, trauma, Paget’s disease, or other musculoskeletal disorder that could affect the distal femur. The differences in age and BMI between groups were not statistically significant (p > 0.1 for age and p > 0.07 for BMI). As in prior studies, a fragility fracture was defined as a fracture due to a fall from a standing height or less [22, 25]. The average time since fragility fracture was 5.7 ± 3.0 months. Subjects underwent standard DXA testing (GE Lunar, Rahway, NJ, USA) to assess T-scores in the hips (total) and the spine (L1–L4). For any analysis, we used the hip T-score for the same lower extremity that we scanned by MRI.
MRI scanning
The distal femur of the dominant lower extremity of all subjects was scanned on a whole body 7 T MRI scanner (Siemens Magnetom, Erlangen, Germany) using a birdcage transmit, 28-channel receive array coil (Quality Electrodynamics, Mayfield Village Ohio). We used a 3-D fast low angle shot sequence to image bone microarchitecture (TR/TE = 20 ms/5.1 ms, field of view = 120 mm, matrix = 512 × 512, in-plane resolution 0.234 mm × 0.234 mm, slice thickness = 1 mm, 80 axial images, parallel acceleration factor = 2, acquisition time = 7 min and 9 s) [27–29].
MR image analysis
We analyzed bone microarchitecture within volumes of interest (VOIs) in two locations: the distal femoral metaphysis (DFM) and the distal femoral epiphysis (DFE). To identify the DFM and DFE, a musculoskeletal radiologist identified the growth plate on sagittal and coronal localizer MR images. The DFM VOI was designated as the ten slices superior to the growth plate and the DFE VOI was designated as the ten slices inferior to the growth plate (Fig. 1).
To each volume of interest, we applied digital topological analysis (DTA). DTA [30, 31] is a 3-D method that accurately determines the topological class (e.g., surfaces, curves, junctions, and edges) of each individual location in a digitized structure that has been applied for quantifying quality of trabecular bone architectural makeup. Before applying DTA, a binarized trabecular bone image is skeletonized to a network of 1-D and 2-D structures representing rods and plates, respectively. DTA involves three steps; the first one is inspecting each bone voxel’s neighboring voxels (i.e., the 26 other voxels within the voxel’s 3 × 3 × 3 kernel). A unique topological classification can be achieved using lookup tables solving for local topological ambiguities in digital manifolds and their junctions. These topological classes are used to compute several topological parameters for trabecular bone (TB) networks. We computed: bone volume fraction (BVF) and apparent trabecular thickness (Tb·Th), as well as markers of: trabecular number (skeleton density, Sk.D), the ends of trabecular rod-like structure or trabecular rod disruption (curve edge, CEnorm), trabecular plate-like structure (surface, Surf), trabecular plate-to-rod ratio (surface–curve, Surf–Curv), trabecular network connectivity (junctions, Junc), trabecular network osteoclastic resorption (Erosion Index), and finally, trabecular isolation (Inorm). These parameters were chosen because in previous bone biopsy studies, they have been shown to deteriorate in patients with osteoporosis [32, 33]. The coefficient of variation for microarchitectural parameters in the distal femur with this image analysis and MRI technique has previously been shown to be 0.8–5.6 % [27].
Statistical analysis
We used SPSS v.20 (IBM, Armonk, New York) to perform statistical analysis. To compare differences between groups, we used the nonparametric Mann–Whitney test, which does not depend on a normal distribution of data (the results of a t test may be unduly influenced by outlier values). To assess the correlation between the bone volume fraction and microarchitectural parameters, we used the Spearman non-parametric test. A p value less than 0.05 was considered statistically significant. To determine the ability of a parameter to discriminate between fracture cases and controls, we performed a receiver operating characteristics (ROC) analysis and computed the area under the curve (AUC), including confidence intervals and p values.
Results
Differences between groups
Figure 2a shows representative axial 7 T MR images of the distal femoral metaphysis in patients with and without fragility fractures. Individual trabeculae are well depicted on the images. At the distal femoral metaphysis, compared to controls, fracture cases demonstrated lower values for markers of trabecular number (skeleton density, −5.7 %), trabecular plate-like structure (Surf, −11.5 %), and trabecular connectivity (Junc, −9.6 %), and higher values for markers of trabecular isolation (Inorm, +450 %) and the disruption of trabecular rod-like structure (CEnorm, +341 %) (Table 1). There were no differences between groups for bone volume fraction, apparent trabecular thickness, or markers of trabecular plate-to-rod ratio (Surf/Curv) and trabecular network resorption (Erosion Index). For both controls and fracture cases at the distal femoral metaphysis, there were moderate to strong correlations between bone volume fraction, a marker of bone mass, and microarchitectural parameters (e.g., trabecular thickness, r = 0.43, p = 0.02; surf [trabecular plate-like structure], r = 0.99, p < 0.001) (Table 2). There was also no difference in BMD T-scores between groups (Table 3).
a Axial high-resolution 7 T MR images of the distal femoral metaphysis in a control (left T-scores = −1.3 in hip, −2.4 in spine) and a subject with a thoracic spine compression fracture (right T-scores = −1.5 in hip, −0.6 in spine). The whole area of trabecular bone was analyzed. The rectangles highlight an area of microarchitectural deterioration in the fracture case (fewer trabeculae, which are disrupted and have less connectivity) and for comparison, the same area within the control. In MR images, trabeculae are hypointense (dark) and marrow is hyperintense (white). b Axial high-resolution 7 T MR images of the distal femoral epiphysis in a control (left T-scores = −2.6 in hip, −1.6 in spine) and a subject with a thoracic spine compression fracture (right T-scores = −2.8 in hip, −2.1 in spine). The whole area of trabecular bone was analyzed. The rectangles highlight an area of microarchitectural deterioration in the fracture case (fewer trabeculae, which are disrupted and have less connectivity), and for comparison, the same area within the control. The ovals highlight areas of microarchitectural deterioration seen medially both within the control and the fracture case. In MR images, trabeculae are hypointense (dark) and marrow is hyperintense (white)
Figure 2b shows representative axial 7 T MR images of the distal femoral epiphysis in patients with and without fragility fractures. Again, individual trabeculae are well depicted on the images. At the distal femoral epiphysis, compared to controls, the fracture cases demonstrated lower bone volume fraction (−3.1 %), and lower values for markers of trabecular number (skeleton density, −5.4 %), trabecular plate-like structure (Surf, −10.3 %), trabecular connectivity (Junc, −9.7 %), and trabecular plate-to-rod ratio (Surf/Curv, −11.4 %). Fracture cases also demonstrated higher values for markers of the disruption of trabecular rod-like structure (CEnorm, +764 %), trabecular isolation (Inorm, +881 %), and trabecular network resorption (Erosion Index, +6.2 %) (Table 1). There was no difference in apparent trabecular thickness between groups. For both controls and fracture cases at the distal femoral epiphysis, there were moderate to strong correlations between bone volume fraction, a marker of bone mass, and microarchitectural parameters (e.g., trabecular thickness, r = 0.41, p = 0.02; erosion index (marker of trabecular network resorption), r = −0.95, p < 0.001) (Table 2).
ROC analyses
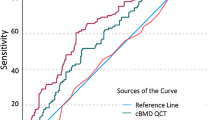
At the distal femoral metaphysis, the parameters skeleton density (AUC = 0.67), Inorm (AUC = 0.68), CEnorm (AUC = 0.70), Surf (AUC = 0.66), and Junc (AUC = 0.67) could be used to discriminate between groups (p < 0.05 for all, Table 4). Bone volume fraction, apparent trabecular thickness, Surf/Curv, and Erosion Index could not be used discriminate between groups (AUC confidence intervals included 0.5, p values >0.05).
At the distal femoral epiphysis, bone volume fraction (AUC = 0.73), skeleton density (AUC = 0.70), Inorm (AUC = 0.73), CEnorm (AUC = 0.72), Surf (AUC = 0.72), Junc (AUC = 0.67), Surf/Curv (AUC = 0.68), and Erosion Index (AUC = 0.66) could all be used to discriminate between groups (p < 0.05 for all, Table 4). Apparent trabecular thickness could not be used to discriminate between groups (AUC confidence intervals included 0.5, p values >0.05.
Finally, hip and spine T-scores could not be used to discriminate between groups (AUC confidence intervals included 0.5, p values > 0.05, Table 5).
Discussion
In this study, we used high-resolution 7 T MRI to evaluate trabecular bone microarchitecture at the distal femoral metaphysis and epiphysis in women with known poor bone quality (fragility fractures) and female controls without fracture. 7 T MRI was able to detect significant deterioration in bone microarchitectural parameters between groups, but there were no differences in DXA-derived BMD T-scores between groups. In addition, in ROC analyses, bone microarchitectural parameters could be used to discriminate between the two groups, but BMD T-scores could not be used to do this. The results provide further insight into how bone microarchitecture deteriorates in patients with fragility fractures, and also suggests that in vivo monitoring of such microarchitectural alterations might allow clinicians to discriminate between subjects without and with bone fragility who are at risk for fracture.
To the best of our knowledge, this is the first study to examine bone microarchitecture in the distal femur of patients with fragility fractures and the largest 7 T MRI study of patients with fragility fractures to date. MRI of bone microarchitecture was originally performed in the distal extremities [34–36], and it is only within the last few years that imaging of bone microarchitecture in more proximal locations of the skeleton has become possible due to improvements in radiofrequency coils and the arrival of high field and ultra high field MRI scanners [29, 37–39]. This study benefitted from both scanning at 7 T and the use of a 28-channel receive array coil to image the distal femur at high-resolution. Because image SNR is approximately linearly proportional with the magnitude of the main magnetic field, MRI at 7 T provides more than twofold higher SNR compared to MRI 3 T, and can thus permit reductions in imaging time and/or voxel size [40, 41]. In addition, the higher SNR provided by 7 T facilitates imaging of deeper anatomy such as the femur, since coil sensitivity for detection of the MR signal decreases exponentially as the distance from the coil to the object of interest increases [42]. Finally, the use of a 28-channel coil also facilitates high-resolution imaging, as the 28-channel coil at 7 T provides approximately 17–400 % higher image SNR compared to the use of a conventional 2-channel quadrature coil [43]. We leveraged the higher SNR provided by the 7 T MRI scanner and the 28-channel receive coil to decrease imaging time to 7 min and 9 s via parallel imaging, while still being able to acquire 80 axial images at 1 mm slice thickness. Decreasing imaging time is important for high-resolution exams, as this will decrease the risk of motion artifact on images. In the future, the additional SNR could also be used to improve in-plane spatial resolution or further decrease the slice thickness.
We found that fracture cases had lower values for markers of trabecular number (skeleton density), connectivity (Junc), plate-like structure (Surf), and plate-to-rod ratio (Surf/Curv), and higher values for markers of the disruption/ends of trabecular rod-like structure (CEnorm), trabecular isolation (Inorm), and trabecular network resoprtion (Erosion Index). All of these trends are consistent with increased osteoclastic (bone resorptive) activity and deterioration of bone microarchitecture/weakening of bone seen in landmark bone biopsy studies of osteoporosis [8, 32, 33]. The results are supportive of previous MRI studies of bone microarchitecture, which were carried out in the distal radius and ankle. Majumdar et al. [34] found that subjects with fragility fractures demonstrated lower bone volume fraction and Tb.N. in the distal radius compared to the controls. In a study of calcaneal microarchitecture, Link et al. [36] found lower bone volume fraction and Tb.N. in fracture cases compared to controls. Finally, Wehrli et al. [44] found that subjects with vertebral deformities demonstrated deterioration in parameters of bone microarchitecture at the distal radius that reflected a conversion of trabecular plates to rods as well as a disruption of trabecular rods. Osteoporosis is a “systemic skeletal disease” and the ideal site for bone quality/microarchitectural assessment remains to be determined. In the future, we hope to extend these methods to the proximal femur, which is the most devastating fragility fracture site (requires major surgery, greatest morbidity and mortality of all fractures), but also the most challenging to image because it is deeper in location (5–8 cm from the skin surface) and limited by low SNR. Both 7 T MRI and multichannel coils may again play a similar role in terms of facilitating high-resolution imaging in this location.
While the ability of 7 T MRI to detect differences between groups is useful from the research perspective in terms of providing insight into the pathogenesis of osteoporosis, clinical value would come from being able to use MRI of bone microarchitecture as a test to discriminate between subjects without and with poor bone quality. This has been a large motivating factor for the use of ultrasound to study calcaneal bone quality or HR-pQCT to study distal tibia/distal radius bone quality. If a clinical test could do this, then in theory if a patient were detected before they suffered a fracture, they could be started on one of the many effective bone-strengthening medications that can reduce fracture risk by up to 50 % [5]. Overall, our results provide evidence that measurement of microarchitectural parameters, even in a more proximal skeletal location such as the distal femur, might be able to detect patients with poor overall bone quality who are not currently detectable using DXA criteria for a diagnosis of osteoporosis. We found that microarchitectural measures in the distal femur could discriminate between patients with and without fragility fractures. However, there was no difference in BMD T-scores between cases and controls, and BMD T-scores could not discriminate between the two groups. The inability of DXA to do this highlights the poor sensitivity of DXA to identify individuals at risk for fracture, and the large overlap in BMDs of patients with and without fragility fractures [3, 6, 12, 13, 17, 45]. The discriminatory ability of microarchitectural parameters has been recently described in cross-sectional HR-pQCT studies of the distal radius. For example, in Melton et al.’s 2007 study of 18 females with forearm fractures and 18 controls, Tb.N. measured at the distal radius demonstrated an AUC of 0.72 for the discrimination of fracture cases from controls [22]. And more recently, Nishiyama et al. [23], in a study of 44 patients with any type of fragility fracture and 88 controls, found that microarchitectural parameters measured by HR-pQCT at the distal radius had an AUC of 0.67 for the discrimination of all fracture cases from controls. We found AUC values for bone microarchitectural parameters measured in the distal femur to be within a similar range.
Finally, we note that the parameter bone volume fraction (which is actually more akin to a marker of bone mass), when measured in the distal femoral epiphysis, performed as well as microarchitectural parameters for the discrimination of fracture cases and controls. This is reflected by its significant AUC value of 0.73, which was equal to the AUC value for the best performing microarchitectural parameter, Inorm. Furthermore, the confidence interval for this AUC value of bone volume fraction overlapped with confidence intervals for the AUC values of microarchitectural parameters. There was also moderate to very strong correlation between bone volume fraction and microarchitectural parameters (as demonstrated by the results in Table 2), which suggests that there is overlap in the bone quality information provided by bone volume fraction and microarchitectural measures. Overall, these results raise the question of whether bone volume fraction could be used alone to discriminate fracture status, rather than a microarchitectural measure. In the distal femoral metaphysis, bone volume fraction could not discriminate fracture cases from controls, even though microarchitectural parameters could do this. Because of the small sample size in this study, we did not have enough power to perform multivariable logistic modeling to determine which parameter or combination of parameters from which measurement site (metaphysis or epiphysis) would provide the highest AUC value. In the future, it will be necessary to perform larger patient studies in order to determine the measurement site and parameters (bone volume fraction, microarchitectural parameters, or a combination of both) that are most useful for the discrimination of fracture status and ultimately, assessment of fracture risk.
There are limitations to this study. First, because this is not a longitudinal study, we cannot draw any conclusions regarding the association between baseline microarchitectural measures and the occurrence of future fractures. Second, at the voxel size of this study 0.234 mm × 0.234 mm × 1 mm, we cannot depict trabeculae smaller than the voxel dimensions. Nevertheless, we could still visualize individual trabeculae on all images. MRI of bone microarchitecture requires high-resolution, but the long imaging times required by high-resolution MRI scans can increase the risk of patient motion artifact or discomfort. We felt that at the resolution of this study, there was a good balance between having adequate resolution to detect differences between groups and having a tolerable scan time to maintain patient comfort/low risk of motion artifact. Finally, this study was performed on an ultra high field, 7 T MRI scanner, which is not widely available in the community. However, over the last decade, there has been a steady rise in the number of 7 T MRI scanners being installed at academic medical centers worldwide (at least ten in the United States). Like high-resolution peripheral computed tomography (HR-pQCT) scanners, bone microarchitecture imaging could at least be used for noninvasive clinical research studies (as opposed to bone biopsy studies) at hospitals equipped with the scanners.
In conclusion, we have used 7 T MRI to investigate, for the first time, differences in distal femur bone microarchitecture in patients without and with poor bone quality (fragility fractures). There was deterioration of bone microarchitecture in fracture cases compared to controls, and microarchitectural parameters could be used to discriminate between the fracture subjects and controls even though these subjects did not differ by BMD. Overall, the results provide further insight into the role that bone microarchitecture plays in fracture pathogenesis, and the results suggest that evaluation of bone microarchitecture may allow detection of patients with bone fragility who are at higher risk for fracture and who cannot be detected by DXA. Longitudinal studies are necessary to determine whether microarchitectural parameters have added predictive value for the occurrence of future fracture, and to determine whether microarchitectural parameters can be used as surrogate endpoints for fracture in clinical trials for osteoporosis interventions.
References
Consensus development conference: diagnosis, prophylaxis, and treatment of osteoporosis (1993). Am J Med 94:646–650
Kanis JA (2002) Diagnosis of osteoporosis and assessment of fracture risk. Lancet 359:1929–1936
Marshall D, Johnell O, Wedel H (1996) Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ 312:1254–1259
Management of osteoporosis in postmenopausal women: 2010 position statement of The North American Menopause Society (2010). Menopause 17:25–54; quiz 55–26
Seeman E, Delmas PD (2006) Bone quality—the material and structural basis of bone strength and fragility. N Engl J Med 354:2250–2261
Cummings SR (1985) Are patients with hip fractures more osteoporotic? Review of the evidence. Am J Med 78:487–494
Wehrli FW (2007) Structural and functional assessment of trabecular and cortical bone by micro magnetic resonance imaging. J Magn Reson Imaging 25:390–409
Dempster DW (2000) The contribution of trabecular architecture to cancellous bone quality. J Bone Miner Res 15:20–23
Baum T, Kutscher M, Muller D et al (2013) Cortical and trabecular bone structure analysis at the distal radius-prediction of biomechanical strength by DXA and MRI. J Bone Miner Metab 31:212–221
Boehm HF, Horng A, Notohamiprodjo M et al (2008) Prediction of the fracture load of whole proximal femur specimens by topological analysis of the mineral distribution in DXA-scan images. Bone 43:826–831
Le Corroller T, Halgrin J, Pithioux M, Guenoun D, Chabrand P, Champsaur P (2012) Combination of texture analysis and bone mineral density improves the prediction of fracture load in human femurs. Osteoporos Int 23:163–169
Bohr H, Schaadt O (1983) Bone mineral content of femoral bone and the lumbar spine measured in women with fracture of the femoral neck by dual photon absorptiometry. Clin Orthop Relat Res 179:240–245
Ross PD, Davis JW, Vogel JM, Wasnich RD (1990) A critical review of bone mass and the risk of fractures in osteoporosis. Calcif Tissue Int 46:149–161
Cranney A, Jamal SA, Tsang JF, Josse RG, Leslie WD (2007) Low bone mineral density and fracture burden in postmenopausal women. CMAJ 177:575–580
Stone KL, Seeley DG, Lui LY et al (2003) BMD at multiple sites and risk of fracture of multiple types: long-term results from the Study of Osteoporotic Fractures. J Bone Miner Res 18:1947–1954
Wainwright SA, Marshall LM, Ensrud KE et al (2005) Hip fracture in women without osteoporosis. J Clin Endocrinol Metab 90:2787–2793
Schuit SC, van der Klift M, Weel AE et al (2004) Fracture incidence and association with bone mineral density in elderly men and women: the Rotterdam Study. Bone 34:195–202
Link TM (2012) Osteoporosis imaging: state of the art and advanced imaging. Radiology 263:3–17
Griffith JF, Engelke K, Genant HK (2010) Looking beyond bone mineral density: imaging assessment of bone quality. Ann NY Acad Sci 1192:45–56
Majumdar S (2002) Magnetic resonance imaging of trabecular bone structure. Top Magn Reson Imaging 13:323–334
Liu XS, Cohen A, Shane E et al (2010) Individual trabeculae segmentation (ITS)-based morphological analysis of high-resolution peripheral quantitative computed tomography images detects abnormal trabecular plate and rod microarchitecture in premenopausal women with idiopathic osteoporosis. J Bone Miner Res 25:1496–1505
Melton LJ 3rd, Riggs BL, van Lenthe GH et al (2007) Contribution of in vivo structural measurements and load/strength ratios to the determination of forearm fracture risk in postmenopausal women. J Bone Miner Res 22:1442–1448
Nishiyama KK, Macdonald HM, Hanley DA, Boyd SK (2013) Women with previous fragility fractures can be classified based on bone microarchitecture and finite element analysis measured with HR-pQCT. Osteoporos Int 24:1733–1740. doi:10.1007/s00198-012-2160-1
Melton LJ 3rd, Christen D, Riggs BL et al (2010) Assessing forearm fracture risk in postmenopausal women. Osteoporos Int 21:1161–1169
Boutroy S, Van Rietbergen B, Sornay-Rendu E, Munoz F, Bouxsein ML, Delmas PD (2008) Finite element analysis based on in vivo HR-pQCT images of the distal radius is associated with wrist fracture in postmenopausal women. J Bone Miner Res 23:392–399
Melton LJ 3rd, Riggs BL, Keaveny TM et al (2007) Structural determinants of vertebral fracture risk. J Bone Miner Res 22:1885–1892
Chang G, Wang L, Liang G, Babb JS, Saha PK, Regatte RR (2011) Reproducibility of subregional trabecular bone micro-architectural measures derived from 7-Tesla magnetic resonance images. MAGMA 24:121–125
Chang G, Rajapakse CS, Diamond M et al (2013) Micro-finite element analysis applied to high-resolution MRI reveals improved bone mechanical competence in the distal femur of female pre-professional dancers. Osteoporos Int 24:1407–1417
Chang G, Rajapakse CS, Babb JS, Honig SP, Recht MP, Regatte RR (2012) In vivo estimation of bone stiffness at the distal femur and proximal tibia using ultra-high-field 7-Tesla magnetic resonance imaging and micro-finite element analysis. J Bone Miner Metab 30:243–251
Saha PK, Chaudhuri BB (1996) 3D digital topology under binary transformation with applications. Comput Vis Image Underst 63:418–429
Saha PK, Gomberg BR, Wehrli FW (2000) Three-dimensional digital topological characterization of cancellous bone architecture. Int J Imaging Syst Technol 11:81–90
Kleerekoper M, Villanueva AR, Stanciu J, Rao DS, Parfitt AM (1985) The role of three-dimensional trabecular microstructure in the pathogenesis of vertebral compression fractures. Calcif Tissue Int 37:594–597
Amling M, Posl M, Ritzel H et al (1996) Architecture and distribution of cancellous bone yield vertebral fracture clues. A histomorphometric analysis of the complete spinal column from 40 autopsy specimens. Arch Orthop Trauma Surg 115:262–269
Majumdar S, Link TM, Augat P et al (1999) Trabecular bone architecture in the distal radius using magnetic resonance imaging in subjects with fractures of the proximal femur. Magnetic Resonance Science Center and Osteoporosis and Arthritis Research Group. Osteoporos Int 10:231–239
Wehrli FW, Hwang SN, Ma J, Song HK, Ford JC, Haddad JG (1998) Cancellous bone volume and structure in the forearm: noninvasive assessment with MR microimaging and image processing. Radiology 206:347–357
Link TM, Majumdar S, Augat P et al (1998) In vivo high resolution MRI of the calcaneus: differences in trabecular structure in osteoporosis patients. J Bone Miner Res 13:1175–1182
Blumenkrantz G, Lindsey CT, Dunn TC et al (2004) A pilot, 2-year longitudinal study of the interrelationship between trabecular bone and articular cartilage in the osteoarthritic knee. Osteoarthr Cartil 12:997–1005
Chang G, Pakin SK, Schweitzer ME, Saha PK, Regatte RR (2008) Adaptations in trabecular bone microarchitecture in Olympic athletes determined by 7T MRI. J Magn Reson Imaging 27:1089–1095
Krug R, Carballido-Gamio J, Banerjee S et al (2007) In vivo bone and cartilage MRI using fully-balanced steady-state free-precession at 7 Tesla. Magn Reson Med 58:1294–1298
Regatte RR, Schweitzer ME (2007) Ultra-high-field MRI of the musculoskeletal system at 7.0T. J Magn Reson Imaging 25:262–269
Krug R, Stehling C, Kelley DA, Majumdar S, Link TM (2009) Imaging of the musculoskeletal system in vivo using ultra-high field magnetic resonance at 7 T. Invest Radiol 44:613–618
Wright SM, Wald LL (1997) Theory and application of array coils in MR spectroscopy. NMR Biomed 10:394–410
Chang G, Wiggins GC, Xia D et al (2012) Comparison of a 28-channel receive array coil and quadrature volume coil for morphologic imaging and T2 mapping of knee cartilage at 7T. J Magn Reson Imaging 35:441–448
Wehrli FW, Gomberg BR, Saha PK, Song HK, Hwang SN, Snyder PJ (2001) Digital topological analysis of in vivo magnetic resonance microimages of trabecular bone reveals structural implications of osteoporosis. J Bone Miner Res 16:1520–1531
Nelson HD, Helfand M, Woolf SH, Allan JD (2002) Screening for postmenopausal osteoporosis: a review of the evidence for the US Preventive Services Task Force. Ann Intern Med 137:529–541
Conflict of interest
The authors acknowledge grant support from the United States National Institutes of Health: NIAMS/NIH K23-AR059748, NIAMS/NIH RO1-AR053133, NIAMS/NIH RO1-AR056260, NIAMS/NIH RO1-AR060238. Otherwise, the authors have no financial disclosures or conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Chang, G., Honig, S., Liu, Y. et al. 7 Tesla MRI of bone microarchitecture discriminates between women without and with fragility fractures who do not differ by bone mineral density. J Bone Miner Metab 33, 285–293 (2015). https://doi.org/10.1007/s00774-014-0588-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-014-0588-4